More Information
Submitted: January 23, 2024 | Approved: February 14, 2024 | Published: February 15, 2024
How to cite this article: Soares L, Dantas SA. Cervical Cancer and Quality of Life: Systematic Review. Clin J Obstet Gynecol. 2024; 7: 017-024.
DOI: 10.29328/journal.cjog.1001158
Copyright License: © 2024 Soares L, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Cervical cancer; Human Papiloma Virus - HPV; Treatment; Prevention; Quality of life
Cervical Cancer and Quality of Life: Systematic Review
Luísa Soares* and Sofia Abreu Dantas
and Sofia Abreu Dantas
Department of Psychology, University of Madeira, FAH, Portugal
*Address for Correspondence: Luisa Soares, Department of Psychology, University of Madeira, FAH, Portugal, Email: [email protected]
Cervical cancer is diagnosed annually in thousands of women around the world, and thousands die from it. The main objectives of this systematic review were to understand and characterize cervical cancer and understand what impacts it has on the lives of diagnosed women and survivors. To this end, a systematic review based on the PRISMA principles was carried out. The search was carried out through the Online Knowledge Library (B-on), obtaining 1179 articles, which were verified, considering the inclusion and exclusion criteria, with 18 articles and 20 additional references included in this review. The results demonstrated that cervical cancer (1) is preventable and can be treated with good results if identified early; (2) it is caused by Human Papilloma Virus infection; (3) it can be treated using different techniques; and (4) it has significant impacts on women's quality of life.
Cervical cancer is preventable and can be cured if detected early and treated appropriately. However, it continues to be one of the most common cancers with the highest number of deaths among women, thus representing a health concern and a threat to women's lives [1-6].
Cervical cancer is the 4th most common type of cancer among women worldwide, and in 2020, it is estimated that there were around 604,000 new cases and 342,000 deaths [7,8]. Indeed, these numbers are already high and are expected to continue to rise, reaching 700,000 cases and 400,000 deaths by 2030 [5]. According to the National Cancer Institute (n. d.), [9] in 2023, and to date, around 13,960 new cases of cervical cancer have been identified, and the estimated number of deaths caused by it is 4,310.
It should also be noted that all countries are affected by cervical cancer. However, in low- and middle-income countries, the incidence is almost twice as high, and mortality rates are three times higher than in high-income countries [5,10]. In other words, around 90% of cervical cancer cases occur in low- and middle-income countries and this is due to the lack of access to vaccination against the Human Papillomavirus (HPV), quality screening, and the lack of treatment for cervical cancer [2,5].
At the European level, incidence estimates are 13 new cases per 100,000 women and four deaths per 100,000 women [11,12].
In Portugal, cancer represents the second leading cause of death, and in the last decade, there have been few improvements in mortality rates. Regarding cervical cancer, estimates suggest that there are 15 new cases and three deaths for every 100,000 women [11,12].
In the Autonomous Region of Madeira, malignant tumors (cancers) are the second cause of death, and in 2020 resulted in around 622 deaths (374 men and 288 women), which in turn is equivalent to 24.4% of mortality in the Region. Regarding cervical cancer in the Region, between 2018 and 2020, around 48 new cases of cervical cancer were identified [12,13]. Also, in 2020, 5 women aged between 50 and 79 died in the Region due to this type of cancer [12,13].
Regarding the overall survival rate, according to the [9] around 67.2% of women diagnosed with cervical cancer survive five or more years after being diagnosed with the disease. In Europe, the net survival rate for cervical cancer is 64%, and in Portugal, it is 66% [11]. It must be taken into account that the earlier cervical cancer is diagnosed, the greater the chance of survival [9].
Indeed, the research objectives are (1) to understand and characterize cervical cancer and its characteristics and (2) to understand how cervical cancer influences the quality of life of women diagnosed and survivors.
Therefore, the research questions are: (1) What is cervical cancer and its characteristics? Moreover, (2) How does cervical cancer influence the quality of life of diagnosed and surviving women?
A literature review was carried out based on the principles of Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [14,15]. Considering the research objective, the following terms in the research are "Cervical cancer," "symptoms," psychological effects and impacts," and "quality of life." The research took place in September and October 2023, and the Online Knowledge Library (B-On) and all databases available on this platform were used. It should also be noted that the research focused only on scientific articles published between 2003 and 2023 in English and Portuguese. However, the option for the Portuguese language was not available.
The inclusion criteria defined were: (a) scientific articles published between 2003 and 2023, (b) scientific articles from academic journals, (c) articles in English and Portuguese, (d) articles available in full, and (e) articles that mentioned cervical cancer in the title and abstract and that were relevant to the topic to be addressed. The exclusion criteria were: (a) scientific articles published before 2003, (b) scientific articles that were not published in academic journals, (c) articles in languages other than English or Portuguese, (d) articles that were not fully available, (e) documents that were not scientific articles and (f) articles whose title and abstract did not mention cervical cancer.
