More Information
Submitted: January 23, 2024 | Approved: February 02, 2024 | Published: February 05, 2024
How to cite this article: Soares L, Gomes K, dos Santos Silva I. Thyroid Cancer and Quality of Life: A Literature Review. Clin J Obstet Gynecol. 2024; 7: 007-013.
DOI: 10.29328/journal.cjog.1001156
Copyright License: © 2024 Soares L, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Thyroid cancer; Quality of life; Psychological intervention
Thyroid Cancer and Quality of Life: A Literature Review
Luísa Soares1*  , Karina Gomes1
, Karina Gomes1  and Inês dos Santos Silva2
and Inês dos Santos Silva2 
1Psychology Department, FAH, University of Madeira, Portugal
2Instituto Superior Técnico, Portugal
*Address for Correspondence: Luísa Soares, Psychology Department, FAH, University of Madeira, Portugal, Email: [email protected]
Thyroid cancer, characterized by the development of malignant tumors in the cells of the thyroid gland, impacts the quality of life and well-being of diagnosed patients. This article explores different aspects of this type of cancer, including everything from its typologies, incidence, causes, and risk factors to symptoms, diagnostic methods, and treatment options. Furthermore, the impact on Health-Related Quality of Life (HRQoL) is addressed, highlighting that, although the prognosis is generally favorable, patients can experience significant negative repercussions. Therefore, the need for further investigation into the priorities of psychological intervention with the population with this problem is emphasized.
Thyroid cancer refers to the formation of malignant tumors in the cells of the thyroid gland, an endocrine gland, located in the lower front of the neck [1,2]. It is formed by two lobes (the right and the left) joined by the isthmus. The function of the thyroid gland is to produce thyroid hormones, which help the body use energy, maintain an adequate body temperature, as well as maintain the proper functioning of some organs [1]. Furthermore, the normal thyroid gland is composed of two types of cells: follicular cells, involved in the production of thyroid hormones, and C, or particular cells, which produce the hormone calcitonin [2].
Regarding the types of thyroid cancer, these are associated with the two types of cells mentioned above, with medullary thyroid cancer being related to C cells. In contrast, the follicular, papillary, and anaplastic types are linked to follicular cells.
Therefore, the most prevalent is papillary thyroid cancer, which represents approximately 70% to 80% of thyroid cancer cases, followed by the follicular type, which represents approximately 10% to 15% of cases. This medullary type represents approximately 2%; finally, the anaplastic type constitutes less than 2% of cases [1]. When Exploring each type, it is interesting to note that the papillary type has a greater risk of spreading to the lymph nodes in the neck, while the follicular type has a greater risk of metastasizing through the blood to distant organs, such as lungs and bones; around 25% of cases of medullary thyroid cancer have a hereditary component and the anaplastic type is the most aggressive, occurring in more advanced stages of cancer, with a low probability of responding to treatment [1].
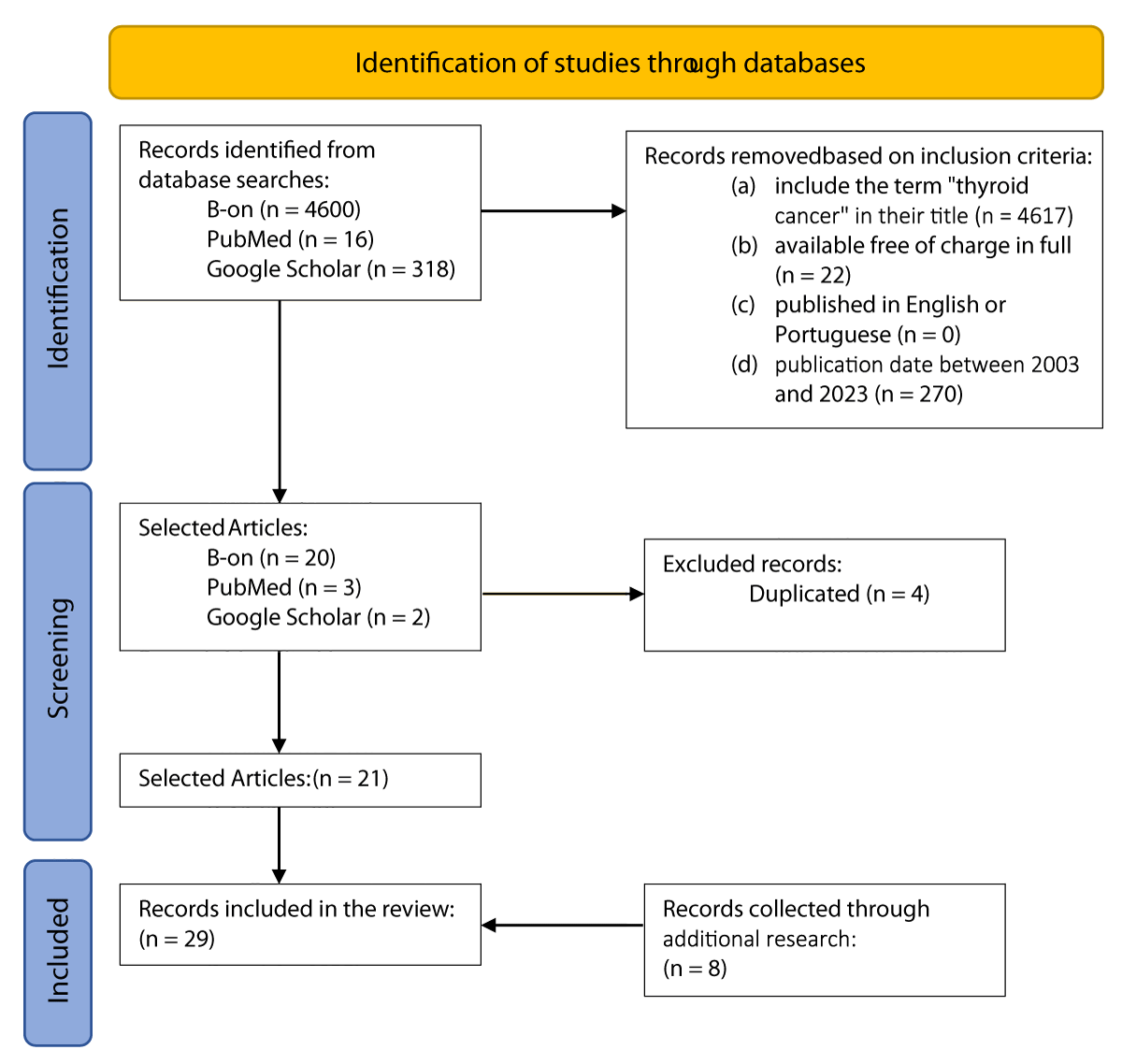
Concerning the methodology used in the present study, a search was carried out in the literature published between the years 2003 and 2023 in the databases "B-on," "PubMed," and "Google Scholar" using the keywords “ thyroid cancer," "psychotherapy," "treatment," "risk factors," "quality of life" and "epidemiology." This research was carried out with the help of the Boolean operators "AND" and "OR" and the truncators" and it took place between September 30th and November 5th, 2023. As inclusion criteria, studies would have to: (a) include the term "thyroid cancer" in its title, (b) be available in full for free and, (c) be published in English or Portuguese and (d) have a publication date between the years 2003 and 2023. They excluded studies in review format and those that did not meet the previously mentioned criteria. Therefore, 19 documents were considered for analysis (Figure 1), the main conclusions of which are presented in Table 1. Furthermore, additional records were included, selected from additional research, to make this study more complete, using 29 records (Figure 1).
