More Information
Submitted: February 15, 2024 | Approved: February 24, 2024 | Published: February 26, 2024
How to cite this article: Gurashi A, Osman A, Suliman H, Eltigani A, Siralkatim I, et al. Second Stage of Labor Cesarean Section Maternal and Fetal Outcomes. Clin J Obstet Gynecol. 2024; 7: 025-033.
DOI: 10.29328/journal.cjog.1001159
Copyright License: © 2024 Gurashi A, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Second stage; Labor; Cesarean section; Maternal; Fetal; Outcome
Abbreviations: AVD: Assisted Vaginal Delivery; BMI: Body Mass Index; CI: Confidence Interval; CPD: Cephalopelvic Disproportion; CS: Cesarean Section; DDI: The decision to Deliver Interval; EFM: Electronic Fetal Heart Rate Monitoring; EWTD: European Working Time Directive; FSB: Fresh Stillbirth; IUFD: Intra-Uterine Fetal Deaths; NICU: Neonatal Intensive Care Unit; OP: Occipito-Posterior; OR: Odds Ratio; OVB: Operative Vaginal Birth; P: Para; PPH: Postpartum Hemorrhage; PV: Prevaginal; RANZOG: Royal Australian and New Zealand College of Obstetricians and Gynecologists; RCOG: Royal College of Obstetricians and Gynecologists; RDS: Respiratory Distress Syndrome; RR: Risk Ratio; SPSS: Statistical Package for Social Science; TTN: Transient Tachypnea of the Newborn; VBAC: Vaginal Birth after Cesarean Section; WHO: World Health Organization
Second Stage of Labor Cesarean Section Maternal and Fetal Outcomes
Ahazeej Gurashi1, Ameer Osman2, Hajar Suliman1, Ayat Eltigani3, Isra Siralkatim3, Hamza Orfali1 and Awadalla Abdelwahid Suliman1*
1Department of Obstetrics & Gynecology, Alneelain University, Khartoum, Sudan
2Department of Obstetrics & Gynecology, Khartoum University, Khartoum, Sudan
3Department of Obstetrics & Gynecology, Sudan Medical Specialization Board, Khartoum, Sudan
*Address for Correspondence: Awadalla Abdelwahid Suliman, Obstetrician & Gynaecologist Consultant, Head of Department of Obstetrics and Gynecology, Faculty of Medicine, Al Neelain University, Khartoum, Sudan, Email: [email protected]
Background: Cesarean section at the second stage of labor occurs when the mother requires delivery with full dilatation of the cervix by cesarean section (CS), which poses a risk to the mother and fetus.
Purpose: To study the maternal and fetal outcomes of second-stage cesarean section.
Methods: This comparative study was conducted at Alhasahisa Teaching Hospital from August 2021 to January 2022. The study sample comprised 226 women who fulfilled the inclusion criteria, including 113 who delivered by second-stage cesarean section and 113 who delivered by first-stage labor cesarean section as controls. Data were collected using a questionnaire filled out by doctors after informed consent was obtained.
Results: The common indications in women who delivered via second-stage cesarean section were fetal distress in 62(51.9%), obstructed labor in 26(23%), and failure to progress in 25(22.1%). In women who underwent first-stage cesarean section, the common indications were failure to progress in 85(75.2%), fetal distress in 16(14.2%), and chorioamnionitis in 12(10.6%) (p < 0.05).
The reported maternal complications in women who underwent second-stage cesarean section were postpartum hemorrhage in 34(30.1%), sepsis in 11(9.7%), prolonged labor in eight (7.1%), extended tears in four (3.5%), umbilical cord prolapse in three (2.7%), and episiotomy in three (2.7%).
The admission to the neonatal intensive care unit (NICU) and the causes of admission were more common among the babies of the women delivered by second-stage cesarean section than the babies of the women delivered by first-stage cesarean section (p value < 0.05).
Maternal complications in women who underwent second-stage cesarean section included postpartum hemorrhage in 34(30.1%), sepsis in 11(9.7%), prolonged labor in 8(7.1%), uterine extension in 4(3.5%), umbilical cord prolapse in 3(2.7%), and episiotomy in 3(2.7%) (p < 0.05).
Conclusion: Second-stage labor cesarean section showed more complications of postpartum hemorrhage, sepsis, and extended tears, as well as more fetal complications, such as admission to the neonatal intensive care unit, fresh stillbirths, low Apgar scores, and birth asphyxia.
Cesarean section (CS) at the second stage of labor occurs when the mother requires delivery at full dilatation by CS and poses a risk to the mother and fetus. The increasing trend of CS in the second stage of labor is a major concern in modern obstetrics [1]. The incidence of CS in the second stage of labor has increased from 0.9% to 2.2%. The second stage of labor CS has been reported to increase with increasing CS rates [2].
The literature review suggests that this trend is multifactorial, probably due to a lack of training for junior staff in the second stage of labor decision-making and a lack of expertise in assisted vaginal delivery. An increase in primary CS has a great impact on subsequent obstetric outcomes and delivery [3,4].
The Royal College of Obstetricians and Gynecologists (RCOG) reported that 6% of primary CS occurs at full dilatation, and in 50% of these patients, instrumental vaginal delivery was not attempted [5].
Cesarean section at full dilatation is technically more challenging than CS in early labor [6]. It is also difficult to deliver a deeply engaged fetal head, which can be delivered by the Patwardhan or push methods [7]. Maternal morbidity is higher in the second stage of labor CS [8]. Maternal morbidity in the second stage of labor CS occurs in the form of extension of the uterine angles, postpartum hemorrhage, and prolonged surgical time [9]. Bladder injury and postpartum pyrexia are common complications reported during the second stage of labor CS [10].
Neonatal morbidity in terms of neonatal intensive care unit (NICU) admissions, fetal academia, hypoxemia, and prolonged NICU stay is reportedly higher in the second stage of labor CS [11].
Decision-making for CS in the second stage of labor is one of the greatest challenges in current obstetric practice. The involvement of a skilled obstetrician in the management of the second stage of labor CS aids in minimizing morbidity and mortality [12]. A previous study in Khartoum found that the second-stage cesarean section rate was 2.4%, and the overall CS rate was 26.9% during the same period [13]. Another study in Eastern Sudan on post-CS blood transfusion found the rate of second-stage CS to be 3.3% [14].
A study in Western Sudan found that second-stage cesarean section was the cause of near-miss women [15]. An Ethiopian study found that second-stage CS had four-fold complications in comparison to women not in labor [16] and found postpartum hemorrhage, uterine tear, atonia, and a greater need for antibiotics in second-stage CS [17-20].
Maternal hemorrhage (>1000 ml) is reported to occur in 4.7%5–10%19 of CS cases at full dilatation [6], a cohort study of 393 women who had undergone either operative vaginal delivery in theatre or CS at full dilatation found that 73% of those who were considering further pregnancy achieved a further pregnancy after 3 years [21], and the psychological impact of either vaginal or abdominal operative delivery in the second stage is likely to be significant and long-lasting [22].
Similarly, the rate of neonatal intracranial hemorrhage was greater following operative vaginal delivery than following CS. This suggests that the delivery itself can be traumatic [23]. Apgar score < at 5 minutes; significant trauma or sepsis) demonstrated low rates of neurodevelopment morbidity at the age of 5 years, irrespective of whether they were delivered by successful instrumental delivery or CS at full dilatation [24].
In a Nepal study, perinatal complications of meconium stain liquor were as follows: 27.77%, NICU admissions, 13.88%, Apgar score <5 at 5 min, 13.55%, NICU admission, 5.54%, and fresh stillbirth, 2.77% [25].
A cesarean section at the second stage of labor poses a risk to the mother and the fetus. The increasing trend of CS at the second stage of labor is of major concern in modern obstetrics compared to CS at the first stage of labor. The incidence of the second stage of labor CS has increased from 0.9% to 2.2%. This may maybe due to a lack of trained and skilled staff in instrumental delivery. The different results in the previous study are explained by the hospital setup.
During our work in Alhasahisa maternity hospital, it was observed that second-stage CS contributes to an appreciable percentage of the emergency c/s, not only that but several serious complications and adverse outcomes were observed attended staff, patients were referred from nearby hospitals that were covered by juniors’ doctors and midwives those patients who needed second stage labor CS with more complications, both fetal and maternal. This study is conducted to explore the causes of this high incidence of second-stage CS, to know how we can reduce the number of second-stage CS and end up with objective results and recommendations that might reduce this drastic scenario.