In the research carried out at B-on, the following research protocol was used: ("cervical cancer") AND (symptoms) AND ("psychology* effects" OR "psychology* impact") AND ("quality of life") NOT ("breast cancer"). The Boolean Operators "AND" were used to ensure that the four topics above were all included in the search, "OR" to increase the possibilities of results, and "NOT" to narrow the search further. Regarding truncators, the "*" symbol included words with the exact origin. The "was" used to ensure that concepts with two words were considered together, not individually. Inclusion and exclusion criteria (a), (b), (c), and (d) were achieved using the tools available at B-On, and I manually checked criteria (e) and (f).
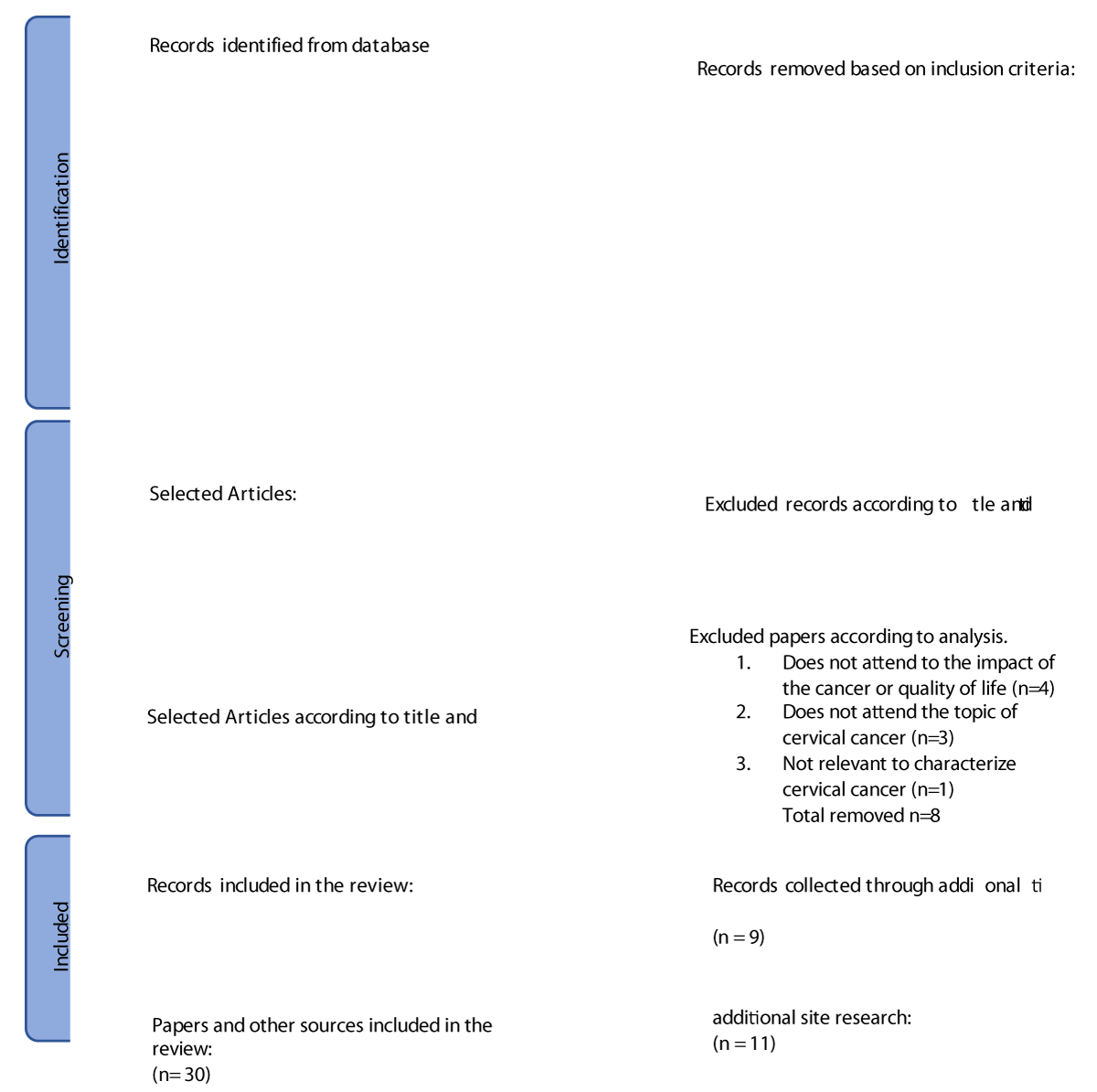
Effectively, first, around 1179 results were obtained. Then, we applied the date criterion and ended up with 1098 articles. Then, we selected the full-text option and ended up with 314 articles. After we selected the language option (there was an option for articles in English but none for Portuguese), 311 articles remained. Then, it excludes 46 conference papers and abstracts. We ended up with 154 articles, as B-on itself removed the duplicates and removed two repeated articles manually. Then, we read the titles and abstracts of these 154 articles, considering whether they mentioned cervical cancer and were relevant to the objective, thus excluding 136 articles. Then we were left with 18 articles, of which 8, after reading them thoroughly, we decided to exclude, leaving with 10 (Figure 1). Additionally, we included sources, some websites of trustworthy organizations, and article recommendations given by the teacher (11 references), and I consulted the secondary references of some main articles (9 secondary articles).
