Review Article
TMD and pregnancy?

Afa Bayramova*
Obstetrician, Department of Gynecology, Russia*Address for Correspondence: Afa Bayramova MD, Obstetrician, Department of Gynecology, Russia, Email: [email protected]
Dates: Submitted: 01 March 2018; Approved: 13 March 2018; Published: 14 March 2018
How to cite this article: Bayramova A. TMD and pregnancy? Clin J Obstet Gynecol. 2018; 1: 001-006. DOI: 10.29328/journal.cjog.1001001
Copyright License: © 2018 Bayramova A. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Pregnancy; TMD; TMJ; Orthodontics; Dentistry; Obstetrics
Abstract
Pregnancy is a happy stage in life of every woman, but at the same time it is a rather difficult period, since pregnancy represents a serious strain on the body. In the body of a woman during this period there are significant physiological changes that ensure the correct development of the fetus, prepare the body for the upcoming delivery. In this difficult period, the burden on all organs and systems of the woman’s body is significantly increased. Especially often suffer joints; there is a risk of permanent pain, the development of diseases or exacerbation of existing diseases. One of the most common problems is Temporomandibular Dysfunction or Disorder (TMD) which many women face, but still hasn’t been explained.
Review
Often the term TMJ is being used instead of TMD. In actuality, using the phrase “You have TMJ” is inaccurate. TMJ is neither a disease nor syndrome. It is the joint in front of your ear that allows the jaw to move.
TMJ=Temporomandibular Joint
TMD=Temporomandibular Dysfunction or Disorder
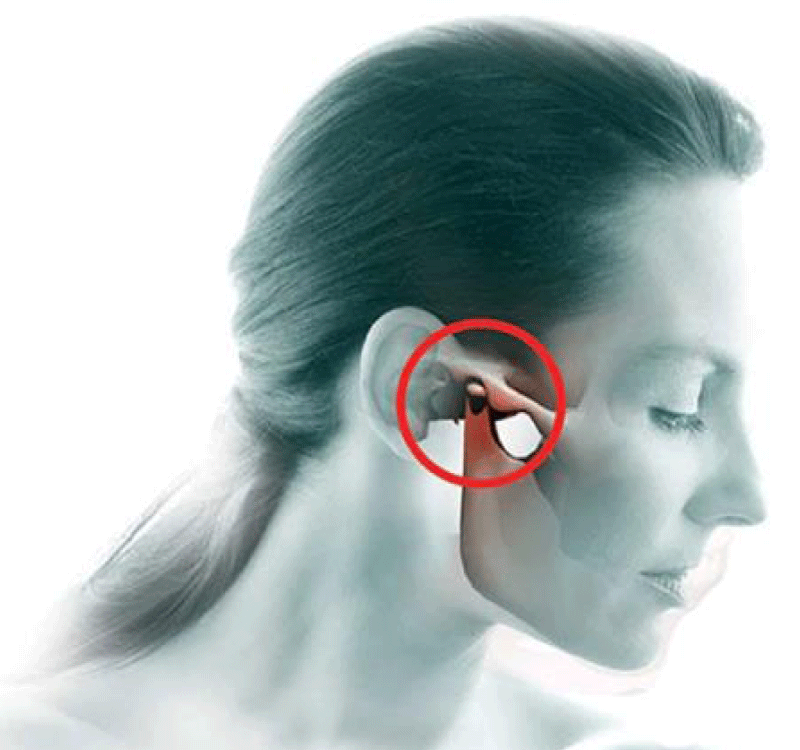
The temporomandibular joint (TMJ) is formed by the articulation of the mandible and the temporal bone of the cranium. It is located anteriorly to the tragus of the ear, on the lateral aspect of the face. The temporomandibular joint (TMJ) acts like a sliding hinge, connecting your jawbone to your skull. You have one joint on each side of your jaw [1]. TMJ disorders-a type of temporomandibular disorder or TMD-can cause pain in your jaw joint and in the muscles that control jaw movement (Figure 1).