This comparative study was carried out at the Alhasahisa Teaching Hospital in the Alhasahisa locality, Sudan, from August 2021 to January 2022.
The inclusion criteria for this study were that all women who delivered by first-stage labor cesarean section were selected as the control group, while all women who delivered by second-stage labor cesarean section were selected as the case group, who provided consent to participate in the study and those managed during the study period.
The study excluded women who had given birth vaginally (normal or abnormal), women who had medical disorders, women who had a placental abruption, those outside the study period and setting, those with vaginal birth after cesarean section (VBAC), and those who refused to participate in the study. The study data were collected from all women who delivered via emergency CS in 2nd stage cesarean section cases and all women who delivered via emergency CS in 1st stage of CS.
Data were collected using a pre-designed closed-ended questionnaire filled out by registrars. The independent variables were the demographic characteristics, age, parity, and gravidity. The dependent variables were maternal and fetal outcomes.
Sample size
The size of the study was determined through the following formula:
n = (Z2 × (p×q))/e2
n: sample size required by the study
Z: the determined area under the normal curve by the desired confidence interval (CI:1.96) standard normal deviate
P: The prevalence of C/S is estimated at 2% [12].
Then, P = 0.02
q = 1-p = 1 – 0.02= 0.98
e = the desired precision (e=0.05) because the prevalence is relatively small (less than10%)
n = (1.96) 2 × (0.02x0.98))/0.0025=159.2=112.9=113
The sample size was 226 study participants, 113 cases of second-stage CS, and 113 delivered by first-stage CS.
The sampling technique used simple random sampling methods, collecting the number of women who delivered by the second stage as the case group and those who delivered by the first stage as the comparative group. A total of 113 mothers were enrolled in the study, representing the main study group, and 113 mothers delivered via first-stage cesarean section were selected as the comparative group.
Statistical analysis was performed via SPSS 23 software (SPSS, Chicago, IL, USA).
Descriptive statistics in terms of frequency tables, percentages, and graphs. Descriptive analysis was performed for all study variables with mean and standard deviation for quantitative data, and frequencies with proportions for qualitative data.
Bi-variable analysis to determine the associations between the main outcome variable and the other relevant risk factors using the Chi-square test (for categorical variables) and t-test (quantitative variables) statistical tests and a p - value of 0.05 or less were considered significant.
Data are presented after the analysis in the form of univariable tables, cross-tabulation (bi-variable tables), multivariable tables, figures, and narrative illustrations.
Ethical considerations were considered, and the study was approved by the ethics review committee of the Sudan Medical Specialization Board. Council of Obstetrics and Gynecology. The agreement was obtained from the administrative authorities of the Alhasahisa Hospital. Written consent was obtained from all the participants after explaining the nature and purpose of the study. Confidentiality of participants’ data was considered by coding the questionnaire. The respondents were informed that the study was not associated with experimental or therapeutic intervention and that information was collected from them.
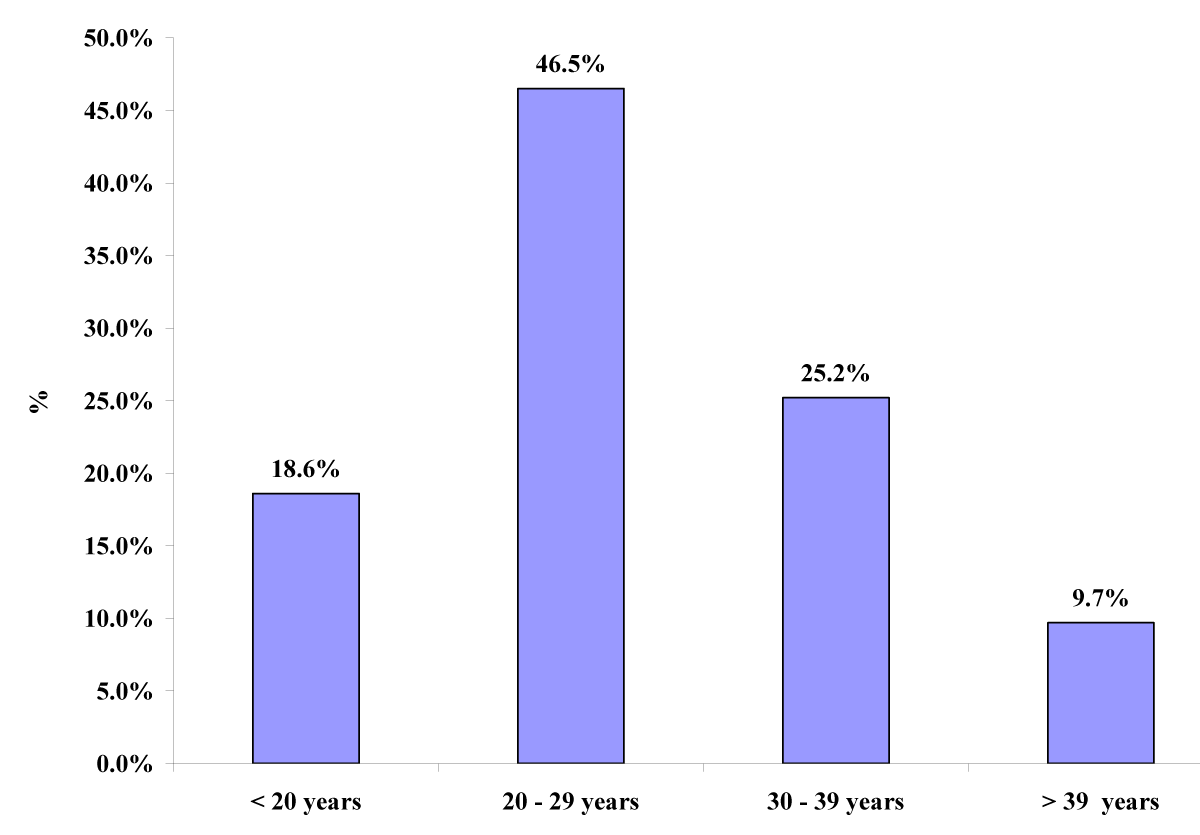
The number of women aged 20 – 29 years was 105(46.5%), between 30 – 39 years 57(25.2%) were between 20 years 42(18.6%) were more than 39 years, and 22(9.7%) (Figure 1).
Figure 1: Age of the women delivered by Second stage CS and first-stage CS (n = 226).
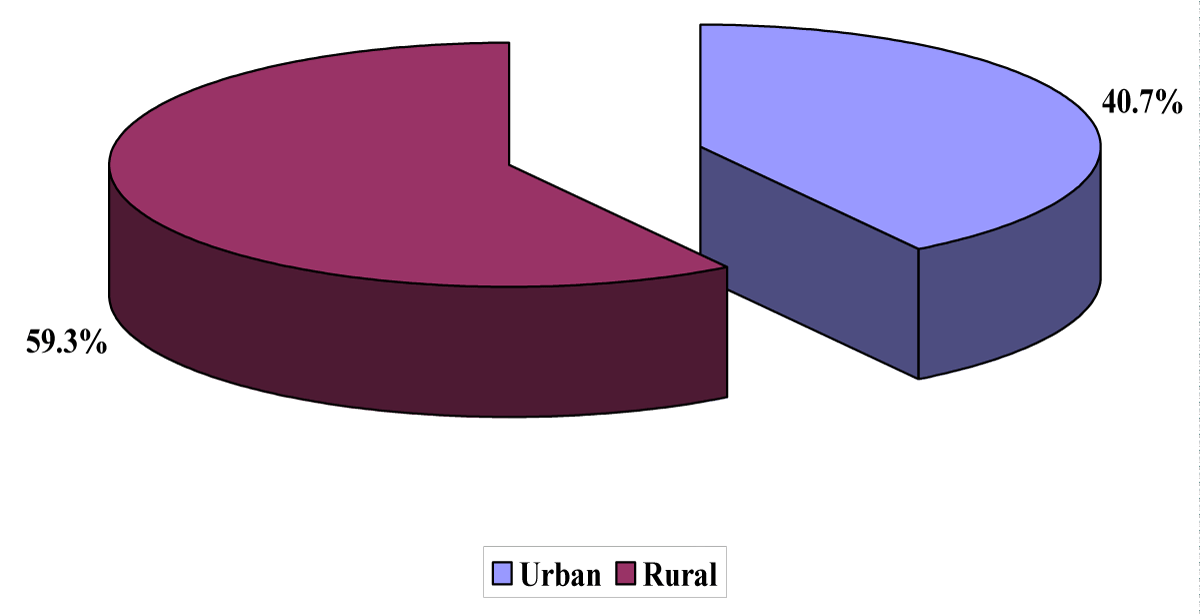
A total of 134(59.3%) women were from rural areas and 92(40.7%) were from urban areas (Figure 2).