Figure 1: PRISMA diagram: Guidelines for reporting systematic reviews [14,15].
Cervix cancer
Cervical cancer develops in a woman's cervix, specifically in the cells lining it, at the entrance to the uterus through the vagina [8,16]. Cervical cancer develops when there is an uncontrolled and abnormal growth of cells in the cervix, and these changes are not immediate but relatively gradual; that is, they develop little by little and can culminate in cancer [17].
Cause
According to the Portuguese League Against Cancer (2023), [18] around 100% of cervical cancer cases occur due to HPV infection (a high-risk subtype), with this virus being responsible for 84% of cancers. Of the anus, 70% of cancers of the vagina, 47% of cancers of the penis, 40% of cancers of the vulva, and 99% of condylomas or warts on the genitals [2,8,16,18,19]. Also, HPV can influence the development of mouth and throat cancer [17,20-22].
HPV is a virus that infects cells on the surface of the skin and surfaces covering the genitals and other parts of the body (such as the mouth, throat, and anus) but not the blood or internal organs (such as the heart or lungs). Moreover, although there is no cure, HPV is treatable [17].
HPV is easily transmitted sexually and most people become infected with this virus shortly after sexual intercourse; However, this is the case; transmission does not only occur when there is penetration but also occurs through skin-to-skin contact, sexual activity (sex, anal sex, and oral sex) in the genital areas (e.g., anus, lips, among others) [8,17]. It is also important to note that HPV does not choose genders or ages; that is, both men and women can become infected by it [8,23,24].
Most sexually active women and men will eventually be infected since the peak period for becoming infected by HPV is right after the beginning of sexual life and in some cases, the same individual can be infected more than once [8,18].
In most cases (around 90%) of HPV infection, the body manages to eliminate it after one to two years, the infection disappears spontaneously, there are no symptoms, even when the infection is already established, and the lesions pre-cancer resolve. However, in other cases, the infection does not disappear/is persistent, and this can lead to a variety of clinical conditions (from pre-cancer lesions to cancer and genital diseases), both in men and women, such as cancer of the cervix [4,5,17-19,25].
HPV infection is widespread (around 75% of people under fifty have it or have had it), and there are more than two hundred types of HPV recognized, of which preferentially affect the genital organs (vulva, cervix, vagina, penis, and anus). HPV can be a low-risk type (not linked to the development of cancer) or a high-risk type (it is linked to the development of cancer), with high-risk HPV types including types 16 and 18, which are responsible for 75% of the most severe lesions and if they persist and are not identified, they can lead to cancer [17,18].
For cervical cancer to develop and manifest, it can take between fifteen and twenty years in women with a standard immune system. In women with a weaker immune system (such as women with an untreated infection by the Human Immunodeficiency Virus), the development time is reduced to five to ten years [8].
Risk factors
In fact, there are controllable risk factors that can increase the likelihood of cervical cancer, including: (1) HPV infection; (2) the person's sexual history (having started sexual life early, especially before the age of 18, having or having had several sexual partners or having a partner who has the infection, considered high risk, or has had several partners;, (3) if the individual smokes (the chemicals released are transported in our blood system, damage the DNA of cervical cells and make our immune system less effective in fighting HPV infections); (4) have a weak immune system; (5) have or have ever been infected with chlamydia (studies show that chlamydia bacteria can help HPV grow and stay) or have a history of sexually transmitted infections; (6) long-term use of contraceptives oral (pill, for example); (7) having had several full-term pregnancies (women who have had 3 or more full-term pregnancies have a higher risk); (8) being young at the first full-term pregnancy (women under 20 year olds who have had their first pregnancy are exposed to a greater risk than compared to women who only became pregnant after the age of 25); (9) economic status (women from low-income countries do not have as much access to health screening services, which can lead to non-identification of lesions that can progress to cancer); (10) having a diet low in fruit and vegetables (women who do not include fruits and vegetables in their diet may be exposed to a greater risk) and (11) not carrying out regular screening practices (in countries that have screening programs) [2,17].
Additionally, cervical cancer may run in some families. Consequently, if any member of a woman's family has been affected, the chances of her developing cancer are very high, and this is a risk factor that cannot be controlled/altered [17,26].
Symptoms
In the early stages of cervical cancer, there are usually no signs or symptoms; however, when the tumor develops and begins to grow progressively in the skin tissue, symptoms appear [2,17,18]. The most common symptoms are (1) abnormal vaginal bleeding (during or after sexual intercourse, after menopause, bleeding between periods and larger or heavier menstrual bleeding than usual, for example); (2) unusual bloody vaginal discharge; (3) abundant discharge with or without blood, but with an intense smell, followed by spontaneous blood loss; (4) pain in the pelvic Region and (5) pain during sex [17,18,26].
In more advanced cases of cervical cancer, swelling of the legs may occur, problems urinating, and blood may appear in the urine [17,18,27].
However, it is necessary to understand that these symptoms vary depending on the structures affected. They may arise from other medical conditions other than cancer. If any of these symptoms are present, it is advisable to consult a doctor so that, if applicable, the chances of successful cancer treatment are greater [17,18].