Figure 1: PRISMA diagram for the selection of research works for the study.
| Table 1: Main conclusions of the articles. | |||
| Authors | Methodology | Target Group | Main conclusions |
| Barbus, et al. 2018 [3] | Transversal Study | Patients with thyroid cancer | - Fatigue is the main factor relating to physical well-being. - Initial diagnostic and cirurgic impact on psychological wellbeing |
| Büel-Drabe, et al. 2018 [4] |
Transversal Study | Patients with thyroid cancer and their partners | - cancer diagnostic changed significantly in 44,7% of patients and 42,1% of their partners - negative changes associated with higher levels of depression and lower quality of relationship |
| Costa & Pakenham 2012 [5] | Questionnaires (154 patients, 32 partners) | Patients with thyroid cancer and their partners | - Perceived benefit associated with more significant positive affect and positive changes in health behavior. - Perceived benefit related to better results in higher-order cognitive and motivational states (HOCMS) of adaptation. |
| Drabe, et al. 2016 [6] | Online study with standard Questionnaires | Patients with thyroid cancer and their partners | - Impact of diagnosis and treatment associated with anxiety and fatigue on patients and partners. - A simple question can identify patients at risk. |
| Duan, et al. 2015 [4] | Literature Review | Patients with thyroid cancer | - Recognition of QoL as a central point in treating thyroid cancer, highlighting the need for constant assessment. - Challenges and importance of balancing medical, psychological, and patient perspectives, emphasizing the relevance of Patient Reported Outcomes (PROs) in research and clinical practice. |
| Gamper, et al. 2015 [8] | Routine Monitoring of QVRS | Patients with thyroid cancer | Clinically significant differences regarding fatigue and the function role compared to the general population. - Favorable prognosis does not directly translate into good HRQoL. |
| Hamurcu, et al. 2022 [9] |
Psychiatric Assessment of Distress | Patients with Papillary Thyroid Cancer | - High prevalence of distress (78%). - Distress associated with psychopathology, low and high income, physical comorbidity, high anxiety, and depression. |
| Henry, et al. 2018 [10] |
Quasi-Experimental Study | Thyroid Cancer Patients (ThyCa) | - Assessment of the Impact of the ITCA-ThyCa Program showed better results in the intervention group. - Hospital resources must consider aspects beyond the medical trajectory. |
| Hou, et al. 2021 [11] | Genomic and Functional Analysis | Patients with thyroid cancer | - Identification of mutated genes associated with the ineffectiveness of radioactive iodine therapy. - miR-146b-3p was identified as a potential therapeutic target to improve the efficacy of radioactive iodine therapy. |
| Jarząb, et al. 2016 [12] | Guidelines Review (Poland) |
Health Professionals | - Revised guidelines approved by the Scientific Committee based on international guidelines. - Emphasis on therapeutic optimization and updated criteria for post-treatment monitoring. |
| Jarząb, et al. 2022 [13] | Adaptation of International Guidelines (Poland) | Health Professionals | - Therapeutic adaptation in cases of low-risk thyroid carcinoma. - Modification of indications for postoperative radioactive iodine and criteria for postoperative treatment. |
| Javaloyes, et al. 2022 [14] |
Non-Randomized Controlled Study | Patients with thyroid cancer | - Significant reduction in anxiety and depression in the experimental group (GE) compared to the control group (CG). - Significant improvement in the general psychological wellbeing index in the EG compared to the CG. |
| Kreissl, et al. 2014 [15] | Delphi panel with nine clinical experts | Health Professionals | - Supportive care for CMT includes symptom relief to maintain quality of life. - The total average cost of supportive care per patient/year is estimated at €9,248. |
