More Information
Submitted: November 15, 2023 | Approved: November 24, 2023 | Published: November 27, 2023
How to cite this article: Elzein AM, Ahmed HSI, Suliman AA, Handay SOM, Omer GB, et al. Women's Perceptions of Medical Treatment Versus Surgical Management of First-trimester Miscarriage. Clin J Obstet Gynecol. 2023; 6: 193-200.
DOI: 10.29328/journal.cjog.1001150
Copyright License: © 2023 Eltigani AM, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Perception; Medical; Surgical; Treatment; First-trimester miscarriage
Abbreviations: D&C: Dilation and Curettage; HB: Haemoglobin; WHO: World Health Organization
Women's Perceptions of Medical Treatment Versus Surgical Management of First-trimester Miscarriage
Azza Mustafa Elzein1, Hajar Suliman Ibrahim Ahmed2, Awadalla Abdelwahid Suliman2* , Siddig Omer M Handay3, Gamar Bushra Omer4 and Sahar Ali Musa5
, Siddig Omer M Handay3, Gamar Bushra Omer4 and Sahar Ali Musa5
1Obstetrics and Gynecology Consultant, Sudan Medical Specialization Board, Sudan
2Obstetrics and Gynecology Consultant, Faculty of Medicine, Al Neelain University, Sudan
3Obstetrics and Gynecology Consultant, Faculty of Medicine, Garden City University, Sudan
4Obstetrics and Gynecology Consultant, Faculty of Medicine, Gezira University, Sudan
5Obstetrics and Gynecology Specialist, Gezira College of Medicine and Sciences, Sudan
*Address for Correspondence: Awadalla Abdelwahid Suliman, Obstetrician & Gynaecologist Consultant, Head of Department of Obstetrics and Gynecology, Faculty of Medicine, Al Neelain University, Khartoum, Sudan, Email: [email protected]
Background: Miscarriage is a common gynecological problem and early pregnancy loss occurs in the first trimester. Early pregnancy miscarriage is managed expectantly, surgically, and medically. Medical management is a new treatment option, also surgical evacuation is the standard treatment for some types and presentations of miscarriage. Medical management might be more suitable instead of surgical evacuation, it may be less costly than surgical treatment and consequently, due to its lower complications, most patients prefer it.
Purpose: This study aimed to determine women's perception of medical treatment versus surgical intervention, complications associated with surgical procedures, and medical treatment.
Methodology: It was a comparative, hospital-based study conducted in Bashair Teaching Hospital, on 336 patients diagnosed with miscarriage in the first trimester, 168(group A) were treated medically while 168(group B) were treated surgically. All participating patients in the study fulfilled the selection criteria, that is, the provision of an informed consent and agreement to participate in the study.
Results: The total number of women during the period of study was 336. The study found that 239(71%) of women prefer medical management compared to 97 (29%) preferring surgery. The complications associated with the medical treatment were (4.2%) infection, (0.6%) bleeding, and (95.2%) without obvious complications. The complications associated with surgical procedures were (7.7%) developmental infection, (16.1%) bleeding, (10.7%) incomplete evacuation, (1.8%) uterine perforation, and (63.7%) without obvious complications.
Conclusion: The study found that over two-thirds of patients Favor medical treatment over surgical procedures. It has also revealed that medical treatment is very effective in terminating pregnancies within the first trimester.
First-trimester miscarriage is a common gynecological problem, women presented with vaginal bleeding and abdominal pain, they treated by either surgical or medical treatment by Misoprostol, but women's satisfaction with each method will help other women to take their best option of treatment and reduce morbidity.
In our study most women favored medical over surgical management of first-trimester miscarriage, they wish for less hospital stay, less cost, and less need for pain relief and anesthesia complications, the success rate of medical treatment of first-trimester miscarriage was (80.7%), and complications among women who used medical treatment is less than surgical treatment. Which indicates that medical treatment is better than surgical treatment in selected cases.