Prevention
As previously mentioned, cervical cancer is preventable, and prevention can be implemented through primary and secondary prevention strategies, maximizing quality of life [3,8,28,29].
Primary prevention focuses on avoiding HPV infection and encompasses vaccination against HPV, education about tobacco use, sexual education, and safe sexual practices (such as the use of condoms, which are not 100% effective but can prevent infection). As for secondary prevention, this covers cervical cancer screening programs and strategies [2,3,8,19,30].
According to the Portuguese League Against Cancer (2023), [18] the best protection is to associate vaccination with screening since these two methods become more effective together in preventing pre-cancer lesions and cervical cancer [28]. Additionally, the HPV vaccine prevents several diseases caused by the virus. However, it does not replace screening [8,31,32].
HPV vaccines work best if they are administered before exposure to the virus. For this reason, the World Health Organization recommends vaccinating girls between the ages of 9 and 14, as most girls have not yet started—their sex life [8].
Regarding screening, the most used method is the Pap test (original screening test), which allows changes to be found in a woman's cervix before the development of cancer or pre-cancer lesions and even identifying cancer at an early stage. (when it is small and easy to treat) Moreover, the HPV test can be applied individually or together [2,8,17,29]. Additionally, according to [29], it is recommended that women adhere to screening only after age 21.
Interestingly, in high-income countries, there are several HPV vaccination programs, regular screenings, and appropriate treatment. On the contrary, in low- and middle-income countries, access to these preventive measures is limited, and, in many cases, cancer is only identified at a more advanced stage, where symptoms are already manifested. Moreover, access to treatment may also be limited, resulting in a higher mortality rate from cervical cancer in these countries [8,33].
Therefore, it is crucial to highlight that health education on this topic is essential to raise people's awareness and motivate them to adopt preventive behaviors against cervical cancer [3,31] and that, based on a prevention approach, screening, and treatment, cervical cancer could be eliminated as a public health problem within a generation [19].
Therefore, HPV vaccination, screening, and treatment of pre-cancer lesions are an effective way to prevent cervical cancer (World Health Organization, 2022). Advances in cervical cancer screening (regular Pap testing and HPV DNA testing) have led to a decrease in cervical cancer rates compared to other types of cancer [1,23,24].
However, although these screening techniques are effective, there are still many racial and ethnic disparities in screening and detection [1].
Diagnosis
Cervical cancer is curable/treatable if diagnosed early and monitored and treated appropriately. Despite this, cancers diagnosed later can also be controlled with appropriate treatments and palliative care [8,19].
Cervical cancer is often diagnosed in women between the ages of 30 and 50, with the average diagnosis being at age 50, but it can also occur after age 65. However, this cancer rarely develops in women under 20 [1,9,17].
In the early stage of cervical cancer, when it is asymptomatic, the diagnosis can be made with the support of a routine screening test, such as a Pap smear or a pelvic exam, which allows the cervix to be visualized [2].
Also, to make the diagnosis, a colposcopy can be carried out, allowing observation of the cervix to check if the woman has any lesions on it. When a lesion or abnormality is verified, a biopsy can be performed, which consists of removing a small tissue fragment, to determine which lesion is present and consider the best type of treatment [2,18].
For example, if any lesion or change is identified from the Pap test, a colposcopy is performed to make the diagnosis. Then, a biopsy is carried out to analyze the tissue. Thus, if the lesion is identified at an early stage by colposcopy and biopsy, then it is possible to perform surgery to remove this portion of tissue [26].
Medical treatment
The type of treatment given to a woman with cervical cancer must be chosen with her so that she can be informed of the side effects of the treatment she chooses (for example, discussing with the patient whether she wants to have children or not) [17].
The most common treatments for cervical cancer include surgery, radiotherapy, chemotherapy, drug therapy, and immunotherapy, and each of these treatment modalities has different impacts/effects on women's quality of life [2,7,17,26].
Firstly, surgical treatment (which implies the removal of cancerous tissue) has two main techniques: ablation, which destroys cancerous tissue in the cervix with cold temperatures or a laser, and excisional surgery, which cuts and removes cancerous cells. This treatment modality can cause side effects such as infertility or complications such as infections, bleeding, and damage to the urinary system, among others [17,26].
Secondly, radiotherapy uses high-energy X-rays to kill cancer cells, and side effects include fatigue (tiredness), stomach pain, nausea and vomiting, skin changes (redness or peeling), bladder changes (urge to urinate more often or blood in the urine), vaginal pain, menstrual changes or early menopause, among others [17,26].
Third, chemotherapy uses drugs that are injected into a vein or taken orally, which enter the blood system and help kill cancer cells. Side effects include nausea, loss of appetite, hair loss, tiredness and fatigue, and mouth ulcers [17,26,34].
Drug therapy focuses on destroying cancer cells or reducing their growth; some promote strengthening the immune system. Some examples of side effects of this method are tiredness, nausea, and high blood pressure [17,35,36].
Next, immunotherapy is a new technique that has shown promising results and focuses on using medications to increase the effectiveness of the immune system so that it can recognize and eliminate cancer cells. Side effects include fatigue, fever, nausea, headaches, and loss of appetite, among others [17,26,36].