| Liu, et al. 2023 [16] | Study with Random Groups | Patients with thyroid cancer | - Effective psychological intervention in improving the psychological distress of patients with DTC during radioactive iodine therapy. |
Incidence and prevalence
It is three times more common in women; thyroid cancer is also more prevalent in women between 35 and 64 years and between men aged between 45 and 74 years [1,22,23].
In terms of global incidence, thyroid cancer is in ninth position in the ranking, compared to other cancers [23]. In 2020, 586202 new cases were presented, representing 3.2% of the number of cancer cases this year [23].
Regarding incidence data in Portugal, thyroid cancer is the third most common type of cancer, in terms of new cases, in women [24]. In 2010, mortality rates were 0.32/100,000 in men and 0.37/100,000 in women, with 32 and 62 cases of death recorded, respectively [25]. Furthermore, in 2018, 367 new cases were registered in men and 1275 in women [22]. Table 1.
Causes and risk factors
Most people with thyroid cancer have no obvious risk factors, and the exact reason for its development remains unknown in most cases [26]. Possible causes and risk factors may include exposure to high doses of ionizing radiation, family history, age (individuals over 40), radioactivity during natural disasters, obesity, smoking, hormonal exposures, and environmental pollution [1,27,28].
Furthermore, a Mendelian randomization study indicated an association between an increase in genetically predicted height and an increased risk of developing thyroid cancer [18,29].
Symptomatology
Generally, symptoms of thyroid cancer include the presence of a thyroid nodule or lump, but they often do not cause other symptoms [1]. Additionally, possible symptoms may include difficulty breathing, swallowing, or a "itchy throat" sensation; and hoarseness (less common, occurs if thyroid cancer targets the nerve that controls your vocal cords) [1].
Some treatments commonly lead to new symptoms, such as interruption or reduction of hormonal treatments before treatment with radioiodine or, in the case of thyrotropin (TSH, a thyroid-stimulating hormone), suppressive therapy treatments after radioiodine treatment, which can result in symptoms such as restlessness, nervousness and palpitations [7,30]. These last symptoms can persist for the rest of the patient's life [7].
Treatments can cause social, cognitive, and emotional problems, sometimes worrying these patients [7,30]. Taking into account that thyroid cancer involves hormonal disharmonies and that this can cause emotional "roller coasters" [7,31] suggests that monitoring by a psychologist can help the patient deal with these symptoms.
Diagnosis
There are several methods used in the diagnosis process and complementary exams [2]. However, it is essential to note that thyroid cancer can only be diagnosed with certainty after surgical removal of the nodule [1].
Thus, some of these methods include [2]:
- Clinical and History Examination, which aims to identify thyroid nodules through palpation and evaluate the patient's clinical history;
- Thyroid Function Tests, responsible for measuring thyroid-stimulating hormone (TSH) in the blood;
- Laryngoscopy (direct or indirect), which is essential both in the preoperative evaluation and in the initial evaluation of a thyroid nodule;
- High-resolution ultrasound, capable of detecting multiple nodules that may not be palpable, being used to perform Fine Needle Aspiration (FNA);
- Fine Needle Aspiration (FNA), a technique used to obtain samples of cells from the thyroid nodule for cytological evaluation;
- Molecular markers have been evaluated in FNA samples to improve diagnostic accuracy.
There are a variety of procedures used in diagnosis, commonly, in the case of suspected thyroid cancer, a physical examination is carried out accompanied by ultrasound/ultrasound, followed by a biopsy if previous tests show evidence of the presence of a nodule and finally, is passed on to surgical treatment if justified by the biopsy results [1].