Figure 2: Residence of the women delivered by Second stage CS and first-stage CS (n = 226).
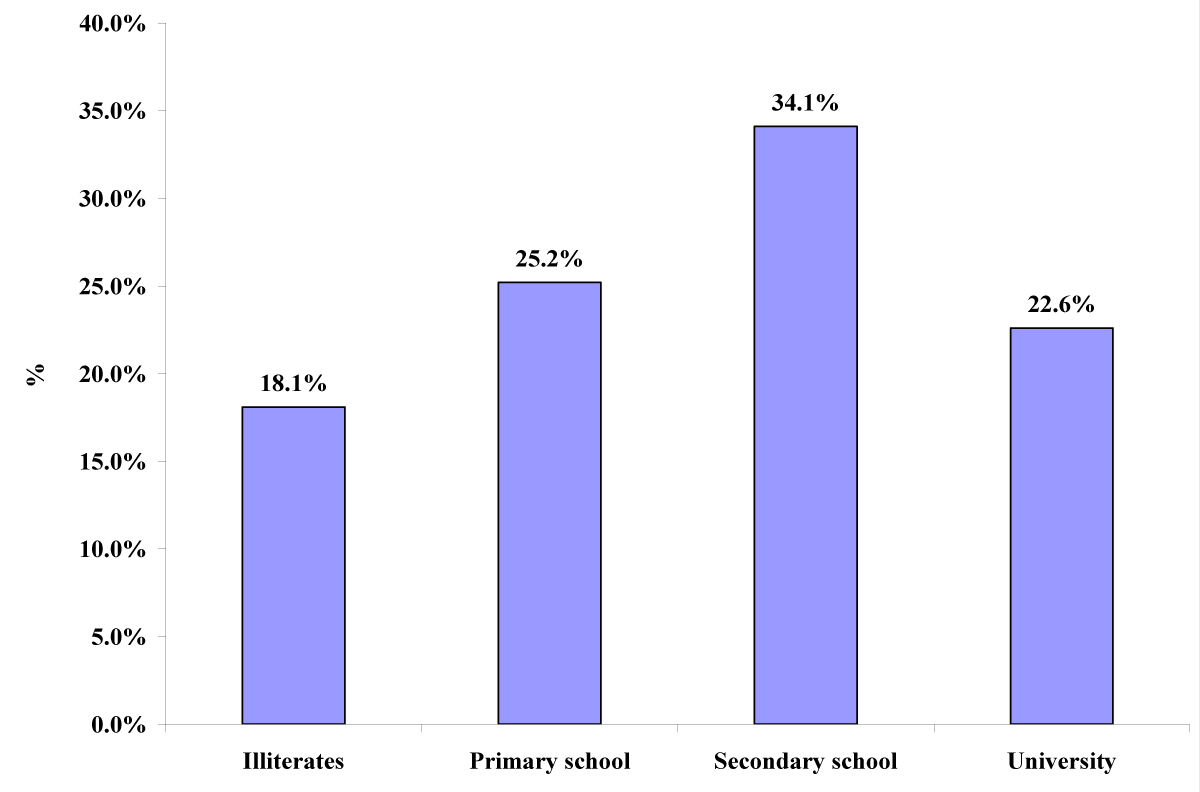
The numbers of women with a secondary level of education were 77(34.1%), 57(25.2%), 51(22.6%), and 41(18.1%), respectively (Figure 3).
Figure 3: Educational level of the women delivered by Second stage CS and first-stage CS (n = 226).
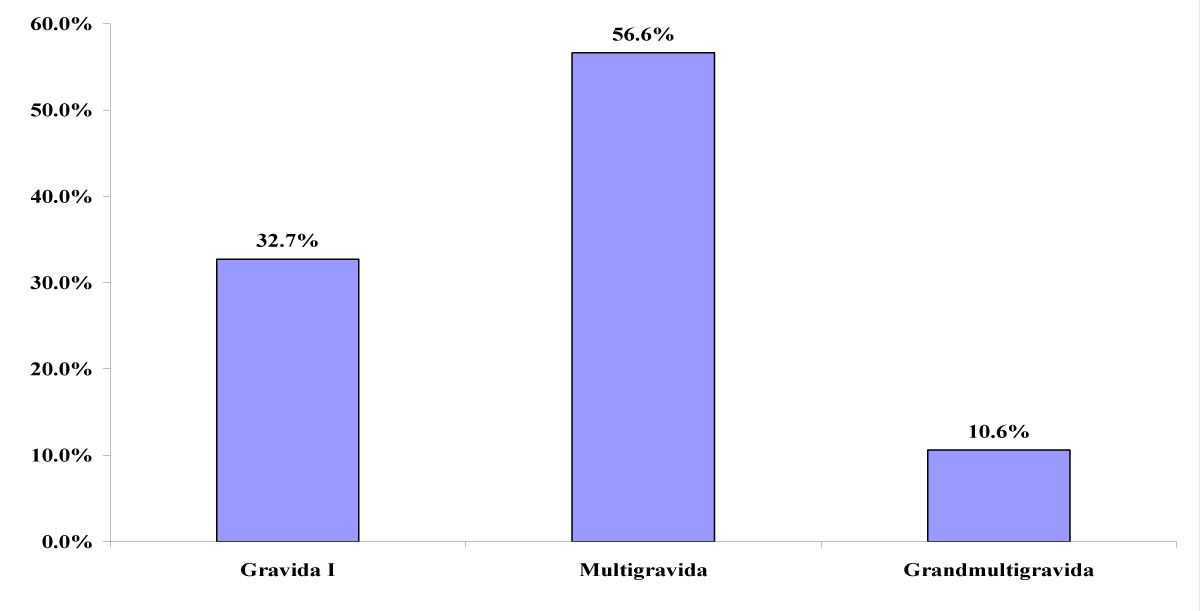
There were 128 (56.6%) multigravidas, 74 (32.7%) gravida I, and 24 (10.6%) grand multigravidas (Figure 4).
Figure 4: Gravidity of the women delivered by Second stage CS (n = 113).
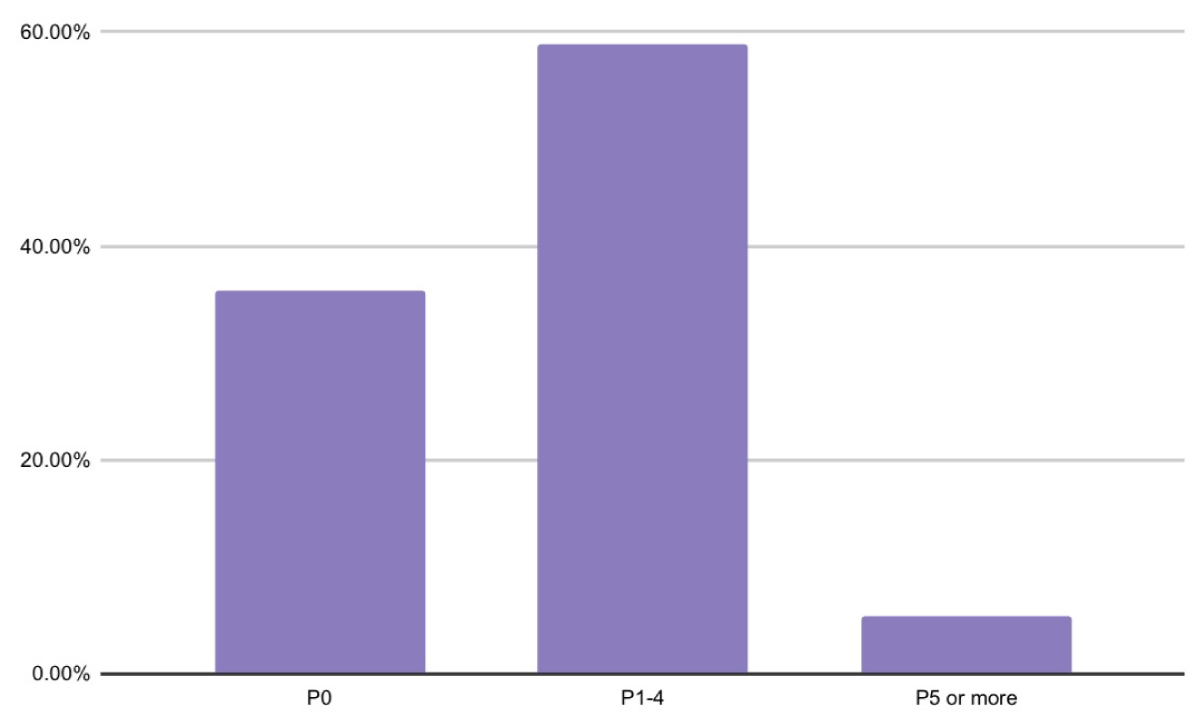
Nulliparous patients comprised 40(35.8%), Para1 (P1) to Para 4 (P4) were 66(58.9%), and 9(5.3%) were para 5 or more (Figure 5).