Additionally, the type of treatment used depends on the stage of the cancer and the extent of the disease at the time of diagnosis and depends on the resources available [2,17,26]. In the case of early-stage cervical cancer, surgery (a widespread and successful technique) or radiotherapy can be used. However, in more advanced stages, other methods must be used [26].
Therefore, the treatment modality must be chosen with the patient so that they can discuss the best treatment strategy and possible side effects with their doctor and ask questions about the process [17].
Impacts and quality of life
According to the literature, with the diagnosis and treatment of cervical cancer, impacts arise at a physical level, a sexual and reproductive level, a relational and social level, a psychological level, and an economic level of disease face. Short and long-term, influencing their quality of life [28,37,38].
Effectively, the treatment has several impacts on a physical level, which will depend on the type of treatment available, from incontinence (leakage of urine and the urge to urinate frequently, in cases of radiotherapy treatment), intestinal problems, swelling of the legs, physical changes in the vagina (in cases of surgery), vaginal rigidity, gynecological problems, among others, as previously mentioned [27,34,37,39,40].
These side effects affect not only women's social interactions but also their quality of life, as some women may feel embarrassed to be in the presence of other people when they experience these effects [40,41].
Cervical cancer and its treatment also have sexual impacts, and for some women, there may be a decrease in sexual interest, loss of libido, lack of sexual excitement, pain during sexual intercourse, and feelings of anxiety. Moreover, fear regarding penetration, as fear of pain, often leads women to avoid having sexual intercourse, and, therefore, sexual functioning can be compromised due to physical discomfort [27,34,40,42].
Cancer can also affect a woman's marital relationship, if applicable, due to this loss of sexual interest, as they may experience some feelings of guilt towards their partner and can also influence communication with their partner [27,40,43].
Regarding reproduction, women with cervical cancer, in comparison to the public, reveal that they have significant concerns about reproduction, derived from the sadness and frustration of the inability to have children, the inability to talk openly about fertility, and the mourning of the loss of the ability to have children after treatment. These concerns, in turn, are also associated with a decrease in the quality of life of these women and affect satisfaction in intimate relationships and the self-perception of wives and mothers [27,42,43].
In addition to the physical impact of diagnosis and treatment, cervical cancer also has psychological impacts on women in the short and long term, especially regarding their identity, body image, and self-confidence; women can often experience feelings of insecurity [27,43-46]. Also, according to the study by [39], women with cervical cancer with a lower quality of life reported feelings of depression and anxiety, and according to [40], some women may experience feelings of anxiety constantly, related to the fear of the disease recurring. Other psychological responses include worry, aggression, anger, and emotional distress [28,37,47].
Women who survive cervical cancer experience significant disruptions to their well-being, and this persists long-term, with younger survivors appearing to experience more distress [42,48].
Also, cervical cancer survivors reported poor quality of life due to side effects (urinary, sexual, and psychological difficulties) related to the disease and treatment [27].
The quality of life of women with cervical cancer depends on the type of treatment they undergo. An example of this is the study by [34] where surviving women treated with surgery alone or in conjunction with chemotherapy reported having a quality of life like that of healthy women, while women treated with radiotherapy scored lower levels of quality of life. Moreover, in the study by [39] it was identified that radiation treatment with or without chemotherapy contributed to a significant decrease in quality of life, higher stress levels, and depression.
As survival rates have been increasing, it is essential to evaluate the quality of life after treatment, and such an evaluation must include physical and functional well-being and emotional and social well-being [7]. For this reason, healthcare professionals need to recognize that aspects of cancer survival require attention and follow-up care [42].
Regarding the economic impact, according to [28], some women experience economic challenges, such as loss of ability to work, loss of employment and high medical expenses, and disruptions in social relationships, from the end of marriages, isolation by the family and by the community, with the diagnosis and progression of the disease. Also, in the study by [47] participants revealed that several aspects of their economic life were affected, such as the disruption of economic activities, which caused an interruption in their productive routine and the reduction of their capabilities to produce and work as before, which culminated in their dependence on their family (to satisfy their basic needs).
Social support is an aspect that also proved to be associated with and crucial to the quality of life. Social support seems to be very relevant for women with cervical cancer, from diagnosis, during treatment and after, to deal with the emotional difficulties of a cancer diagnosis [48,49]. Thus, in cases of diagnosed women who perceive they have lower social support and do not feel connected or supported by others, they must deal with the psychological implications, physical changes, and logistics of treatment alone, which is associated with levels of lower quality of life [44,49].
It is also important to note that, with the diagnosis of cervical cancer, some women may experience discrimination and stigmatization, and this also influences their well-being and quality of life. In the study by [44] women reported experiences of discrimination and ostracization due to the stigma associated with HPV, as well as opposing views related to the transmission of this virus, which is sexually transmitted, and assumptions about sexual health and women's behavior led to stigmatizing labels (such as promiscuity) [44].
Moreover, in effect, this view of blame attributed to diagnosed women triggers feelings of self-criticism and shame, which can result in isolating behaviors and adverse health outcomes (such as a decrease in the use of health services and preventive screening, due to the stigma of promiscuity), thus negatively affecting their quality of life [44,50,51].