Thyroid nodules are widespread, but less than 1 in 10 will be thyroid cancer. Ultrasound reveals thyroid nodules in 20 to 76% of cases, with only 5% - 15% associated with thyroid cancer [32].
Treatment
After a diagnosis confirms the need for treatment, methods to continue the process are considered. The most common is surgery, which can range from removing just the affected thyroid lobe to total thyroidectomy, usually followed by radioactive iodine therapy to eliminate any remaining thyroid tissue and destroy residual cancer cells [1,2]. Additionally, additional methods such as external beam radiation therapy, chemotherapy, biological therapies, and medication may be used to treat more advanced thyroid cancer that does not respond to surgery and radioactive iodine therapy [1]. However, these additional methods have a limited role in treating thyroid cancer [1]. From a healthcare system perspective, the costs associated with Basic Supportive Care (BSC) are substantial and equivalent to those found in other tumor conditions [15]. Therefore, Kreissl, et al. in 2014 [15] provided a foundation for future health economic analyses within this context.
Finally, it is important to highlight that research to develop more effective medications to treat thyroid cancer is ongoing. A recent example is the study by [11] who identified anti-miR-146b-3p as a promising potential cancer drug, especially in the treatment of differentiated thyroid cancer.
Quality of life
Health-Related Quality of Life (HRQoL) integrates the physical, psychological, emotional, and social consequences that impact the individual [33-35]. In the case of thyroid cancer, defining this construct proved to be a particularly challenging task, as its symptoms are diverse and depend on the individual's hormonal status, and can range from symptoms such as physical discomfort to emotional discomfort [7].
The study by [20] revealed that, in patients with differentiated thyroid cancer, HRQoL is significantly reduced when they are in the process of preparing for diagnostic or therapeutic procedures. The anxiety of these patients is considerably more frequent than that of the general population [20].
In this case, it has been reported that patients with thyroid cancer often face more severe psychological challenges compared to patients with poorer prognoses [7,36]. A possible explanation for this event is that this last group is focused on managing treatments and their side effects, fighting for their survival daily [7]. Additionally, thyroid cancer patients appear to experience symptoms of distress at a level similar to or greater than cancer patients in general [10].
In this sense, although the rate of thyroid cancer survivors has been increasing worldwide and its impact on HRQoL is generally considered lower compared to other cancers, such as head and neck, due to the application of less invasive treatments, patients still feel impacts on their HRQoL [33,37]. These often experience significant negative repercussions after cancer diagnosis despite generally having a more favorable prognosis [33,38] and highlighting that a favorable prognosis does not directly translate into good HRQoL for these patients [8].
Thus, highlights that the HRQoL of individuals diagnosed with thyroid cancer is often equivalent to that of the healthy population [33]. This comparison, however, is seen as an analysis that underestimates the true impact of thyroid cancer on HRQOL [33]. It may be attributed to the tendency of clinicians to neglect concerns related to HRQoL in this group, focusing on the favorable prognosis [7]. Therefore, the assessment of HRQoL in this population may not be usual since there is a misconception that the study of quality of life in this group of patients is more than in other oncological cases [7].
Therefore, it is essential to recognize the experience of being diagnosed with thyroid cancer, even in the face of a favorable medical prognosis [10,39]. This understanding seeks to contribute to a deeper integration of this situation into patients' lives [10,39].
In the case of thyroid cancer, HRQoL concerns may arise following adverse treatment outcomes [28]. Symptoms commonly associated with decreased HRQOL include insomnia, sleep disorders, memory problems, difficulty concentrating, and neuromuscular complaints [33,38].
Furthermore, apprehension regarding the possibility of cancer returning is a widespread concern for all types of cancer and is also an anxiety present in the context of thyroid cancer, again, even when the prognosis is favorable [33].
Patients must have access to information about how their quality of life can be affected by this diagnosis and the treatment that accompanies it [7,40,41]. Furthermore, this information is essential for developing intervention strategies to improve HRQoL [7].
Psychological well-being is influenced by treatment, the possibility of the emergence of another cancer or the recurrence/metastasis of the subsequent malignant disease, and future diagnostic tests [3,40,41].
Regarding the social aspect of HRQoL, [4,41,42]] explored the impact of thyroid cancer on patient-partner dynamics, as well as sexual activity. They identified that a significant portion of their sample reported perceptions of negative or mixed changes in relationships, along with a decrease in the frequency of sexual activity [4]). The results lead the authors to consider that such changes may be indicative of increased anxiety and depression, as well as a lower quality of relationships in patients with differentiated thyroid carcinoma (DTC). Another study conducted by [6] reveals that, in general, it is patients, and not their partners, who face symptoms of anxiety after thyroid cancer diagnosis and treatment. Furthermore, they highlight that patients and their partners feel overwhelmed in various ways at the time of diagnosis and treatment, which is expressed predominantly through fatigue [6]. They also identified that, when perceived as a burden, this feeling was associated with depressive symptoms, anxiety, and fatigue, especially in women. In contrast, the predominant symptom in men was just fatigue [6].