There were 128(56.6%) multigravidas, 74(32.7%) gravida I, and 24(10.6%) grand multigravidas (Figure 4).
Figure 5: Parity of the women delivered by Second stage CS (n = 113).
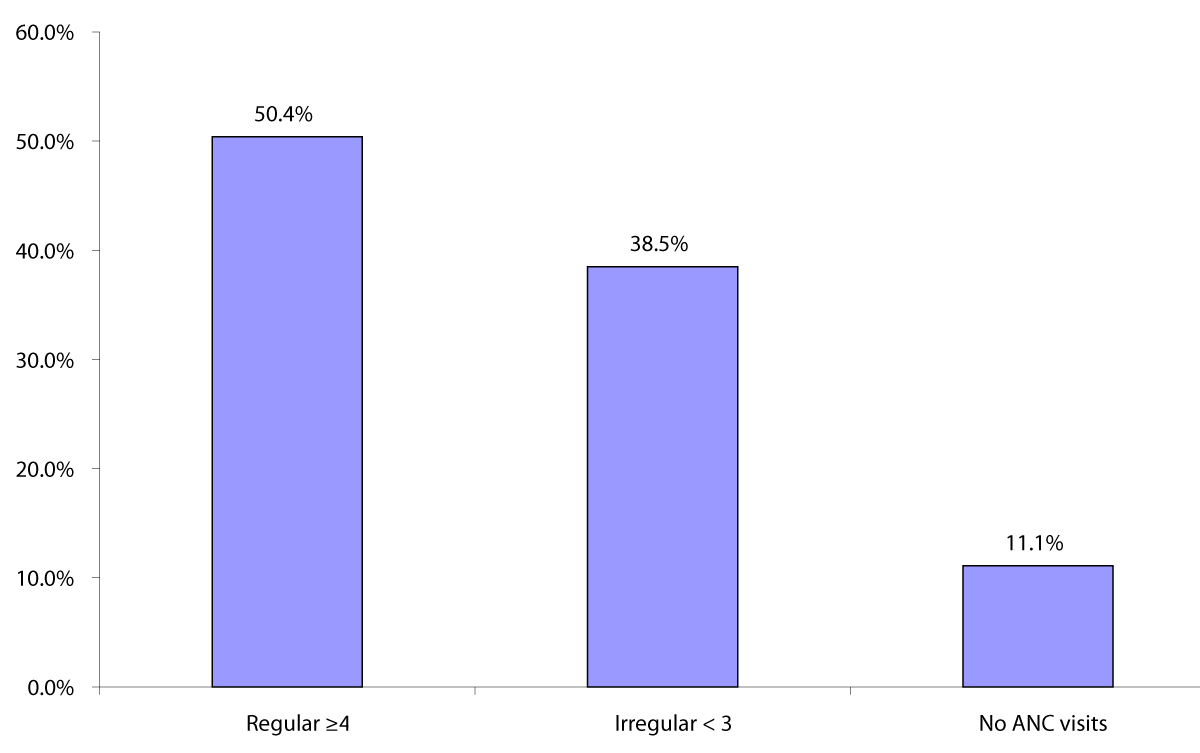
The number of women who attended regular ANC was 114(50.4%), 87(38.5%) were irregular, and 25(11.1%) did not attend (Figure 6).
Figure 6: Number of ANC visits of the women delivered by Second stage CS and first-stage CS (n = 226).
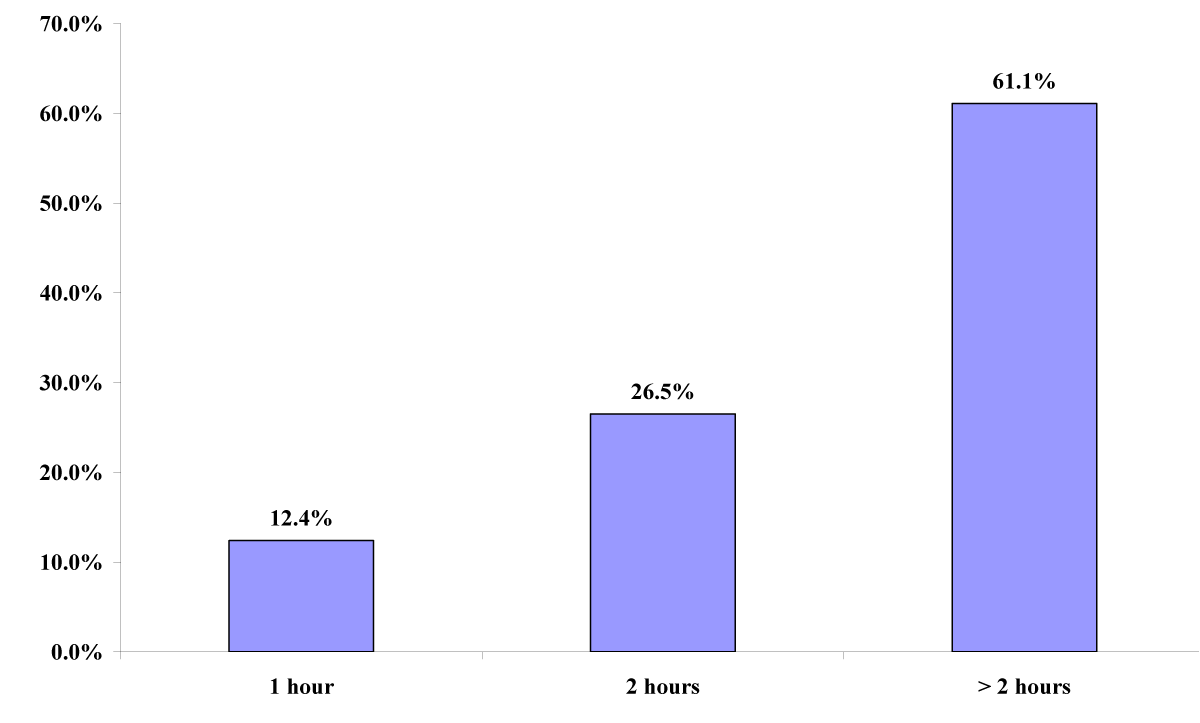
The duration of the second stage of labor was more than 2 h in 69(61.1%), 2 h in 30(26.5%), and 1 h in 14(12.4%) (Figure 7).
Figure 7: Duration of the second stage of labor of the women delivered by Second-stage CS (n = 113).
The common indications for CS in women delivered by second-stage cesarean section were fetal distress 62(54.9%), obstructed labor 26(23%), and failure to progress 25(22.1%). Among the women who delivered by first-stage CS, the common indications were failure to progress in 85(75.2%), fetal distress in 16(14.2%), and chorioamnionitis in 12(10.6%) (p < 0.05) (Table 1).
| Table 1: Indications of CS of the women delivered by Second stage CS VS first stage CS (n = 226). | ||||
| Indications of 2nd stage CS | Type of CS | |||
| Second Stage CS | First stage CS | |||
| N | % | N | % | |
| Failure to progress | 25 | 22.1 | 85 | 75.2 |
| Fetal distress | 62 | 54.9 | 16 | 14.2 |
| Obstructed labour | 26 | 23.0 | 0 | 0.0 |
| Chorioamnionitis | 0 | 0.0 | 12 | 10.6 |
| Total | 113 | 100.0 | 113 | 100.0 |
| p - value = 0.01 | ||||
In maternal assessment, differences were found in prevaginal examination (PV) findings (full dilatation in all women delivered by second-stage CS, station at presentation (-1 and 0 in second-stage CS]) (p < 0.05) (Table 2).