Cervical cancer, as we have seen, affects thousands of women worldwide every year. Prevention strategies and education on this topic play an essential role here, and we must continue investing in them to decrease incidence and mortality rates. It is important to highlight again that this type of cancer is preventable and curable if detected at an early stage, and, therefore, it is essential that all women have access not only to information about cancer but also to screening, treatments, and adequate medical and psychological support.
With this work, it was able to infer the impacts and challenges that women with cervical cancer face daily, and we realized that, in cases like this, the psychologist's role is strictly necessary and helpful. Also, it is essential to highlight the need to look at the psychological impacts that cancer brings with it and promote the creation of studies and intervention programs that focus on promoting the quality of life and well-being of people with cancer.
Regarding the limits of this review, we highlight the choice of keywords, as they may not have been the most appropriate for the study objective. Also, another limitation was that we only carried out the research in a single database (in this case B-On), which may have limited my access to articles relevant to the research objective and created some risk of bias. We would also like to add that another limitation was the short time it took to carry out this study, which meant that we could not delve deeper into other themes/aspects related to cervical cancer as we would have liked. It is also worth mentioning that this review mainly included only articles in English, in addition to the websites and other sources used, which may also have limited access to more information on the topic.
We understand that, as expected, cervical cancer has an impact on the well-being and quality of life at different levels of women who have it. Also, we were able to understand that the psychologist can and should work in the oncological context and in what aspects he can and should work so that women diagnosed, undergoing treatment, and survivors can learn strategies that help them face cancer and promote their well-being.
- Abboud S, De Penning E, Brawner BM, Menon U, Glanz K, Sommers MS. Cervical Cancer Screening Among Arab Women in the United States: An Integrative Review. Oncol Nurs Forum. 2017 Jan 1;44(1):E20-E33. doi: 10.1188/17.ONF.E20-E33. PMID: 27991600; PMCID: PMC5553625.
- Cohen PA, Jhingran A, Oaknin A, Denny L. Cervical cancer. Lancet. 2019 Jan 12;393(10167):169-182. doi: 10.1016/S0140-6736(18)32470-X. PMID: 30638582.
- Lemos MS, Rothes IA, Oliveira F, Soares L. Raising cervical cancer awareness: Analysing the incremental efficacy of Short Message Service. Health Education Journal. 2017; 76(8):1-15. https://doi.org/10.1177/0017896917728
- Nijhuis ER, Reesink-Peters N, Wisman GB, Nijman HW, van Zanden J, Volders H, Hollema H, Suurmeijer AJ, Schuuring E, van der Zee AG. An overview of innovative techniques to improve cervical cancer screening. Cell Oncol. 2006;28(5-6):233-46. doi: 10.1155/2006/273547. PMID: 17167177; PMCID: PMC4617820.
- World Health Organization. Global strategy to accelerate the elimination of cervical cancer as a public health problem. World Health Organization. 2020. https://www.who.int/publications/i/item/9789240014107
- Zibako P, Tsikai N, Manyame S, Ginindza TG. Cervical cancer management in Zimbabwe (2019-2020). PLoS One. 2022 Sep 21;17(9):e0274884. doi: 10.1371/journal.pone.0274884. PMID: 36129898; PMCID: PMC9491541.
- Stuopelytė R, Žukienė G, Breivienė R, Rudaitis V, Bartkevičienė D. Quality of Life in Cervical Cancer Survivors Treated with Concurrent Chemoradiotherapy. Medicina (Kaunas). 2023 Apr 17;59(4):777. doi: 10.3390/medicina59040777. PMID: 37109735; PMCID: PMC10141383.
- World Health Organization. Cervical cancer. 2022. https://www.who.int/news-room/fact-sheets/detail/cervical-cancer
- National Cancer Institute. (n. d.). Cancer Stat Facts: Cervical Cancer. https://seer.cancer.gov/statfacts/html/cervix.html
- Global cancer observatory. Cervical cancer mortality rates in the world per 100,000 inhabitants. 2020. https://gco.iarc.fr/en
- Organization for Economic Cooperation and Development. Perfil sobre cancro por país. OECD Publishing. 2023. https://doi.org/10.1787/40186a6b-pt
- Regional Directorate of Statistics of Madeira. Health Statistics for the Autonomous Region of Madeira. Regional Directorate of Statistics of Madeira. 2022.
- RTP Madeira. Screenings detected 50 cases of cervical cancer. 2022. https://www.rtp.pt/madeira/politica/rastreios-detetaram-50-casos-de-cancro-do-colo-do-utero-video_99293
- Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA Statement. Open Med. 2009;3(3):e123-30. Epub 2009 Jul 21. PMID: 21603045; PMCID: PMC3090117.
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev. 2021 Mar 29;10(1):89. doi: 10.1186/s13643-021-01626-4. PMID: 33781348; PMCID: PMC8008539.