Furthermore, this social dimension can be affected by persistent restrictions on the resumption of daily life, manifesting itself in the interruption or difficulty in domestic activities, in the reduction of weekly working hours due to increased fatigue, and in the impact that cancer has on the patient's family dynamics [3,8,17]. Additionally, if adequate management of the patient's suffering is not carried out, the problem of isolation may arise [3].
Additionally, the treatment of differentiated thyroid cancer has significant emotional repercussions for the patient [14]. As previously mentioned, radioactive iodine therapy requires isolation, making this period challenging for the physician [9]. Thus, the prevalence of distress in patients is high even before this therapy [9]. [10] highlight that although medical care for patients with thyroid cancer is well-established in medicine, the patient experience does not reflect this simplicity. Medical care alone is insufficient to meet the needs for monitoring and social support they perceive.
The study by [5] analyzed correlations between Benefit Found (BF) and psychological adjustment in thyroid cancer with demographic variables. They found that older age is associated with greater self-acceptance and spiritual well-being. However, female sex is related to less positive change in substance use and higher levels of stress linked to cancer. Furthermore, having a partner or a higher income was associated with a greater purpose in life. In summary, this study revealed that age and gender play crucial roles in the experiences and adjustment of cancer patients, impacting aspects ranging from psychological well-being to quality of life and the impact on professional life [5].
It is positive to realize that studies have been carried out to understand the influence of treatments on the quality of life of these patients. For example, the study by [21] sought to understand whether different types of surgery affect a patient's quality of life by comparing the effects of hemorrhoidectomy and complete thyroidectomy in patients with differentiated thyroid cancer. It was concluded that the type of surgery does not appear to have a distinct influence on quality of life in general [21].
In summary, psychological care and rehabilitation play an essential role in the management of thyroid cancer, ensuring adequate emotional and social support for patients during and after the completion of cancer therapy to achieve complete recovery in terms of psychosocial [12,41]. In this sense, the development of psychological intervention programs is encouraged, aiming at rehabilitation and a complete return to patients' social roles before treatment [13,41]. Each phase in the treatment of patients with thyroid cancer can impact different facets of the overall quality of life. As healthcare professionals, we must recognize that we are responsible for providing an accurate diagnosis, appropriate treatment, and care to restore balance in our patient's quality of life [3].
Psychological intervention
Implementing an effective psychological intervention that is well received by patients requires an essential understanding of the priorities they attribute to quality of life. In the study by [19], fatigue emerged as a central concern for several groups analyzed, highlighting the quality of sleep and sudden episodes of tiredness. Additionally, the issue of employment was identified as a priority by patients, indicating a reluctance to abandon work as they seek to remain professionally active for as long as possible [19]. Lastly, fear of progression was noted as the third predominant concern among most patients [19]. [16] emphasize the advantages of individualized communication in intervention to alleviate psychological suffering. They describe how psychological intervention has the potential to significantly improve the suffering of patients undergoing radioactive iodine treatment for differentiated thyroid cancer [16,39]. This intervention demonstrated effectiveness in reducing anxiety, depression, and fatigue associated with cancer, contributing to improving the mood of these patients.
Furthermore, the psycho-oncological approach, focused on counseling on depression, quality of life, anxiety, and well-being in patients with differentiated thyroid cancer, was highlighted by [14] as capable of significantly improving these factors.
Thyroid cancer is a complex condition affecting the thyroid gland, classified into papillary, follicular, medullary, and anaplastic. The global incidence, especially in women aged 35 to 64, highlights its relevance. In addition to physical challenges, thyroid cancer impacts patients' Quality of Life (QOL), addressed by Health-Related Quality of Life (HRQoL), considering physical, psychological, and social implications. A significant reduction in HRQOL is recognized in literature, during diagnostic and therapeutic procedures with high levels of anxiety. Patients with less favorable prognoses may cope better with the psychological impact, suggesting emotional complexity. Recognizing the experience of diagnosis, even with a positive prognosis, is crucial, and highlights the importance of psychological support to deal with emotional challenges. Psychological intervention is essential in reducing anxiety, depression, and fatigue associated with treatment. Therefore, thyroid cancer management goes beyond medical treatment, integrating approaches to ensure complete recovery and resumption of daily activities. Therefore, we emphasize the need for further investigations into intervention priorities for this population and the publication of updated incidence and mortality data for the Portuguese population.
- American Thyroid Association (2022). Thyroid Cancer (Papillary and Follicular) [Brochure]. https://www.thyroid.org/wp-content/uploads/patients/brochures/ThyroidCancer_brochure.pdf
- Carling T, Udelsman R. Thyroid cancer. Annu Rev Med. 2014;65:125-37. doi: 10.1146/annurev-med-061512-105739. Epub 2013 Nov 20. PMID: 24274180.