TMD is a failure of coordinated joint activity due to impaired occlusion of teeth, the location of the TMJ and muscle function. Occurs in 25-30% of the population, in women 3-5 times more often than men. The peak incidence falls on the age of 20-40 years which is the reproductive period for women. The pathophysiology of TMD is the pathology of the joint itself (especially the displacement of the disc) and the pathology of the masticatory muscles surrounding the joint. Predisposing factors are congenital dysplasia, inflammatory diseases of the joints (osteoarthritis, rheumatoid arthritis, degenerative changes, including damage to the intraarticular disc), congenital and acquired defects of teeth and bite, the influence of sex hormones [2]. Provoking factors can be manipulations accompanied by joint stretching (for example, prolonged opening of the mouth related to the dental procedures), pathological habits (for example, gnawing a pencil); injuries of the jaw; overstrain of muscles when chewing hard food, stress; bruxism, sleeping on the stomach etc [3].
Schiffman et al., put forward diagnostic criteria for headaches secondary to TMD, a large OPPERA study conducted in the United States, confirmed the complex genesis of TMD, beyond the scope of local facial pain [4].
Temporomandibular disorder: Do you have TMJ?
In order to open and close your mouth to eat or speak, your TM Joints must be functioning properly. We all have two TM Joints, one on the right and one on the left. These joints, which are moved by muscles and stabilized by ligaments, are therefore part of an orthopaedic system, which can be compromised by overuse, disease, or trauma. Once present, a TMD problem is typically associated with pain and/or limitation of jaw function [5]. Since the face and mouth are so highly personal, a TMD problem can lead to significant levels of concern and suffering. When the TM complex is compromised, there is the potential for a wide variety of symptoms. Because a Temporomandibular Disorder can give rise to so many variable symptoms, making a proper diagnosis is rather difficult [6].
The symptoms classically associated with Temporomandibular Dysfunction (TMD) include
• Limitation of jaw range of motion
• Painful jaw range of motion
• TM joint clicking
• TM joint locking
• A sense of a bite discrepancy
• Tension in the face
• Daily headaches in the temples
• Morning headaches on arising
• Sore jaw muscles
• Jaw pain while eating
• Neck Tension
In addition, ear symptoms are rather common when a Temporomandibular Disorder is present. Ear symptoms can include pain, a sensation of stuffiness or fullness, and a variety of odd sounds such as ringing, humming, buzzing, and whistling. Other less frequent symptoms include:
• Loss of balance and a sense of unsteadiness
• Tingling sensations in the face and jaw
• Some of these symptoms are directly related to the muscles of the face and/or TMJoint while others have their origins in the upper neck region.
The Temporomandibular Joint apparatus does not stand by itself, but is rather part of a highly balanced orthopaedic system including the head, neck, and shoulder regions. Problems in the upper neck and shoulder region can produce Temporomandibular Dysfunction. Less frequently TMJ problems can lead to neck and shoulder pain and/or dysfunction [7]. The Temporomandibular region is often overlooked during examinations for facial pain, unless conducted by a dentist/dental specialist, and/or oral surgeon. The majority of medical schools do not spend a great deal of time educating their students with regard to the temporomandibular apparatus, and therefore this is an area that is often passed over.
Why do TMJ problems get worse during pregnancy? There are few reasons
Pregnancy produces dramatic changes in levels of estrogens and progesterone. Both estrogen and progesterone levels rise throughout pregnancy. Estrogens are known to increase joint laxity, at least during pregnancy, and laxity of the TMJ is thought to play a role in the development of some of these disorders. Another possibility is that estrogens enhance a number of specific inflammatory responses in the TMJ.
Sleep disruption
Most women discover pretty early on in pregnancy that their favourite position is no longer comfortable. In many cases, she can’t even find one sleep position that’s comfortable. Add to being uncomfortable, the frequent need to get up to urinate during the night and you have a situation that wreaks havoc on the sleep cycle. Disrupted sleep and brain arousals during the night seem to increase the likelihood of tooth grinding and clenching. Therefore, the pregnant woman that experienced jaw problems in the past is certainly now at risk again. The result is the typical list of TMJ problems: pain, jaw stiffness, morning headaches and jaw clicking and/or locking [8].
Morning sickness
For many women unrelenting nausea and frequent vomiting characterize the early stages of pregnancy. Vomiting itself puts extreme pressure on the shoulder and neck muscles and causes the jaw to be violently thrust forward. Frequent vomiting can cause the jaw ligaments to be sprained and the jaw muscles to be strained. A traumatized jaw joint can be painful, stiff, and mechanically challenged. Although morning sickness usually lasts only a short time, that can be just long enough for TMJ problems to start or to reoccur.
