More Information
Submitted: October 23, 2025 | Approved: October 28, 2025 | Published: October 29, 2025
How to cite this article: Thorat SN, Ravooru A. Peripartum Cardiomyopathy: Early Diagnosis and Management in Secondary Care Hospital. Clin J Obstet Gynecol. 2025; 8(4): 082-084. Available from:
https://dx.doi.org/10.29328/journal.cjog.1001194
DOI: 10.29328/journal.cjog.1001194
Copyright license: © 2025 Thorat SN, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Cardiomyopathy; Peri-partum cardiomyopathy; Echocardiography; Heart failure
Peripartum Cardiomyopathy: Early Diagnosis and Management in Secondary Care Hospital
Sukanya Nagsen Thorat* and Abhyudai Ravooru
Department of Obstetrics & Gynaecology, Tata Main Hospital, West Bokaro Division, Jharkhand, India
*Address for Correspondence: Dr. Sukanya Nagsen Thorat, Department of Obstetrics & Gynaecology, Tata Main Hospital, West Bokaro Division, Jharkhand, India, Email: [email protected]
Background: We report a case of Peri-Partum Cardiomyopathy in a 28-year-old Primigravida, who came in labor and underwent a Caesarean Section in view of meconium-stained liquor, fetal distress. On day 4 post-partum, she complained of a sudden onset of shortness of breath, cough, and restlessness in the morning. The patient had no prior history of heart disease or respiratory disease. Patient developed sudden onset tachypnoea and tachycardia with bilateral crepitus. On further evaluation, she was diagnosed with Peripartum Cardiomyopathy.
Results: The case was successfully managed by a multi-disciplinary team using dobutamine, diuretics, and Angiotensin receptor blockers.
Conclusion: The case report aims to present a case of Peripartum cardiomyopathy with early diagnosis and successful management in a secondary care level hospital. Peripartum (postpartum) cardiomyopathy is the most common cardiomyopathy in pregnancy, defined as an idiopathic cardiomyopathy that presents with heart failure secondary to left ventricular systolic dysfunction toward the end of pregnancy or after delivery, in the absence of any other cause of heart failure. It is a diagnosis of exclusion, and the majority are diagnosed postpartum. Although the LV may not be dilated, the ejection fraction is nearly always reduced below 45%. Incidence of PPCM is 1:3000 to 1:15000 pregnancies. It is a major cause of morbidity and mortality if diagnosis gets delayed; therefore, early diagnosis and timely management can affect patients’ long-term prognosis. This case report aims to raise awareness in health professionals about the possibilities of PPCM and its symptoms, as in our case.
Peripartum cardiomyopathy develops during the last trimester or within the first 6 months after pregnancy. Risk factors are increased maternal age, increased parity, twin pregnancy [1], malnutrition, use of tocolytic therapy for premature labor, and preeclampsia or toxemia of pregnancy. Several of these risk factors contribute to anti-angiogenic signalling through secreted vascular endothelial growth factor (VEGF) inhibitors, such as soluble FLT1 (sFLT1).
As increased circulatory demand of pregnancy aggravates other cardiac diseases, clinically unrecognized, it is crucial to the diagnosis of PPCM that there be no evidence for a pre-existing cardiac disorder. In familial and sporadic DCM, truncating mutations, predominantly in TTN, are present in 15% patients with PPCM and are associated with systolic dysfunction that persists. Pregnancy may represent another example of environmental triggers for accelerated phenotypic expression of genetic cardiomyopathies [2]. Asian countries exhibit varying rates, with Japan reporting a lower incidence than other parts of Asia. Additionally, countries like Haiti and Nigeria report cases from one in 300 and one in 100 live births, respectively [3].
PPCM is more common in women older than 30 years, black women, multiparous women, women with preeclampsia or hypertension, and those who smoke or are malnourished [4]. The overlap between PPCM and preeclampsia is clinically important, as patients with preeclampsia can present with noncardiogenic edema, and the coexistence of these two conditions highlights potential shared pathogenic mechanisms.