- Barbus E, Pestean C, Larg MI, Gabora K, Cheptea M, Bonci EA, Badulescu C, Piciu D. Quality of life in thyroid cancer: a questionnaire-based study. Journal of Evidence-Based Psychotherapies. 2018; 18(1): 1-20. https://jebp.psychotherapy.ro/wp-content/uploads/2021/03/JEBP_18_1_1.pdf
- Büel-Drabe N, Steinert H, Moergeli H, Weidt S, Seiler A, Jenewein J. Thyroid cancer has a small impact on patient-partner relationships and their frequency of sexual activity. Palliat Support Care. 2018 Jun;16(3):335-346. doi: 10.1017/S1478951517000384. Epub 2017 May 31. PMID: 28560941.
- Costa RV, Pakenham KI. Associations between benefit finding and adjustment outcomes in thyroid cancer. Psychooncology. 2012 Jul;21(7):737-44. doi: 10.1002/pon.1960. Epub 2011 Mar 17. PMID: 21416554.
- Drabe N, Steinert H, Moergeli H, Weidt S, Strobel K, Jenewein J. Perception of treatment burden, psychological distress, and fatigue in thyroid cancer patients and their partners - effects of gender, role, and time since diagnosis. Psychooncology. 2016 Feb;25(2):203-9. doi: 10.1002/pon.3903. Epub 2015 Jul 15. PMID: 26179844.
- Duan H, Gamper E, Becherer A, Hoffmann M. Quality of life aspects in the management of thyroid cancer. Oral Oncol. 2015 Jun;51(6):S1-5. doi: 10.1016/j.oraloncology.2015.03.008. Epub 2015 Apr 25. PMID: 25920747.
- Gamper EM, Wintner LM, Rodrigues M, Buxbaum S, Nilica B, Singer S, Giesinger JM, Holzner B, Virgolini I. Persistent quality of life impairments in differentiated thyroid cancer patients: results from a monitoring programme. Eur J Nucl Med Mol Imaging. 2015 Jul;42(8):1179-88. doi: 10.1007/s00259-015-3022-9. Epub 2015 Mar 13. PMID: 25771905; PMCID: PMC4480943.
- Hamurcu HD, Özer İ, Uçmak G, Çayköylü A, Yüncü ÖA. Distress and related factors in patients with papillary thyroid cancer just before the radioactive iodine therapy: Does perceived social support predict distress? Turkish Journal of Clinical Psychology. 2022; 25(3): 252-259. https://doi.org/10.5505/kpd.2022.65983
- Henry M, Frenkiel S, Chartier G, MacDonald C, Payne RJ, Black MJ, Mlynarek AM, Zeitouni A, Kost K, Loiselle C, Ehrler A, Rosberger Z, Tamilia M, Chang YX, de la Mora C, Arbaud C, Hier MP. Thyroid cancer patients receiving an interdisciplinary team‐based care approach (ITCA‐ThyCa) display better outcomes: Program evaluation results indicate a need for further integrated care and support. Psycho‐Oncology. 2018;27(3): 937-945. https://doi.org/10.1002/pon.4590
- Hou S, Xie X, Zhao J, Wu C, Li N, Meng Z, Cai C, Tan J. Downregulation of miR-146b-3p Inhibits Proliferation and Migration and Modulates the Expression and Location of Sodium/Iodide Symporter in Dedifferentiated Thyroid Cancer by Potentially Targeting MUC20. Front Oncol. 2021 Jan 8;10:566365. doi: 10.3389/fonc.2020.566365. PMID: 33489878; PMCID: PMC7821393.
- Jarząb B, Dedecjus M, Handkiewicz-Junak D, Lange D, Lewiński A, Nasierowska-Guttmejer A, Ruchała M, Słowińska-Klencka D, Nauman J, Adamczewski Z, Bagłaj M, Bałdys-Waligórska A, Barczyński M, Bednarczuk T, Cichocki A, Czarniecka A, Czepczyński R, Gawlik A, Hubalewska-Dydejczyk A, Jażdżewski K, Kamiński G, Karbownik-Lewińska M, Kos-Kudła B, Kułakowski A, Kuzdak K, Łącka K, Małecka-Tendera E, Niedziela M, Pomorski L, Sporny S, Stojcev Z, Syrenicz A, Włoch J, Krajewska J, Szpak-Ulczok S, Kalemba M, Buziak-Bereza M. Diagnostics and Treatment of Thyroid Carcinoma. Endokrynol Pol. 2016;67(1):74-107. doi: 10.5603/EP.2016.0011. PMID: 26884119.
- Jarząb B, Dedecjus M, Lewiński A, Adamczewski Z, Bakuła-Zalewska E, Bałdys-Waligórska A, Barczyński M, Biskup-Frużyńska M, Bobek-Billewicz B, Bossowski A, Buziak-Bereza M, Chmielik E, Czarniecka A, et al. Diagnosis and treatment of thyroid cancer in adult patients - Recommendations of Polish Scientific Societies and the National Oncological Strategy. 2022 Update [Diagnostyka i leczenie raka tarczycy u chorych dorosłych - Rekomendacje Polskich Towarzystw Naukowych oraz Narodowej Strategii Onkologicznej. Aktualizacja na rok 2022]. Endokrynol Pol. 2022;73(2):173-300. doi: 10.5603/EP.a2022.0028. PMID: 35593680.