The relaxin hormone
Relaxin is a very helpful hormone. It helps ligaments in the pelvis stretchier to accommodate the delivery of a baby. The ligaments become more “lax”. During the later stages of pregnancy relaxin becomes more and more elevated in the bloodstream. While relaxin’s main job is to prepare the pelvis, it also can make the ligaments in other parts of the body more elastic, including the jaw.Here’s a frightening scenario that is experience by many pregnant women: A visit to the dentist for a routine cleaning becomes a nightmare when her jaw gets stuck in the open position. Hello relaxin! Relaxin has made the jaw ligaments unstable and allowed the joint to open wider than normal. Sometimes assistance is even needed to get the jaw closed and that can result in pain and soreness for days, or even weeks. The fear of this scary event happening again is very stressful [9]. As the levels of relaxin and estrogen increases throughout pregnancy, laxity of the temporomandibular joint may increase and there may be a tendency to TMD.
Swelling during pregnancy is due to the extra fluid and blood produced by the body. Fluid levels can double, which is the body’s way to soften the skin so that it can expand as the baby develops. Swelling typically begins after week 20 and can escalate through the coming weeks until the birth. If edema occurs on the neck and face, which happens to some but not all women, the amount of pressure on the jaw and around the TMJ may increase. The result can be TMJ pain. If you’re pregnant, have had TMJ problems in the past, and suspect that they are beginning to resurface, see your dentist before it gets worse. A custom-fitted night guard, a routine of jaw exercises, and some general relaxation techniques may just be what you need to relieve the symptoms and allow you enjoy the rest of your pregnancy [10].
Though many Temporomandibular Disorder problems are self-limited, others produce major disruption of one’s life with pain and suffering continuing over long periods of time. Once a diagnosis of Temporomandibular Dysfunction has been made, treatment options can likely include; education, medication, dietary modification, habit breaking strategies, jaw and neck exercises, muscle injections, oral bite plates, physiotherapy, and tension relieving activities. At times, if there is significant anatomic disruption within the TM Joints, Temporomandibular Surgery consultation may be advised.
What is TMJ treatment?
TMJ problems are orthopaedic in nature and are the result of tired, tight, injured or sore muscles, inflamed tendons, or compromised ligaments, bone and cartilage. As a result, TMJ treatment options are similar to those offered by an Orthopaedist when managing a knee problem, for instance. The first step in TMJ treatment, of course, is to try to prevent further injury by avoiding certain foods (bagels, tough crusty breads, tough meats, uncut apples), and controlling any daytime behaviors that put strain on the jaw muscles or TMJ’s. These activities include [11]:
• Gum chewing
• Nail and cuticle biting
• Biting on pen caps, straws, plastic items
• Teeth clenching
• Biting on your lips or cheeks
• Wide or frequent yawns
• Holding your glasses between your teeth
• Leaning your chin into your hands while at work, on the computer, or watching TV
• Phone cradling
• Ice chewing
What are the TMJ treatment options?
At times, compromise of the TMJoint and jaw muscles will require the use of an oral appliance (bite plate), which can be compared to a knee brace. These devices have different shapes and forms, can be made of variable materials and have different goals. Most importantly, they cushion the TMJs and diminish tightness in the jaw muscles [12]. Over-The-Counter oral appliances sold in pharmacies can at times be used to protect the teeth over the short term, but remember, they are not designed to manage a jaw problem over the long term! If you’re pregnant, have had TMJ problems in the past, and suspect that they are beginning to resurface, see your dentist before it gets worse. A custom-fitted night guard, a routine of jaw exercises, and some general relaxation techniques may just be what you need to relieve the symptoms and allow you enjoy the rest of your pregnancy [13,14].
More TMJ treatment options
• Jaw exercises and physical therapy
• Medications (oral, topical, injectable)
• Massage
• Acupuncture
• Botox injections in the jaw muscles
• Trigger point injections for pain and muscle tension in the jaw and neck muscles
• Behavior Modification strategies
• Breathing techniques
On occasion is there is a need to move teeth or do other dental work to manage a jaw related problem. In some instances, changing the way teeth come together, or providing dental care to improve the efficiency of the chewing surfaces of the teeth may help jaw related problems [15].