Diagnosis of PPCM has four criteria [2,5]:
- Development of cardiac failure in the last 4 weeks of pregnancy or within 5 months post-partum.
- No identifiable cause of cardiac failure.
- No recognizable heart disease before the last 4 weeks of pregnancy.
- Left ventricular dysfunction (ejection fraction < 45%).
A 28-year-old Primigravida was admitted to our labour room at Tata Central Hospital, West Bokaro, on 9/12/2022 at 12:30 am as a case of 40 weeks with a singleton pregnancy in labour with no other comorbidities. Her medical and past history were otherwise unremarkable. She denied any history of pre-existing heart disease, any allergy, or autoimmune diseases. Her menstrual history was normal, and she was taking her hematinic supplementation regularly.
At the time of admission, her pulse was 102 beats/min, and her blood pressure was 110/70 mmHg. Her investigations, LFT, KFT, and complete blood count, were within normal limits. On admission, haemoglobin was 10 g/L, total leucocyte count was 10,900, and platelets were 1.7 lakh. Prothrombin time was 14, and INR was 1.0.
She underwent a lower segment caesarean section on 10th December 2022 at 12 pm for meconium-stained liquor and delivered a healthy male baby of 3.120 kg. Her intraoperative period was uneventful. In the immediate post-partum period uterus was Atonic even after administration of oxytocin drip, hence Inj. Carboprost 250 mcg intramuscular stat was administered. The uterus was well contracted later, and no other intervention was required. Rest immediate postoperative period was uneventful.
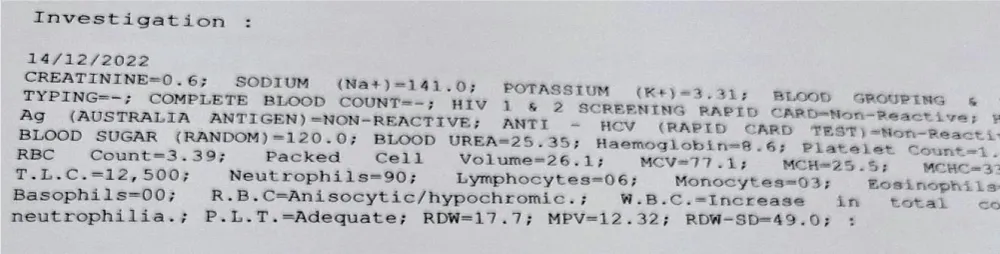
On the 4th postoperative day, the patient complained of a sudden onset of breathlessness and discomfort. On examination, she had developed tachycardia with a pulse rate of 110 beats/min, was afebrile, respiratory rate was 47 breaths per minute with respiratory distress, oxygen saturation was 74% on room air, improved to 80% with nasal oxygen, chest was full of coarse crepitations with fine basal crepitations. Her chest x-ray showed cardiomegaly with bilateral pulmonary infiltrates. Urine albumin was nil on dipstick examination (Figure 1).
Figure 1: Investigations on post-partum day 6.