| Table 2: Prevaginal assessment of the women delivered by Second stage CS VS first stage CS (n = 226). | |||||
| PV findings | Type of CS | p - value | |||
| Second Stage CS | First stage CS | ||||
| N | % | N | % | ||
| 10 cm | 113 | 100.0 | 0 | 0.0 | 0.001* |
| 9 cm | 0 | 0.0 | 9 | 8.0 | |
| 8 cm | 0 | 0.0 | 25 | 22.1 | |
| 7 cm | 0 | 0.0 | 30 | 26.5 | |
| 6 cm | 0 | 0.0 | 33 | 29.2 | |
| 5 cm | 0 | 0.0 | 16 | 14.2 | |
| Station of presenting part | |||||
| - 3 | 0 | 0.0 | 31 | 27.4 | 0.023* |
| - 2 | 10 | 8.8 | 28 | 24.8 | |
| - 1 | 43 | 38.1 | 18 | 15.9 | |
| 0 | 38 | 33.6 | 32 | 28.3 | |
| + 1 | 18 | 15.9 | 4 | 3.5 | |
| + 2 | 4 | 3.5 | 0 | 0.0 | |
| Presentation | |||||
| Cephalic | 113 | 100.0 | 113 | 100.0 | 0.99** |
| Total | 113 | 100.0 | 113 | 100.0 | |
| Position | |||||
| DOA | 9 | 8.0 | 8 | 7.1 | 0.98** |
| LOA | 15 | 13.3 | 15 | 13.3 | |
| ROT | 12 | 10.6 | 12 | 10.6 | |
| LOT | 12 | 10.6 | 19 | 16.8 | |
| TOP | 27 | 23.9 | 27 | 23.9 | |
| DOP | 20 | 17.3 | 15 | 13.3 | |
| LOP | 17 | 15.0 | 15 | 13.3 | |
| LSA | 1 | 1.3 | 2 | 1.8 | |
No significant differences were found between women who delivered by first- and second-stage CS in the duration of membrane rupture and pre-emergency CS CTG assessment (p > 0.05) (Tables 3,4).
| Table 3: Duration of ruptured membranes of the women delivered by Second stage CS VS first stage CS (n = 226). | ||||
| Duration of membrane rupture | Type of CS | |||
| Second Stage CS | First stage CS | |||
| N | % | N | % | |
| < 12 hours | 59 | 52.2 | 65 | 57.5 |
| 12 - 24 hours | 44 | 38.9 | 41 | 36.3 |
| > 24 hours | 10 | 8.8 | 7 | 6.2 |
| Total | 113 | 100.0 | 113 | 100.0 |
| p - value = 0.08 | ||||
| Table 4: Pre cesarean section CTG of the women delivered by Second stage CS VS first stage CS (n = 226). | ||||
| Pre EMCS CTG | Type of CS | |||
| Second Stage CS | First stage CS | |||
| N | % | N | % | |
| Reassuring | 37 | 32.7 | 86 | 76.1 |
| Suspicious | 33 | 29.2 | 17 | 15.0 |
| Pathologic | 43 | 38.1 | 10 | 8.8 |
| Total | 113 | 100.0 | 113 | 100.0 |
| p - value = 0.06 | ||||
The significant differences in fetal assessment outcomes between the women delivered by first- and second-stage cesarean sections were lower Apgar scores at 1 and 5 min, abnormal fetal heart rate, and suffering caput and molding among the fetuses of women delivered by second-stage CS than in first-stage CS (p < 0.05) (Table 5). No significant differences were found between the women delivered by first- and second-stage CS in terms of live fetuses and birth weight (p > 0.05), while admission to the neonatal intensive care unit and the causes of admission were more common among the babies of the women delivered by second-stage cesarean section than the babies of the women delivered by first-stage cesarean section (p < 0.05) (Table 6). Among the mothers, no significant differences were found between the groups delivered by the first- and second-stage CS in the vital sign assessments (p > 0.05) (Table 7).
| Table 5: Fetal assessment of the women delivered by Second stage CS VS first stage CS (n = 226). | |||||
| Assessment findings | Type of CS | p - value | |||
| Second Stage CS | First stage CS | ||||
| Baby gender | N | % | N | % | |
| Male | 64 | 56.6 | 59 | 52.2 | 0.071** |
| Female | 49 | 43.4 | 54 | 47.8 | |
| Apgar score at 1 min | |||||
| < 5 | 39 | 34.5 | 3 | 2.7 | 0.016* |
| 5 - 7 | 41 | 36.3 | 11 | 9.7 | |
| > 7 | 33 | 29.2 | 99 | 87.6 | |
| Apgar scored at 5 minutes | |||||
| < 5 | 21 | 18.6 | 3 | 2.7 | 0.019* |
| 5 - 7 | 40 | 35.4 | 11 | 9.7 | |
| > 7 | 52 | 46.0 | 99 | 87.6 | |
| Fetal signs of obstruction | |||||
| Caput | 56 | 49.6 | 10 | 8.8 | 0.015* |
| Molding | 22 | 19.5 | 9 | 8.0 | |
| No | 35 | 31.0 | 94 | 83.2 | |
| Total | 113 | 100.0 | 113 | 100.0 | |
| * Significant difference (p < 0.05); ** No significant difference (p > 0.05). | |||||
| Table 6: Fetal outcomes of the women delivered by second stage CS VS first stage CS (n = 226). | |||||
| Fetal outcomes | Type of CS | p - value | |||
| Second Stage CS | First stage CS | ||||
| N | % | N | % | ||
| Alive | 112 | 99.1 | 112 | 99.1 | 0.061** |
| Stillbirth | 1 | 0.9 | 1 | 0.9 | |
| Total | 113 | 100.0 | 113 | 100.0 | |
| Admission to NICU | |||||
| Yes | 60 | 53.1 | 10 | 8.8 | 0.013* |
| No | 53 | 46.9 | 103 | 91.2 | |
| Total | 113 | 100.0 | 113 | 100.0 | |
| Causes of admission | |||||
| Birth asphyxia | 18 | 30.0 | 3 | 30.0 | 0.022* |
| Meconium aspiration | 24 | 40.0 | 1 | 10.0 | |
| TTN | 5 | 8.3 | 0 | 0.0 | |
| Grunting | 6 | 10.0 | 0 | 0.0 | |
| Observation | 4 | 6.7 | 6 | 60.0 | |
| Signs of sepsis | 3 | 5.0 | 0 | 0.0 | |
| Total | 60 | 100.0 | 10 | 100.0 | |
| Birth weight | |||||
| < 2500 g | 0 | 0.0 | 8 | 7.1 | 0.082** |
| 2500 - 3900 g | 105 | 92.9 | 94 | 83.2 | |
| > 3900 g | 8 | 7.1 | 11 | 9.7 | |
| Total | 113 | 100.0 | 113 | 100.0 | |
| * Significant difference (p < 0.05); ** No significant difference (p > 0.05) | |||||
| Table 7: Maternal vital signs of the women delivered by Second stage CS VS first stage CS (n = 226). | |||||
| Signs | Type of CS | p - value | |||
| Second Stage CS | First stage CS | ||||
| BP | N | % | N | % | |
| NAD | 6 | 5.3 | 0 | 0.0 | 0.063** |
| Low | 20 | 17.7 | 23 | 20.4 | |
| Normal | 87 | 77.0 | 90 | 79.6 | |
| Heart rate | |||||
| NAD | 16 | 14.2 | 7 | 6.2 | 0.065** |
| Low | 2 | 1.8 | 4 | 3.5 | |
| Normal | 78 | 69.0 | 86 | 76.1 | |
| Elevated | 17 | 15.0 | 16 | 14.2 | |
| Respiratory rate | |||||
| NAD | 13 | 11.5 | 3 | 2.7 | |
| Low | 3 | 2.7 | 4 | 3.5 | 0.74** |
| Normal | 97 | 85.8 | 106 | 93.8 | |
| Temperature | |||||
| NAD | 13 | 11.5 | 3 | 2.7 | 0.064** |
| Normal | 80 | 70.8 | 92 | 81.4 | |
| Elevated | 20 | 17.7 | 18 | 15.9 | |
| Oxygen saturation | |||||
| NAD | 30 | 26.5 | 22 | 19.5 | 0.075** |
| Low | 3 | 2.7 | 4 | 3.5 | |
| Normal | 80 | 70.8 | 87 | 77.0 | |
| Total | 113 | 100.0 | 113 | 100.0 | |
| ** No significant difference (p > 0.05) | |||||
The reported maternal complications in women delivered by second-stage cesarean section were postpartum hemorrhage in 34(30.1%), sepsis in 11(9.7%), prolonged labor in eight (7.1%), uterine extension in four (3.5%), and umbilical cord prolapse in three (2.7%). The maternal complications in women delivered by first-stage cesarean section were postpartum hemorrhage in 13(11.5%), sepsis in one (0.9%), umbilical cord prolapse in one (0.9%), and uterine extension in one (0.9%) (p < 0.05) (Table 8).
| Table 8: Maternal complications of the women delivered by Second stage CS VS first stage CS (n = 226). | ||||
| Maternal complications | Type of CS | |||
| Second Stage CS | First stage CS | |||
| N | % | N | % | |
| No | 53 | 46.9 | 97 | 85.9 |
| Prolonged labour | 8 | 7.1 | 0 | 0.0 |
| Umbilical cord prolapses | 3 | 2.7 | 1 | 0.9 |
| Uterine extension | 4 | 3.5 | 1 | 0.9 |
| PPH | 34 | 30.1 | 13 | 11.5 |
| Sepsis | 11 | 9.7 | 1 | 0.9 |
| Maternal death | 0 | 0.0 | 0 | 0.0 |
| Total | 113 | 100.0 | 113 | 100.0 |
| p - value 0.01 | ||||
All maternal complications are common in the second stage of labor compared with the first stage of labor cesarean section p value < 0.05.