- World Cancer Research Fund International. Worldwide cancer data: Global cancer statistics for the most common cancers worldwide. 2022. https://www.wcrf.org/cancer-trends/worldwide-cancer-data/
- American Cancer Society. Cervical cancer. 2023. https://www.cancer.org/cancer/types/cervical-cancer.html
- Portuguese League against cancer. Cervix cancer. 2023. https://www.ligacontracancro.pt/cancro-do-colo-do-utero/
- World Health Organization. (n.d.). Cervical Cancer. https://www.who.int/health-topics/cervical-cancer#tab=tab_1
- Soares L, Moniz S. Overconsumption and the Effects on Mental Health and Well-Being: A Review, Current Research in Diabetes & Obesity Journal. 2023.
- Silva S, Bártolo A, Santos IM, Paiva D, Monteiro S. Validation of the Portuguese Version of the Fear of Progression Questionnaire-Short Form (FoP-Q-SF) in Portuguese Cancer Survivors. Healthcare (Basel). 2022 Dec 7;10(12):2466. doi: 10.3390/healthcare10122466. PMID: 36553990; PMCID: PMC9778322.
- Soares L, Gomes K, dos Santos Silva I. Thyroid Cancer and Quality of Life: A Literature Review. Clin J Obstet Gynecol. 2024; 7:007-013. DOI: 10.29328/journal.cjog.1001156 https://www.obstetricgynecoljournal.com/cjog/article/view/cjog-aid1158/pdf
- Soares L, Correia Silva LC. Breast Cancer: A Review on Quality of Life, Body Image and Environmental Sustainability. World Journal of Cancer and Oncology Research. 2023; 2(2):133–144. https://www.scipublications.com/journal/index.php/wjcor/article/view/826
- Soares L, Vasconcelos R, Faria AL. Oncological Disease in Metastatic Breast Neoplasia and Palliative Care: A Review. World Journal of Cancer and Oncology Research. 2023; 2(2):122–132. https://www.scipublications.com/journal/index.php/wjcor/article/view/802
- Almeida V, Pires D, Silva M, Teixeira M, Teixeira RJ, Louro A, Dinis MAP, Ferreira M, Teixeira A. Dermatological Side Effects of Cancer Treatment: Psychosocial Implications-A Systematic Review of the Literature. Healthcare (Basel). 2023 Sep 25;11(19):2621. doi: 10.3390/healthcare11192621. PMID: 37830658; PMCID: PMC10572319.
- Burmeister CA, Khan SF, Schäfer G, Mbatani N, Adams T, Moodley J, Prince S. Cervical cancer therapies: Current challenges and future perspectives. Tumour Virus Res. 2022 Jun; 13:200238. doi: 10.1016/j.tvr.2022.200238. Epub 2022 Apr 20. PMID: 35460940; PMCID: PMC9062473.
- Vermeer WM, Bakker RM, Kenter GG, Stiggelbout AM, Ter Kuile MM. Cervical cancer survivors' and partners' experiences with sexual dysfunction and psychosexual support. Support Care Cancer. 2016 Apr;24(4):1679-87. doi: 10.1007/s00520-015-2925-0. Epub 2015 Sep 28. PMID: 26412245; PMCID: PMC4766206.
- Herzog TJ, Wright JD. The impact of cervical cancer on quality of life--the components and means for management. Gynecol Oncol. 2007 Dec;107(3):572-7. doi: 10.1016/j.ygyno.2007.09.019. Epub 2007 Oct 25. PMID: 17963826.
- Le D, Coriolan Ciceron A, Jeon MJ, Gonzalez LI, Jordan JA, Bordon J, Long B. Cervical Cancer Prevention and High-Risk HPV Self-Sampling Awareness and Acceptability among Women Living with HIV: A Qualitative Investigation from the Patients' and Providers' Perspectives. Curr Oncol. 2022 Jan 26;29(2):516-533. doi: 10.3390/curroncol29020047. PMID: 35200547; PMCID: PMC8870184.
- Conceição J, Bueno G. 101 techniques of cognitive beahvioral therapy. (1st ed.). Ed. UnC. 2020.
- Soares L. Psychology: The science of human behavior – a historical perspective. Diversitas Journal. 2023; ISSN 2525-5215: 8; 3:2526-2537.
- Camacho E, Soares L, Faria AL, Fernandes MC. Healthy Lifestyles in the Elderly: State-of-the-Art. Biomed J Sci & Tech Res. BJSTR. 2023; 51(1)-2023.
- Lee S, Jung S, Jung S, Moon JY, Oh GH, Yeom CW, Son KL, Lee KM, Kim WH, Jung D, Kim TY, Im SA, Lee KH, Shim EJ, Hahm BJ. Psychiatric symptoms mediate the effect of resilience on health-related quality of life in patients with breast cancer: Longitudinal examination. Psychooncology. 2022 Mar;31(3):470-477. doi: 10.1002/pon.5829. Epub 2021 Oct 20. PMID: 34668264.
- Greimel ER, Winter R, Kapp KS, Haas J. Quality of life and sexual functioning after cervical cancer treatment: a long-term follow-up study. Psychooncology. 2009 May;18(5):476-82. doi: 10.1002/pon.1426. PMID: 18702067.