Conclusion
Whenever pain problems are confronted, knowing the person attached to those symptoms is critical and will determine which treatments are chosen, how they are sequenced and when they are changed or modified in the pursuit of the best possible outcome.
References
- Yule PL, Durham J, Wassell RW. Pain Part 6: Temporomandibular Disorders. Dent Update. 2016; 43: 39-42. Ref.: https://goo.gl/zWc56B
- Tallents RH, Katzberg RW, Murphy W, Proskin. Magnetic resonance imaging findings in asymptomatic volunteers and symptomatic patients with temporomandibular disorders. J Prosthet Dent. 1996. 75: 529-533. Ref.: https://goo.gl/u3jSKr
- Uyanik JM, Murphy E. Evaluation and management of TMDs, Part 1. History, epidemiology, classification, anatomy, and patient evaluation. Dent Today. 2003; 22: 140-145. Ref.: https://goo.gl/hRdekM
- [Guideline] American Society of Temporomandibular Joint Surgeons. Guidelines for diagnosis and management of disorders involving the temporomandibular joint and related musculoskeletal structures. Cranio. <2003; 21: 68-76.
- Sanders AE, Maixner W, Nackley AG, Diatchenko L, By K, et al. Excess risk of temporomandibular disorder associated with cigarette smoking in young adults. J Pain. 2012; 13: 21-23. Ref.: https://goo.gl/JCwM9T
- Frid P, Nordal E, Bovis F, Giancane G, Larheim TA, et al. Temporomandibular Joint Involvement in Association With Quality of Life, Disability, and High Disease Activity in Juvenile Idiopathic Arthritis. Arthritis Care Res (Hoboken). 2017; 69: 677-686. Ref.: https://goo.gl/C89cUV
- Hegde V. A review of the disorders of the temporomandibular joint. J Indian Prosthodont Soc. 2005. 5: 56-61. Ref.: https://goo.gl/98f5F8
- Rammelsberg P, LeResche L, Dworkin S. Longitudinal outcome of temporomandibular disorders: a 5-year epidemiologic study of muscle disorders defined by research diagnostic criteria for temporomandibular disorders. J Orofac Pain. 2003. 17: 9-20. Ref.: https://goo.gl/TAkvTv
- Fricton JR, Look JO, Schiffman E, Swift J. Long-term study of temporomandibular joint surgery with alloplastic implants compared with nonimplant surgery and nonsurgical rehabilitation for painful temporomandibular joint disc displacement. J Oral Maxillofac Surg. 2002; 60: 1400-1411. Ref.: https://goo.gl/BUAkcG
- Ahn SJ, Kim TW, Lee DY. Evaluation of internal derangement of the temporomandibular joint by panoramic radiographs compared with magnetic resonance imaging. Am J Orthod Dentofacial Orthop. 2006; 129: 479-485. Ref.: https://goo.gl/Ud8UF6
- American Academy of Family Physicians. Temporomandibular join (TMJ) pain. Am Fm Physician. 2007; 76: 1483-1484.
- Briceño F, Ayala R, Delgado K, Piñango S. Evaluation of temporomandibular joint total replacement with alloplastic prosthesis: observational study of 27 patients. Craniomaxillofac Trauma Reconstr. 2013; 6: 171-178. Ref.: https://goo.gl/RkxFfb
- Venezian GC, da Silva MA, Mazzetto RG, Mazzetto MO. Low level laser effects on pain to palpation and electromyographic activity in TMD patients: a double-blind, randomized, placebo-controlled study. Cranio. 2010; 28: 84-91. Ref.: https://goo.gl/8nVhjY
- Silva PA, Lopes MT, Freire FS. A prospective study of 138 arthroscopies of the temporomandibular joint. Braz J Otorhinolaryngol. 2015; 81: 352-357. Ref.: https://goo.gl/GWBAHT
- Felix VB, Cabral DR, de Almeida AB, Soares ED, de Moraes Fernandes KJ. Ankylosis of the Temporomandibular Joint and Reconstruction with a Costochondral Graft in a Patient with Juvenile Idiopathic Arthritis. J Craniofac Surg. 2017; 28: 203-206. Ref.: https://goo.gl/kEtDvn