This study included 226 women: 113 delivered by the second stage of labor cesarean section as the case group and 113 delivered by the first stage of labor CS as the control group.
A fetal outcome study found significant differences between the fetuses of women delivered by the second stage of labor CS and the fetuses of women delivered by the first stage of labor CS; admission to the neonatal intensive care unit and the causes of admission were more common among the babies of women delivered by the second stage of labor cesarean section than those delivered by the first stage of labor cesarean section (p < 0.05).
The higher rate of admission of babies delivered by second-stage CS to the NICU is due to more frequent meconium aspiration, birth asphyxia, low Apgar score, and grunting. Similar to Khaniya, et al. s study in Nepal, perinatal complications included meconium stain liquor 10(27.77%), Transient Tachypnea of the Newborn (TTN) admissions 5(13.88%), Apgar score < 5 at 5 min 5 (13.55%), NICU admission2(5.54%), and fresh stillbirth 1(2.77%) [26,27].
An Indian study by Anusha, et al. revealed that neonatal outcome variables such as APGAR< 3 at 5 min, respiratory distress, and neonatal death were observed in nine, 28, and six deliveries, respectively [28]. These findings are in agreement with those of Khaniya, et al. [25], who found no statistically significant difference between maternal and neonatal mortality rates. Another study showed similar results since it did not find an increase in perinatal death in women who had a trial of labor after CS. For example, Samal and Pallavee [28] showed that neonatal morbidity was much higher in patients who underwent cesarean section during the second stage of labor. There was an increase in neonatal complications, such as APGAR less than 7 at 5 min, NICU admissions for more than 24 h, and neonatal septicemia (p < 0.001), which may be due to a deficiency in nursery staff. Jombo, et al, 44% of babies required nursery admission, most commonly due to birth asphyxia (16%) and respiratory distress syndrome (RDS) (11%) [29]. Gupta, et al. reported that out of 4477 deliveries, 1466 had cesarean section with a rate of 32%. The rate of second-stage cesarean sections was 3% of total cesarean section and 1% of total deliveries [30].
The second stage of labor cesarean section had higher maternal and perinatal morbidities, such as atonic PPH (33.3%), lower uterine segment extension (7%), febrile morbidity (10%), and the need for blood transfusion (15%). There were 15.5% NICU admissions in second stage cesarean group while none in first stage group, and this may be due to the unavailability of a senior or well-trained operator
Thirukumar, et al. [31] identified more maternal and perinatal complications of the second stage of labor cesarean sections. Blood-stained urine was the major complication observed in 60% of the patients, followed by difficulty in the extraction of the baby (48%). Lower uterine segment tears and angle extensions were observed in 12% of patients; PPH and broad ligament hematoma were noted in one patient. The mean duration of the hospital stay was 2.28 days, the longer duration was 5 days for the patient as she underwent a total abdominal hysterectomy due to extensive uterine tears during a cesarean section.
All babies had an APGAR score > 7 at 5 min. Nearly 20% (n = 5) of the babies were admitted to the PBU; among them, one required neonatal resuscitation at birth, and two received IV antibiotics for possible sepsis [32].
In this study, maternal complications, such as postpartum hemorrhage, sepsis, prolonged labor, and extended uterine tears, were significantly more common among women delivered by the second stage of labor CS than among women delivered by the first stage of labor CS. The reported maternal complications in women who underwent second-stage cesarean section were postpartum hemorrhage in 34(30.1%), sepsis in 11(9.7%), prolonged labor in eight (7.1%), extended uterine tears in four (3.5%), umbilical cord prolapse in three (2.7%), and episiotomy in three (2.7%). Maternal complications in women delivered by the first stage of labor via cesarean section were postpartum hemorrhage in 13(11.5%), sepsis in 1(0.9%), umbilical cord prolapse in 1(0.9%), extended uterine tear in 2(0.9%), and episiotomy in 0(0.0%) (p < 0.05). Similar to the study by Umbeli. et al. in Omdurman maternity hospital showed that Postoperative complications were reported in 142 (30.2%), mainly due to puerperal infection, postpartum hemorrhage (PPH), paralytic ileus, wound dehiscence and one maternal death [33] and Sucak [34].
McKelvey, et al. investigated the background and morbidity a total of 91(15.3%) of the 595 emergency cesarean sections underwent full dilatation. Instrumental delivery was attempted in 36(40%) patients. The most common maternal complications were postpartum hemorrhage, sepsis, and uterine extension tears. Seven (8 %) infants were admitted to the neonatal unit. They found that these procedures carry high maternal morbidity but relatively low neonatal morbidity, and recommended that most senior obstetricians should be involved in decision-making and delivery in these cases [35]. Babre, et al. studied indications of second-stage cesarean section. During the study period of 2760, cesarean sections were performed, of which 61 underwent 2nd stage cesarean section. Of the 61 Caesarean deliveries, 14 were given a prior instrumental trial followed by 2nd stage cesarean section. Intraoperative complications were higher in terms of blood loss, primary PPH, and extension of uterine incision, in one case bladder injury was noticed this may conclude that CS following an Instrumental trial led to higher complications, and some hospitals try to avoid this by not giving patients instrumental trial. Patwardhan method was used in 23% of cases for delivery of deeply engaged heads. Atonic PPH was observed in 11.5% of patients, and 3.3% of patients had an extension of the uterine incision [36]. Gurung, et al. studied the feto-maternal outcome of cesarean section in the second stage of labor. During the study period, there were 40,860 deliveries. A total of 18,011(44%) babies were born by cesarean section, 10484 by emergency, and 7527 by elective delivery. Of the emergency cesarean sections, 200(1.9%) were performed during the second stage of labor. The indication of CS was CPD in 92.4%, maternal complications, atonia PPH (12.5%), postpartum pyrexia (18.8%), and wound infection (4.8%).
The explanation is that the studies are in agreement with our results, and those results comply with biological reasoning and are similar to [37-39].
Study strengths and limitations
The strength of this study is that it compared women delivered by CS in the second stage of labor versus first-stage CS in all maternal and fetal outcomes, which increased the significance of the study. Our hospital is a major referral hospital that facilitates the inclusion of a high number of women, and its characteristics can be generalized to other hospitals. In addition, neonatal intensive care unit admission was evaluated and indications for cesarean section delivery were included, which increases the significance of the study.
The limitation of this study was that we did not compare preoperative and postoperative hemoglobin levels and a figure was not used to compare the population of the case group and the control group.
Postnatal complication long-term follow-up not addressed and neonatal death.
The increasing trend of CS in the second stage of labor is a major concern in modern obstetrics, which is a technically more difficult procedure than CS in early labor.
This study aimed to compare maternal and fetal outcomes between mothers who delivered second-stage CS and mothers who delivered first-stage CS.
A total of 113 mothers who delivered second-stage CS and 113 mothers who delivered first-stage CS at Alhasahisa Teaching Hospital were included.
The common indications in women who delivered via second-stage cesarean section were fetal distress, obstructed labor, and failure to progress.
Maternal complications in women delivered by second-stage cesarean section include postpartum hemorrhage, sepsis, prolonged labor, extended tears, umbilical cord prolapse, and episiotomy.
While admission to the neonatal intensive care unit and causes of admission were more common among the babies of women delivered by second-stage cesarean section, the second stage of labor CS should be performed by the most trained senior registrar. Pediatricians should attend the 2nd stage of CS.