- Javaloyes N, Crespo A, Redal MC, Brugarolas A, Botella L, Escudero-Ortiz V, Sureda M. Psycho-oncological intervention through counseling in patients with differentiated thyroid cancer in treatment with radioiodine (COUNTHY, NCT05054634): a non-randomized controlled study. Frontiers in Psychology. 2022; 13: https://doi.org/10.3389/fpsyg.2022.767093
- Kreissl MC, Jacob C, Führer D, Karges W, Luster M, Lux MP, Mann K, Mittendorf T, Schott M, Spitzweg C, Schmoll HJ. Best supportive care from the conservative/non-surgical perspective and its costs in the treatment of patients with advanced medullary thyroid cancer: results of a Delphi panel. Oncology Research and Treatment. 2014; 37(6): 316-322. https://doi.org/10.1159/000362613
- Liu YB, Zuo LJ, Liu YC, Li YP, Xin YC, Zhang HY, Hou LY. Effect of Psychological Intervention on Differentiated Thyroid Cancer Patients in the Treatment with Radioactive Iodine. Patient Prefer Adherence. 2023 Mar 18;17:731-738. doi: 10.2147/PPA.S400832. PMID: 36970302; PMCID: PMC10032163.
- Neudeck MR, Steinert H, Moergeli H, Weidt S, Seiler A, Strobel K, Jenewein J, Drabe N. Work ability and return to work in thyroid cancer patients and their partners: a pilot study. Psychooncology. 2017 Apr;26(4):556-559. doi: 10.1002/pon.4154. Epub 2016 May 11. PMID: 27167216.
- Papadopoulou A, Åsvold BO, Burgess S, Kuś A, Medici M, Sterenborg R, Teumer A, Deloukas P, Marouli E. Height, Autoimmune Thyroid Disease, and Thyroid Cancer: A Mendelian Randomization Study. Thyroid. 2023 Dec;33(12):1476-1482. doi: 10.1089/thy.2023.0272. Epub 2023 Oct 26. PMID: 37772697; PMCID: PMC7615364.
- Singer S, Husson O, Tomaszewska IM, Locati LD, Kiyota N, Scheidemann-Wesp U, Hofmeister D, Winterbotham M, Brannan C, Araújo C, Gamper EM, Kulis D, Rimmele H, Andry G, Licitra L. Quality-of-life priorities in patients with thyroid cancer: a multinational European organization for research and treatment of cancer phase I study. Thyroid; 2016;26(11): 1605-1613. https://doi.org/10.1089/thy.2015.0640
- Tagay S, Herpertz S, Langkafel M, Erim Y, Bockisch A, Senf W, Görges R. Health-related Quality of Life, depression and anxiety in thyroid cancer patients. Qual Life Res. 2006 May;15(4):695-703. doi: 10.1007/s11136-005-3689-7. PMID: 16688502.
- Yang X, Yang Q, Tang Y, Ma J, Ye H. Impact of the Extent of Thyroidectomy on Quality of Life in Differentiated Thyroid Cancer Survivors: A Propensity Score Matched Analysis. Cancer Manag Res. 2021 Sep 7;13:6953-6967. doi: 10.2147/CMAR.S321988. PMID: 34522138; PMCID: PMC8434861.
- Miranda A, Mayer-da-Silva A, Glória L, Brito C. National Oncological Registry: of All Tumors in the Resident Population in Portugal, in 2018. National Oncological Registry. https://ron.min-saude.pt/media/2196/2021-0518_publica%C3%A7%C3%A3o-ron_2018.pdf
- World Cancer Research Fund International (2022) Worldwide cancer data: Global cancer statistics for the most common cancers worldwide. https://www.wcrf.org/cancer-trends/worldwide-cancer-data/
- Ferlay J, Colombet M, Soerjomataram I, Dyba T, Randi G, Bettio M, Gavin A, Visser O, Bray F. Cancer incidence and mortality patterns in Europe: Estimates for 40 countries and 25 major cancers in 2018. Eur J Cancer. 2018 Nov;103:356-387. doi: 10.1016/j.ejca.2018.07.005. Epub 2018 Aug 9. PMID: 30100160.
- La Vecchia C, Malvezzi M, Bosetti C, Garavello W, Bertuccio P, Levi F, Negri E. Thyroid cancer mortality and incidence: a global overview. Int J Cancer. 2015 May 1;136(9):2187-95. doi: 10.1002/ijc.29251. Epub 2014 Oct 13. PMID: 25284703.