The women's satisfaction with medical treatment will influence other women to choose this method of treatment as an alternative to a surgical option, protocols of use of Misoprostol its dose and the route of admiration is a challenge for gynecologists also auditing of medical treatment about gestational age.
Miscarriage, defined as the spontaneous loss of a pregnancy before 24 weeks gestation, is common with approximately 25% of women experiencing a miscarriage in their lifetime. An estimated 15% of pregnancies end in miscarriage. Miscarriage can lead to serious morbidity, including hemorrhage, infection, and even death, particularly in settings without adequate healthcare provision. Early miscarriages occur during the first 14 weeks of pregnancy and can be managed expectantly, medically, or surgically [1].
The overall early pregnancy loss rate is thought to be nearly 50%. At least 15% of fertilized ova are lost before implantation and 20% - 25% of pregnancies end before they can be clinically detected leading to an incidence of spontaneous abortion of some 12% - 19% among clinically recognized pregnancies [2-4].
Miscarriage can be managed expectantly (waiting for the pregnancy tissue to pass naturally), medically (tablets given to make the womb expel the pregnancy tissue), or surgically (removal of the pregnancy tissue during surgery). However, there is uncertainty about the effectiveness, safety, and side effects of the available methods for managing a miscarriage. First-trimester miscarriage is terminated by surgical evacuation of the uterus [5,6]. Currently, the methods recommended by the (World Health Organization) WHO for first-trimester abortion are vacuum aspiration, as the surgical method of choice; and medical abortion, either with Misoprostol only or in combination with mifepristone [7].
Medical abortion comprises the use of mifepristone in combination with Misoprostol or Misoprostol alone. These drugs stimulate uterine contractions and cause the uterine contents to be expelled [8]. The drug, Misoprostol, has been used to reduce the risk of stomach ulcers and is now more commonly used to stimulate contractions of the uterus. In recent years, physicians have begun prescribing Misoprostol in place of surgery to women who have experienced miscarriage [9].
In recent years, the medical management of miscarriage, which can achieve complete uterine evacuation in 95% of early first-trimester miscarriages, has been developed as a realistic alternative to surgical evacuation [10].
Currently, both surgical and medical options are acceptable in practice but differ in clinical efficacy, costs and patient experiences, and deciding what the best method is not clear [11-13].
Medical treatment with Misoprostol is a cheaper alternative to surgery, it is five times more inexpensive than curettage. Given its success rates higher than 80%, mild side effects, controllable with additional medication and a high degree of overall satisfaction, it should be prioritized over the evacuation curettage in patients who meet the treatment criteria [14]. Although medical treatment was associated with a higher failure rate, there was no statistically significant difference in the effectiveness of both treatment methods. However, medical treatment was associated with higher client acceptance and satisfaction and was more cost‑effective than surgical treatment [15].
Surgical or medical management of early pregnancy failure can be cost-effective, depending on the circumstances. Surgery is cost-effective and more productive when performed in an outpatient setting. For incomplete or inevitable abortion, medical management is cost-effective and more efficacious [16].
The risks of using medication to expedite a miscarriage (rather than having a Dilatation and Curettage (D & C)) are about the same as the risks of miscarrying naturally. There's a small chance of hemorrhage, infection, and needing a D&C later on if tissue remains in the uterus. A D & C carries some small risks also, so the choice is individual -- except in those cases where a medical emergency necessitates a D & C. Length of bleeding for a medically induced miscarriage is about the same as for a miscarriage that happens without intervention about two weeks [17].
This was a comparative study; it was conducted in Bashair Teaching Hospital in a period from May 2020 up to October 2020.
The Study population that was included all patients who came to the casualty with first-trimester miscarriages were included, about 168 (for each group).