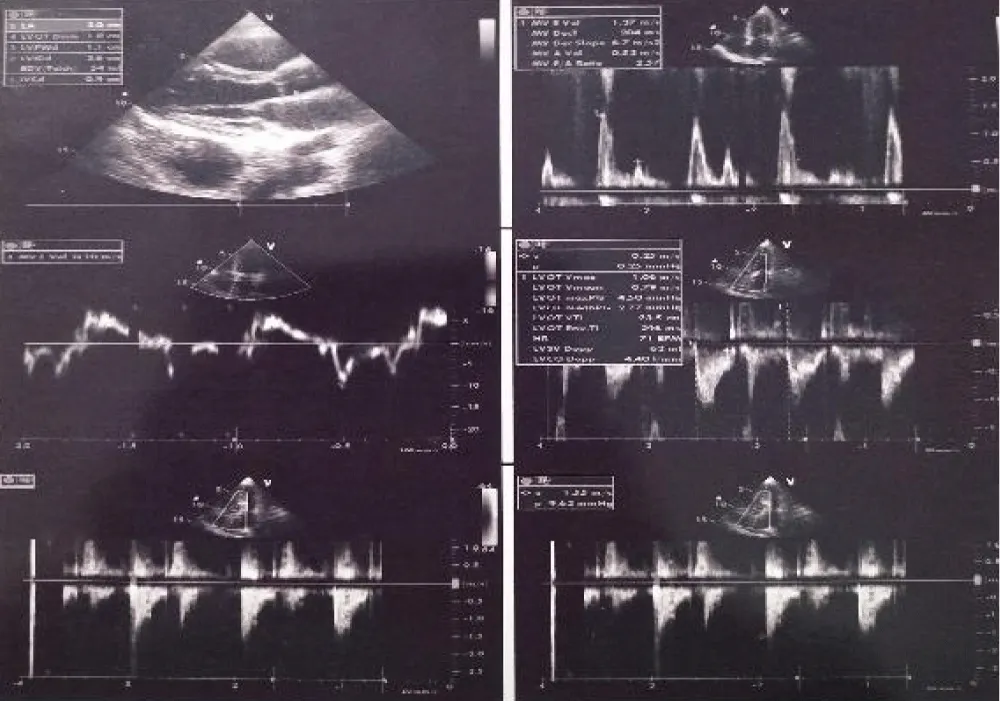
The echocardiograph showed pathognomonic changes identifiable with peripartum cardiomyopathy. She was immediately shifted to the intensive care unit and was managed conservatively with oxygenation, propped up positioning, intravenous furosemide, and hydrocortisone. Mechanical ventilation was not required. The patient was stabilised and oxygen saturation improved to 95% and referred to a higher centre for cardiologist opinion and further management.
2D Echo showed normal size left ventricular function, Ejection fraction of 50%, mild mitral regurgitation, mild tricuspid regurgitation, PG: 26 mmHg, Central venous pressure: 8 cm, PASP: 34 mmHg, no mitral stenosis, no intracardiac lesions or pericardial effusions. The final diagnosis of Post Partum Cardiomyopathy was made by the cardiologist, and the patient was started on dobutamine therapy. The patient improved with treatment and was discharged after 3 days in a hemodynamically stable condition. Patient was advised oral digoxin and oral diuretics at discharge. The patient was managed by a multidisciplinary team approach of obstetricians, physicians, and cardiologists.
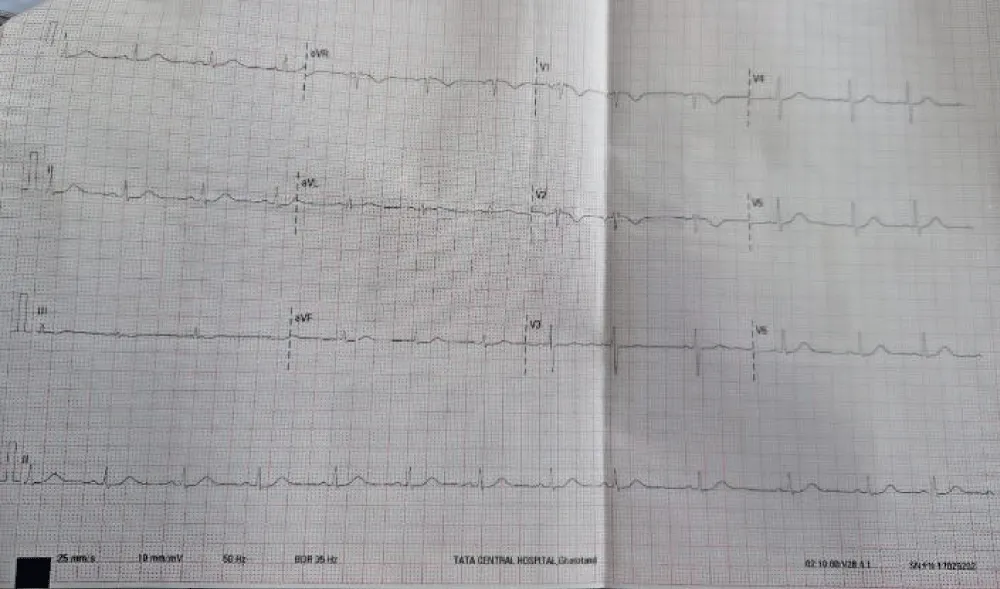
On follow-up after 2 weeks patient was asymptomatic. The patient and her family were counselled about the prognosis and recurrence of the disease in the next pregnancy, and options of contraception were discussed (Figures 2,3).