- Xu Y, Wu D, Wu W, Jiang J, Xi C, Ye N, Wang Y, Xu X. Diagnostic value of cytology, thyroglobulin, and combination of them in fine-needle aspiration of metastatic lymph nodes in patients with differentiated thyroid cancer: A systematic review and network meta-analysis. Medicine (Baltimore). 2019 Nov;98(45):e17859. doi: 10.1097/MD.0000000000017859. PMID: 31702649; PMCID: PMC6855606.
- Soares L, Correia Silva LC. Breast Cancer: A Review on Quality of Life, Body Image and Environmental Sustainability. World Journal of Cancer and Oncology Research.2023; 2(2): 133–144. https://www.scipublications.com/journal/index.php/wjcor/article/view/826
- Almeida V, Pires D, Silva M, Teixeira M, Teixeira RJ, Louro A, Dinis MAP, Ferreira M, Teixeira A. Dermatological Side Effects of Cancer Treatment: Psychosocial Implications-A Systematic Review of the Literature. Healthcare (Basel). 2023 Sep 25;11(19):2621. doi: 10.3390/healthcare11192621. PMID: 37830658; PMCID: PMC10572319.
- Silva S, Bártolo A, Santos IM, Paiva D, Monteiro S. Validation of the Portuguese Version of the Fear of Progression Questionnaire-Short Form (FoP-Q-SF) in Portuguese Cancer Survivors. Healthcare (Basel). 2022 Dec 7;10(12):2466. doi: 10.3390/healthcare10122466. PMID: 36553990; PMCID: PMC9778322.
- Lee S, Jung S, Jung S, Moon JY, Oh GH, Yeom CW, Son K, Lee K, Kim W, Jung D, Kim T, Im S, Lee K, Shim E, Hahm BJ. Psychiatric symptoms mediate the effect of resilience on health-related quality of life in patients with breast cancer: Longitudinal examination. Psycho-Oncology. 2022; 31(3): 470-477. https://doi.org/10.1002/pon.5829
- Conceição J, Bueno G. (2020). 101 cognitive behavioral therapy techniques. (1st ed.). Editora UnC.
- National Health Service (2018) Hospital Referral Network: Endocrinology and nutrition. Ministry of Health, Portuguese Republic. https://www.sns.gov.pt/wp-content/uploads/2022/04/RRH-Endocrinologia-e-Nutric%CC%A7a%CC%83o.pdf
- Walshaw EG, Smith M, Kim D, Wadsley J, Kanatas A, Rogers SN. Systematic review of health-related quality of life following thyroid cancer. Tumori. 2022 Aug;108(4):291-314. doi: 10.1177/03008916211025098. Epub 2021 Aug 13. PMID: 34387109; PMCID: PMC9310144.
- Hall K, Gibbie T, Lubman DI. Motivational interviewing techniques - facilitating behaviour change in the general practice setting. Aust Fam Physician. 2012 Sep;41(9):660-7. PMID: 22962639.
- Djuric Z, Ellsworth JS, Weldon AL, Ren J, Richardson CR, Resnicow K, Newman LA, Hayes DF, Sen A. A Diet and Exercise Intervention during Chemotherapy for Breast Cancer. Open Obes J. 2011;3:87-97. doi: 10.2174/1876823701103010087. PMID: 22238561; PMCID: PMC3253619.
- Soares L, Vasconcelos R, Faria AL. Oncological Disease in Metastatic Breast Neoplasia and Palliative Care: A Review. World Journal of Cancer and Oncology Research. 2023; 2(2): 122–132. https://www.scipublications.com/journal/index.php/wjcor/article/view/802
- Rosario JS, Soares L. Psychological Adaptation to the Autoimmune Disease Diabetes Mellitus Type 1 in Adolescence: A Review, Current Research on Diabetes & Obesity Journal. 2023; 17(1): 555955. DOI: 10.19080/CRDOJ.2023.17.555955 · Sep 13, 2023
- Roth EM, Lubitz CC, Swan JS, James BC. Patient-Reported Quality-of-Life Outcome Measures in the Thyroid Cancer Population. Thyroid. 2020 Oct;30(10):1414-1431. doi: 10.1089/thy.2020.0038. Epub 2020 May 14. PMID: 32292128; PMCID: PMC7583324.
- Soares L. Psychology: The science of human behavior – a historical perspective. Diversitas Journal ISSN 2525-5215 Volume 8, Number 3 (Jul./Sept. 2023). 2023; 2526 – 2537·
- Camacho E, Soares L, Faria AL, Fernandes MC. Healthy Lifestyles in the Elderly: State-of-the-Art. Biomed J Sci Tech Res. 51(1)-2023. BJSTR.
- Soares L, Leal T, Faria AL, Aguiar A, Carvalho C. Social Determinants of Cardiovascular, Novel Practices in Med Study. 2023; 1(2). NPMS.000508.2023.
- Soares L, Cabral S, Faria AL. Mental Health and Obesity in Childhood and Adolescence. Novel Practices in Med Study. 2023; 1(2). NPMS.000509.2023.