The study concluded that the second stage of labor cesarean section is associated with a higher rate of maternal and fetal complications than the first stage of cesarean section. Women delivered by second-stage cesarean section showed more complications of postpartum hemorrhage, sepsis, and extended uterine tear, as well as more fetal complications, such as admission to the neonatal intensive care unit, low Apgar score, birth asphyxia, and fresh stillbirths.
Recommendations
To reduce the second-stage CS rate assisted vaginal delivery should encourage, the second stage of labor, CS, should be performed by the most available trained senior registrar. Pediatricians should attend the 2nd stage of labor CS. Hospitals covered by joints should be obstetricians on call.
Midwives should be aware of the signs of complicated CS to transfer patients as early as possible. There is an urgent need to conduct a Multi-centric study of Feto-maternal outcomes in the second stage of labor CS to obtain recommendations that may be approved as a local protocol in this situation. Women in the study area should be advised about the importance of antenatal care follow-up and health centers in the study area should provide proper antenatal care. Audit of second stage cesarean section indications.
Declaration
The Submitted manuscript contains original and authentic results, data, and ideas that have not been published elsewhere. No material from other publications has been reproduced in this article. The author of this paper read and approved the final version of the manuscript. None of the co-authors should submit the same manuscript to more than one journal.
Ethical clearance
Ethical approval was obtained from the Research and Ethics Committee of Alhasahisa. The ethical principles of autonomy, beneficence, non-maleficence, and justice, as stipulated in the ethical guidelines of the Sudan Medical Specialization Board (SMSB) and Medical Research Council, were upheld throughout the study. The approval number provided by the ethics review committee is 10270.
Written consent was obtained from all the respondents who agreed to participate in the study. The study was not associated with experimental or therapeutic interventions, and information was collected from them.
Availability of data and materials
All data and materials are available upon request.
Competing interest: No direct or indirect financial interests or conflicts exist, all authors agree with the content of the manuscript, and there are no conflicts of interest between or among them.
Funding: No funding was received from any institute or organization for this study. This research project was self-sponsored with the help of colleagues and co-authors.
Authors contribution: All the authors contributed to this research.
| Questionnaire |
| Patient number: ……. |
| 1. Age: ……………………… |
| 2. Residence: ............................................... |
| 3. Education: Illiterate ( ) Primary ( ) Secondary ( ) University ( ) |
| 4. Gravidity: ………………………………………………………………. |
| 5. Parity: ............................................................................ |
| 6. ANC i) Regular ( ) ii) Irregular ( ) iii) never at all ( ) |
| 7. Type of Em CS: 1st stage ( ) 2nd stage ( ) |
| 8. Indication for Em CS in 2nd stage : (1) Failure of progress ( ) (2) Fetal distress ( ) (3) Obstructed labor ( ) (4) Chorioamnionitis ( ) |
| 9. PV findings ……… cm |
| 10. Station of presenting part: -3 ( ) -2 ( ) -1 ( ) 0 ( ) +1( ) +2 ( ) +3 ( ) |
| 11. Presentation: cephalic ( ) breech ( ) |
| 12. Position: ROA ( ) DOA ( ) LOA ( ) ROT ( ) LOT ( ) ROP ( ) DOP ( ) LOP ( ) RSA ( ) LSA ( ) RSL ( ) LSL ( ) RSA ( ) LSA ( ) |
| 13. Duration of membranes rupture …………… |
| 14. Pre-Em CS CTG: Reassuring ( ) Suspicious ( ) pathological ( ) |
| 15. Duration of 2nd stage labor……………………. |
| 16. Baby outcome: Male ( ) Female ( ) |
| 17. Apgar score: 1 min i) <5 ii) 5-7 iii) >7 5 min i) <5 ii) 5-7 iii) >7 |
| 18. Neonatal outcome: Alive ( ) Stillbirth ( ) |
| 19. Admission to neonatal intensive care unit NICU: Yes ( ) No ( ) |
| 20. If yes, indication for admission: Birth asphyxia ( ) Meconium aspiration ( ) others ………… |
| 21. Birth weight: …………………….. grams |
| 22. Did the neonate suffer from: i) Caput ii) Molding |
| 23. Maternal vitals before surgery: |
| · Blood pressure …………………………… |
| · Heart rate ……………………………. |
| · Respiratory rate…………………… |
| · Temperature…………………. |
| · Oxygen saturation ……………….. |
| 24. Maternal complications: 1. Yes ( ). 2. No ( ) |
| 25. If Yes: |
| a. Premature rupture of membrane Yes ( ) No ( ) |
| b. Prolonged labor Yes ( ) No ( ) |
| c. Umbilical cord prolapse Yes ( ) No ( ) |
| d. Episiotomies Yes ( ) No ( ) |
| e. Perineal tears Yes ( ) No ( ) |
| f. Postpartum hemorrhage Yes ( ) No ( ) |
| g. Rupture uterus Yes ( ) No ( ) |
| h. Sepsis Yes ( ) No ( ) |
We acknowledge the cooperation of Alhasahisa Teaching Hospital residents who participated in appointing the patients and following up. We also appreciate the commitment and compliance of the patients who reported the required data and attended the regular follow-up.
- Goswami KD, Parmar MM, Kunjadiya AN. Study of fetomaternal outcome in second stage cesarean section. International Journal of Reproduction, Contraception, Obstetrics and Gynecology. 2019; 8(6): 2169-2172.
- Offringa Y, Paret L, Vayssiere C, Parant O, Loussert L, Guerby P. Second stage cesarean section and the risk of preterm birth in subsequent pregnancies. Int J Gynaecol Obstet. 2022 Dec;159(3):783-789. doi: 10.1002/ijgo.14186. Epub 2022 Apr 6. PMID: 35307823.
- Kawakita T, Reddy UM, Grantz KL, Landy HJ, Desale S, Iqbal SN. Maternal outcomes associated with early preterm cesarean delivery. Am J Obstet Gynecol. 2017 Mar;216(3):312.e1-312.e9. doi: 10.1016/j.ajog.2016.11.1006. Epub 2016 Nov 10. PMID: 27840144; PMCID: PMC5334149.
- Davis G, Fleming T, Ford K, Mouawad MR, Ludlow J. Caesarean section at full cervical dilatation. Aust N Z J Obstet Gynaecol. 2015 Dec;55(6):565-71. doi: 10.1111/ajo.12374. Epub 2015 Jul 30. PMID: 26223774.
- Janani S. Primary Caesarean Section: A Prospective Observational study (Doctoral dissertation, Kilpauk Medical College, Chennai). 2020.
- Corry EMA, Ramphul M, Rowan AM, Segurado R, Mahony RM, Keane DP. Exploring full cervical dilatation caesarean sections-A retrospective cohort study. Eur J Obstet Gynecol Reprod Biol. 2018 May;224:188-191. doi: 10.1016/j.ejogrb.2018.03.031. Epub 2018 Mar 20. PMID: 29614445.
- Rada MP, Ciortea R, Măluțan AM, Prundeanu I, Doumouchtsis SK, Bucuri CE, Blaga LD, Mihu D. Maternal and neonatal outcomes associated with delivery techniques for impacted fetal head at cesarean section: a systematic review and meta-analysis. J Perinat Med. 2022 Feb 7;50(4):446-456. doi: 10.1515/jpm-2021-0572. PMID: 35119802.
- McKinney JR, Allshouse AA, Heyborne KD. Duration of labor and maternal and neonatal morbidity. Am J Obstet Gynecol MFM. 2019 Aug;1(3):100032. doi: 10.1016/j.ajogmf.2019.100032. Epub 2019 Aug 5. PMID: 33345796.
- Patil DA, Deshmukh V, Gadappa S, Chandwade A. Comparative Study of Maternal and Neonatal Outcomes in Second Stage LSCS Vs First Stage LSCS in Tertiary Care Centre. International Journal of Medical and Pharmaceutical Research. 2023; 4: 625-632.
- Anuff H, Rahman Z, Dube R, Al-Zuheiri ST. Comparison of Maternal and Neonatal Outcomes in Case of Primary Cesarean Section Done During Late vs. Early Labor. Applied Clinical Research, Clinical Trials and Regulatory Affairs. 2020; 7(3): 244-253.
- Flatley CJ. Maternal and perinatal factors associated with adverse perinatal outcomes at term and the development of a predictive model for identification of at-risk pregnancies. 2019.