Data was collected by direct interview by using a well-structured questionnaire. The participants were interviewed about age, education, occupation, gestational age (weeks), ultrasound finding, amount of vaginal bleeding (mild, moderate, severe, and shock), cervix close or open, the dose of misoprostol, route of misoprostol complications after management (bleeding Infection, incomplete evacuation, uterine perforation, blood transfusion, method of management, Haemoglobin level the result of the scan after primary management, complications management, and treatment preference.
Statistical analysis was performed via SPSS software (SPSS, Chicago, IL, USA). Continuous variables were compared using the student’s t-test (for paired data) or the Mann–Whitney U test for nonparametric data. For categorical data, a comparison was done using the Chi-square test (X2) or Fisher’s exact test when appropriate. A p - value of < 0.05 was considered statistically significant.
Ethical consideration was taken, and it was presented to the Sudan Medical Specialization Board (SMSB) and the Ethics Review Committee (EDC) and approved, permission to conduct the study was requested from authorities of health care in Bashair Teaching Hospital, data was handled with a high degree of confidentiality throughout the study, and written informed Consent was taken from all participants in the study. Throughout the study, written informed consent was obtained from all participants in the study.
During the study period, a total of 336 pregnant women presented with miscarriages in the first trimester, (group A) 168 patients were treated medically via Misoprostol and were followed up, while (group B) 168 were treated surgically in Bashair Teaching Hospital. The demographical parameters of women, their treatment outcomes and associated complications were analyzed.
The age group study population was more than 35 years old, 114 (34.0%) of the patients were in the age group over 35 years old, followed by the age group (31 - 35) years, 80 (23.8%) and the least group 32 (9.5%) were in the age group under 20 years old as most of the women had primary school level 177 (52.7%) while the university was lest group 36 (10.7%). In most of our studies, women were housewives 241 (71.7%) while employees were 22 (6.6%).
The women were presented with different gestational ages 140 (41.7%) were presented at GA (5 weeks - 7 weeks), 93 (27.7%) were presented at GA (7 - 9) weeks, and 103 (30.6%) were presented at GA (10 - 12) weeks (Table 1).
| Table 1: Sociodemographic characteristic of first-trimester miscarriage women (n = 336). | ||
| Sociodemographic | Frequency | Percent% |
| Age | ||
| < 20 years | 32 | 9.5% |
| 20 - 25 years | 66 | 19.6% |
| 26 - 30 year | 44 | 13.1% |
| 31 - 35 years | 80 | 23.8% |
| > 35 years | 114 | 34.0% |
| Total | 336 | 100.0 |
| Education level | Frequency | Percent |
| Illiterate | 38 | 11.3% |
| Primary school | 177 | 52.8% |
| Secondary school | 85 | 25.3% |
| University | 36 | 10.6% |
| Total | 336 | 100.0% |
| Occupation | Frequency | Percent |
| Housewives | 241 | 71.7% |
| Workers | 73 | 21.7% |
| Employees | 22 | 6.6% |
| Total | 336 | 100.0% |
| GA | Frequency | Percent |
| 5 - 7 weeks | 140 | 41.7% |
| 7 - 9 weeks | 93 | 27.7% |
| 10 - 12 weeks | 103 | 30.6% |
| Total | 336 | 100.0 |
Women presented according to the severity of bleeding. In group (A) 108 (64.3%) were mild, 64 (35.7%) were moderate and no severe cases, while in the group (B) 27 (16.1%) were mild, 46 (27.4%) were moderate, 62 (36.9%) were severe and 33 (19.6%) were shock cases p – value 0.01.