Figure 2: 2D-Echocardiography of the patient on postpartum day 4.
Figure 3: Electrocardiogram on postpartum day 4.
Since breathlessness and discomfort a common findings in even normal pregnancy and post-partum period, PPCM doesn’t strike as an obvious differential diagnosis. But a careful look at the pulse rate, saturation levels, and auscultatory lung findings can help in early diagnosis and treatment of a condition where morbidity and mortality can be saved easily. Decisions regarding the timing of delivery in PPCM should be individualized based on maternal and fetal factors, including the severity of cardiac dysfunction, gestational age, and overall clinical stability. While expedited delivery may be necessary in critical cases to improve maternal outcomes, it should be balanced with the risks of prematurity for the foetus [6].
Early post-partum diagnosis is independently associated with higher baseline Left Ventricular function, which may represent the mechanism by which early diagnosis leads to a favourable outcome. Obstetricians must know what PPCM is and how to diagnose this condition early so that prompt intervention can be done and the patients’ lives can be saved in this rare but easily diagnosed condition.
All images and all information in this case report are reported under explicit informed consent of the patient: patient anonymity has been preserved in accordance with the Declaration of Helsinki.
- Schaufelberger M. Cardiomyopathy and pregnancy. Heart. 2019;105(14):1112-1118.
- Demakis JG, Rahimtoola SH, Sutton GC, Meadows WR, Szanto PB, Tobin JR Jr, et al. Natural course of peripartum cardiomyopathy. Circulation. 1971 Dec;44(6):1053-1061. Available from: https://doi.org/10.1161/01.cir.44.6.1053
- Safira A, Tjahjadi AK, Adytia GJ, Waitupu A, Sutanto H. Peripartum cardiomyopathy unveiled: aetiology, diagnosis, and therapeutic insights. Curr Probl Cardiol. 2024;49(5):102474. Available from: https://doi.org/10.1016/j.cpcardiol.2024.102474
- Regitz-Zagrosek V, Roos-Hesselink JW, Bauersachs J, Blomström-Lundqvist C, Cífková R, De Bonis M, et al. ESC Scientific Document Group. 2018 ESC Guidelines for the management of cardiovascular diseases during pregnancy. Eur Heart J. 2018;39(34):3165-3241. Available from: https://doi.org/10.1093/eurheartj/ehy340
- Sliwa K, Hilfiker-Kleiner D, Petrie MC, Mebazaa A, Pieske B, Buchmann E, et al. Heart Failure Association of the European Society of Cardiology Working Group on Peripartum Cardiomyopathy. Current state of knowledge on aetiology, diagnosis, management, and therapy of peripartum cardiomyopathy: a position statement from the Heart Failure Association of the European Society of Cardiology Working Group on Peripartum Cardiomyopathy. Eur J Heart Fail. 2010;12(8):767-778. Available from: https://doi.org/10.1093/eurjhf/hfq120
- Rojas DM, Peña DF, González LM. Peripartum cardiomyopathy: a case report of mortality from a rare and potentially fatal condition. Cureus. 2024;15(8):e171-179. Available from: https://doi.org/10.14740/jmc4228