- Dickinson FM, Allott H, Nyongesa P, Eyinda M, Muchemi OM, Karangau SW, Ogoti E, Shaban NA, Godia P, Nyaga L, Ameh CA. "It's complicated…": Exploring second stage caesarean sections and reasons for non-performance of assisted vaginal births in Kenya: A mixed methods study. PLOS Glob Public Health. 2023 Nov 17;3(11):e0001495. doi: 10.1371/journal.pgph.0001495. PMID: 37976293; PMCID: PMC10656000.
- Azza Jaafar B, Rihab Jaafar I, Yassir Ahmed Mohammed E, Awad Ali MA, Siddig Omer MH. Maternal and Perinatal Outcomes Among Women Underwent Second-Stage Versus First-Stage Caesarean Delivery at Ibrahim Malik Hospital in Sudan. WJ Gynecol Women’s Health. 1(3): 2018.
- Mandar O, Hassan B, Abdelbagi O, Eltayeb R, ALhabardi N, Adam I. Prevalence and Associated Factors for Post-Caesarean Delivery Blood Transfusion in Eastern Sudan: A Cross-Sectional Study. J Blood Med. 2022 May 9;13:219-227. doi: 10.2147/JBM.S355846. PMID: 35585876; PMCID: PMC9109909.
- Eltigani A, Ahmed TU, Suliman AA, SalahEldin A, Siralkatim I, Suliman H. Near-miss Women Causes and Prevalence in Alobied Maternity Hospital. Clinical Journal of Obstetrics and Gynecology. 2023; 6(4): 185-192.
- Alemu H, Yigzaw ZA, Asrade L, Nega B, Belachew A. Proportion and associated factors of maternal complications of cesarean sections among mothers who deliver at Bahir Dar City Public Specialized Hospitals, Bahir Dar, Ethiopia. BMC Womens Health. 2023 May 6;23(1):237. doi: 10.1186/s12905-023-02388-y. PMID: 37149559; PMCID: PMC10164306.
- Vitner D, Bleicher I, Levy E, Sloma R, Kadour-Peero E, Bart Y, Sagi S, Aviram A, Gonen R. Differences in outcomes between cesarean section in the second versus the first stages of labor. J Matern Fetal Neonatal Med. 2019 Aug;32(15):2539-2542. doi: 10.1080/14767058.2018.1440545. Epub 2018 Feb 22. PMID: 29471705.
- Sapir A, Friedrich L, Gat R, Erez O. Cesarean section in the second stage of labor is associated with early-term and late preterm birth in subsequent pregnancies. J Matern Fetal Neonatal Med. 2023 Dec;36(1):2175658. doi: 10.1080/14767058.2023.2175658. PMID: 36842965.
- Alexander JM, Leveno KJ, Rouse DJ, Landon MB, Gilbert S, Spong CY, Varner MW, Moawad AH, Caritis SN, Harper M, Wapner RJ, Sorokin Y, Miodovnik M, O'Sullivan MJ, Sibai BM, Langer O, Gabbe SG; National Institute of Child Health and Human Development (NICHD) Maternal-Fetal Medicine Units Network (MFMU). Comparison of maternal and infant outcomes from primary cesarean delivery during the second compared with first stage of labor. Obstet Gynecol. 2007 Apr;109(4):917-21. doi: 10.1097/01.AOG.0000257121.56126.fe. PMID: 17400854.
- Rahim A, Lock G, Cotzias C. Incidence of second-stage (fully dilated) cesarean sections and how best to represent it: A multicenter analysis. Int J Gynaecol Obstet. 2022 Jan;156(1):119-123. doi: 10.1002/ijgo.13672. Epub 2021 Apr 4. PMID: 33715159.
- Reid HE, Hayes D, Wittkowski A, Vause S, Whitcombe J, Heazell A. The effect of senior obstetric presence on maternal and neonatal outcomes in UK NHS maternity units: a systematic review and meta-analysis. BJOG. 2017 Aug;124(9):1321-1330. doi: 10.1111/1471-0528.14649. Epub 2017 May 5. PMID: 28332762.
- Ramphul M, Ooi PV, Burke G, Kennelly MM, Said SA, Montgomery AA, Murphy DJ. Instrumental delivery and ultrasound : a multicentre randomised controlled trial of ultrasound assessment of the fetal head position versus standard care as an approach to prevent morbidity at instrumental delivery. BJOG. 2014 Jul;121(8):1029-38. doi: 10.1111/1471-0528.12810. Epub 2014 Apr 11. PMID: 24720273.
- Lawani LO, Anozie OB, Ezeonu PO, Iyoke CA. Comparison of outcomes between operative vaginal deliveries and spontaneous vaginal deliveries in southeast Nigeria. Int J Gynaecol Obstet. 2014 Jun;125(3):206-9. doi: 10.1016/j.ijgo.2013.11.018. Epub 2014 Mar 11. PMID: 24717812.
- Vousden N, Cargill Z, Briley A, Tydeman G, Shennan AH. Cesarean section at full dilatation: incidence, impact, and current management. Obstet Gynaecol. 2014; 16(3): 199-205.
- Khaniya B. The fetomaternal outcome in second stage cesarean section. Nepalese Medical Journal. 3(1), 279-281.
- Eze P, Lawani LO, Chikezie RU, Ukaegbe CI, Iyoke CA. Perinatal outcomes of babies delivered by second-stage cesarean section versus vacuum extraction in a resource-poor setting, Nigeria–a retrospective analysis. BMC pregnancy and childbirth. 2020; 20: 1-7.
- Anusha SR. Our experience of maternal and fetal outcomes in 2nd stage cesarean deliveries-tertiary care center study. Blood Transfusion. 2020; 29: 58.
- Samal R, Pallavee P. The fetomaternal outcome of nulliparous women undergoing cesarean section in the first and second stage of labor: A prospective study in a tertiary care center of Puducherry. Int J Clin Obstet Gynaecol. 2019; 3(5): 166-9.
- Jombo S, Ossai C, Onwusulu D, Ilikannu S, Fagbemi A. Feto-maternal outcomes of caesarean delivery in Federal Medical Centre, Asaba: a two year review. Afr Health Sci. 2022 Mar;22(1):172-179. doi: 10.4314/ahs.v22i1.22. PMID: 36032432; PMCID: PMC9382540.
- Gupta N, Gupta T, Singh R. The feto-maternal outcome in second versus first stage cesarean delivery in a tertiary medical care center. International Journal of Reproduction, Contraception, Obstetrics and Gynecology. 2018; 7(12): 5084-5088.
- Thirukumar M. Feto-Maternal Outcome in Caesarean Sections Performed in Second Stage of Labour. Jaffna Medical Journal. 2020; 32(1).
- Vashi CA, Vijay N, Bhalerao A, Shetty A, Vashi C. Obstetrics Outcomes in Women Undergoing Second-Stage Cesarean Section: A Cross-Sectional Study. Cureus. 2023; 15(6).
- Umbeli T, Ismail S, Kunna A, Elmahgoub A, Nasr A, Abdalwahab R. Maternal and neonatal complications associated with cesarean section in the second stage of labor at Omdurman maternity hospital during 2012-2013. Merit Research Journal of Medicine and Medical Sciences. 2014; 2(10): 225-228.
- Sucak A, Celen S, Akbaba E, Soysal S, Moraloglu O, Danışman N. Comparison of nulliparas undergoing cesarean section in first and second stages of labour: a prospective study in a tertiary teaching hospital. Obstet Gynecol Int. 2011;2011:986506. doi: 10.1155/2011/986506. Epub 2011 Sep 20. PMID: 21941557; PMCID: PMC3176624.
- McKelvey A, Ashe R, McKenna D, Roberts R. Caesarean section in the second stage of labour: a retrospective review of obstetric setting and morbidity. J Obstet Gynaecol. 2010 Apr;30(3):264-7. doi: 10.3109/01443610903572109. PMID: 20373928.
- Babre VM, Bendre KR, Niyogi G. Review of cesarean sections at full dilatation. International Journal of Reproduction, Contraception, Obstetrics and Gynecology. 2017; 6(6): 2491-2494.
- Khaniya B. Fetomaternal outcome in second stage cesarean section. NMJ. 2020; 3(1):279-81.
- Goswami KD, Parmar MM, Kunjadiya AN. Study of fetomaternal outcome in second stage cesarean section. International Journal of Reproduction, Contraception, Obstetrics and Gynecology. 2019; 8(6): 2169-2172.
- Gurung P, Malla S, Lama S, Malla A, Singh A. Caesarean Section During Second Stage of Labor in a Tertiary Centre. J Nepal Health Res Counc. 2017 Sep 8;15(2):178-181. doi: 10.3126/jnhrc.v15i2.18210. PMID: 29016591.