- Djuric Z, Ellsworth JS, Weldon AL, Ren J, Richardson CR, Resnicow K, Newman LA, Hayes DF, Sen A. A Diet and Exercise Intervention during Chemotherapy for Breast Cancer. Open Obes J. 2011;3:87-97. doi: 10.2174/1876823701103010087. PMID: 22238561; PMCID: PMC3253619.
- Rosario JS, Soares L. Psychological Adaptation to the Autoimmune Disease Diabetes Mellitus Type 1 in Adolescence: A Review, Current Research on Diabetes & Obesity Journal. 2023; 17(1): 555955.DOI: 10.19080/CRDOJ.2023.17.555955 · Sep 13, 2023
- Costa DSJ, Mercieca-Bebber R, Rutherford C, Gabb L, King MT. The Impact of Cancer on Psychological and Social Outcomes. Australian Psychologist. 2016; 51(2):89–99. https://doi.org/10.1111/ap.12165
- Lynch J, D'Alton P, Gaynor K. Evaluating the role of perceived injustice in mental health outcomes in cervical cancer care. Support Care Cancer. 2022 Jul;30(7):6215-6223. doi: 10.1007/s00520-022-07060-z. Epub 2022 Apr 21. PMID: 35445867; PMCID: PMC9022611.
- Osann K, Hsieh S, Nelson EL, Monk BJ, Chase D, Cella D, Wenzel L. Factors associated with poor quality of life among cervical cancer survivors: implications for clinical care and clinical trials. Gynecol Oncol. 2014 Nov;135(2):266-72. doi: 10.1016/j.ygyno.2014.08.036. Epub 2014 Sep 3. PMID: 25192629; PMCID: PMC4479396.
- Tadesse SK. Socio-economic and cultural vulnerabilities to cervical cancer and challenges faced by patients attending care at Tikur Anbessa Hospital: a cross sectional and qualitative study. BMC Womens Health. 2015 Sep 16;15:75. doi: 10.1186/s12905-015-0231-0. PMID: 26376638; PMCID: PMC4571133.
- Soares L, Leal T, Faria AL, Aguiar A, Carvalho C. Social Determinants of cardiovascular, Novel Practices in Med Study. 2023; 1(2): NPMS.000508.
- Wenzel L, DeAlba I, Habbal R, Kluhsman BC, Fairclough D, Krebs LU, Anton-Culver H, Berkowitz R, Aziz N. Quality of life in long-term cervical cancer survivors. Gynecol Oncol. 2005 May;97(2):310-7. doi: 10.1016/j.ygyno.2005.01.010. PMID: 15863123.
- Soares L, Cruz O, Oliveira F, Lucas CV, Neto F. Psychosocial Predictors of Love Satisfaction Among College Students from Madeira. Journal of Relationships Research. 2020; 11:e6. doi:10.1017/jrr.2020.4
- Ferrandina G, Mantegna G, Petrillo M, Fuoco G, Venditi L, Terzano S, Moruzzi C, Lorusso D, Marcellusi A, Scambia G. Quality of life and emotional distress in early stage and locally advanced cervical cancer patients: A prospective, longitudinal study. Gynecologic Oncology. 2012; 124(3):389-394. https://doi.org/10.1016/j.ygyno.2011.09.041
- Coleman D, Hurtado-de-Mendoza A, Montero A, Sawhney S, Wang JH, Lobo T, Graves KD. Stigma, social support, and spirituality: associations with symptoms among Black, Latina, and Chinese American cervical cancer survivors. J Cancer Surviv. 2022 Nov 22:10.1007/s11764-022-01283-z. doi: 10.1007/s11764-022-01283-z. Epub ahead of print. PMID: 36417116; PMCID: PMC10200827.
- Santos PJ, Soares, Faria AL. Narrative therapy as an innovative approach to Anorexia Nervosa treatment: a literature review, Journal of Poetry Therapy. 2023;
- Soares L, Barbosa P, Aguiar A, Pinto M. Clinical Psychology and the new technological challenges after Covid-19, Novel Practices in Medical study. 2023; 1,2: NPMS. 000510.2023
- Chona EZ, Msengi EA, Gosse RA, Ambikile JS. The lived experiences and caring needs of women diagnosed with cervical cancer: A qualitative study in Dar es Salaam, Tanzania. PLoS One. 2023 Aug 10;18(8):e0289925. doi: 10.1371/journal.pone.0289925. PMID: 37561728; PMCID: PMC10414621.
- Soares L, Cabral S, Faria AL. Mental Health and Obesity in Childhood and Adolescence, Novel Practices in Med Study. 2023; 1(2): NPMS.000509.
- Hall K, Gibbie T, Lubman DI. Motivational interviewing techniques - facilitating behaviour change in the general practice setting. Aust Fam Physician. 2012 Sep;41(9):660-7. PMID: 22962639.
- Jacobs EA, Rathouz PJ, Karavolos K, Everson-Rose SA, Janssen I, Kravitz HM, Lewis TT, Powell LH. Perceived discrimination is associated with reduced breast and cervical cancer screening: The Study of Women's Health Across the Nation (SWAN). J Womens Health (Larchmt). 2014 Feb;23(2):138-45. doi: 10.1089/jwh.2013.4328. Epub 2013 Nov 21. PMID: 24261647; PMCID: PMC3922246.