Women according to cervical status in group (A), 107 (63.7%) presented with a closed cervix 61 (36.3%) with an opened cervix, group (B) 55 (32.7%) with a closed cervix, and 113 (67.3%) presented with the opened cervix p - value 0.02 (Table 2).
| Table 2: The Severity of Bleeding and Cervical status of first-trimester miscarriage women (n = 336). | |||||
| Severity of bleeding | Case-Group- A | Control-Group- B | p - value | ||
| Frequency | Percent | Frequency | Percent | ||
| Mild | 108 | 64.3% | 27 | 16.1% | |
| Moderate | 60 | 35.7% | 46 | 27.4% | 0.01 |
| Severe | 0 | 0% | 62 | 36.9% | |
| Shock | 0 | 0% | 33 | 19.6% | |
| Cervical status | |||||
| Closed | 107 | 63.7% | 55 | 32.7% | 0.02 |
| Open | 61 | 36.3% | 113 | 67.3% | |
| Total | 168 | 100.0% | 168 | 100.0% | |
The complications associated with surgical procedure, 13 (7.7%) of the patients had an infection, 27 (16.1%) of the patients presented with bleeding, 18 (10.7%) of the patients presented with incomplete evacuation, 3 (1.8%) of the patients had uterine perforation and 107 (63.7%) were without obvious complications. complications associated with medical treatment, 7 (4.2%) of the patients had an infection, 1 (0.6%) of the patients presented with bleeding, and 160 (95.2%) were without obvious complications p – value 0.01 (Table 3).
| Table 3: Complications after the management of first-trimester miscarriage women (n = 69). | |||||
| Complication | Case Group A | Control-Group- B | p - value | ||
| Frequency | Percent | Frequency | Percent | ||
| Infection | 7 | 4.2% | 13 | 7.7% | |
| Bleeding | 1 | 0.6% | 27 | 16.1% | |
| Uterine perforation | 0 | 0.0% | 3 | 1.8% | 0.01 |
| Incomplete evacuation | 0 | 0.0% | 18 | 10.7% | |
| No complications | 160 | 95.2% | 107 | 63.7% | |
| Total | 168 | 100 | 168 | 100.0 | |
The complications in current miscarriage, in group (A), (12.5%) of the patients had bleeding, and (87.5%) of the patients had an infection, while in group (B), (44.3%) of the patients had bleeding, (21.3%) of the patients had infection, (29.5%) of the patients had incomplete evacuation and (4.9%) had uterine perforation p - value 0.01.
Women complications were managed, in group (A) all the patients received antibiotics, while in group (B) 18 (29.5%) of the patients had re-evacuation, 34 (55.7%) of the patients received antibiotics, 3 (4.9%) had laparotomy and 6 (9.9%) had observation. p - value 0.03 (Table 4).
| Table 4: Complications and management of first-trimester miscarriage (A) and surgical treatment(B) (n = 69). | |||||
| Complication and Management | Group- A | Group- B | p - value | ||
| Frequency | Percent | Frequency | Percent | ||
| Bleeding | 1 | 12.5% | 27 | 44.3% | |
| Infection | 7 | 87.5% | 13 | 21.3% | |
| Incomplete evacuation | 0 | 0% | 18 | 29.5% | 0.01 |
| Uterine perforation | 0 | 0% | 3 | 4.9% | |
| Management | |||||
| Re evacuation | 0 | 0% | 18 | 29.5% | |
| Antibiotics | 8 | 100.0% | 34 | 55.7% | 0.03 |
| Laparotomy | 0 | 0% | 3 | 4.9% | |
| No treatment | 0 | 0% | 6 | 9.9% | |
| Total | 8 | 100.0% | 61 | 100.0% | |
After primary management women's ultrasound was done, in the group(A) all 168 (100.0%) of the patients had complete evacuation, while in group (B) 153 (91.1%) of the patients had complete evacuation, while 15 (8.9%) were not (Table 5).
| Table 5: Result of the scan after primary management of first-trimester miscarriage women (n = 336). | |||||
| Result scan | Group- A | Group- B | p - value | ||
| Frequency | Percent | Frequency | Percent | ||
| Complete evacuation | 168 | 100% | 153 | 91.1% | 0.02 |
| Incomplete evacuation | 0 | 0% | 15 | 8.9% | |
| Total | 168 | 100% | 168 | 100% | |
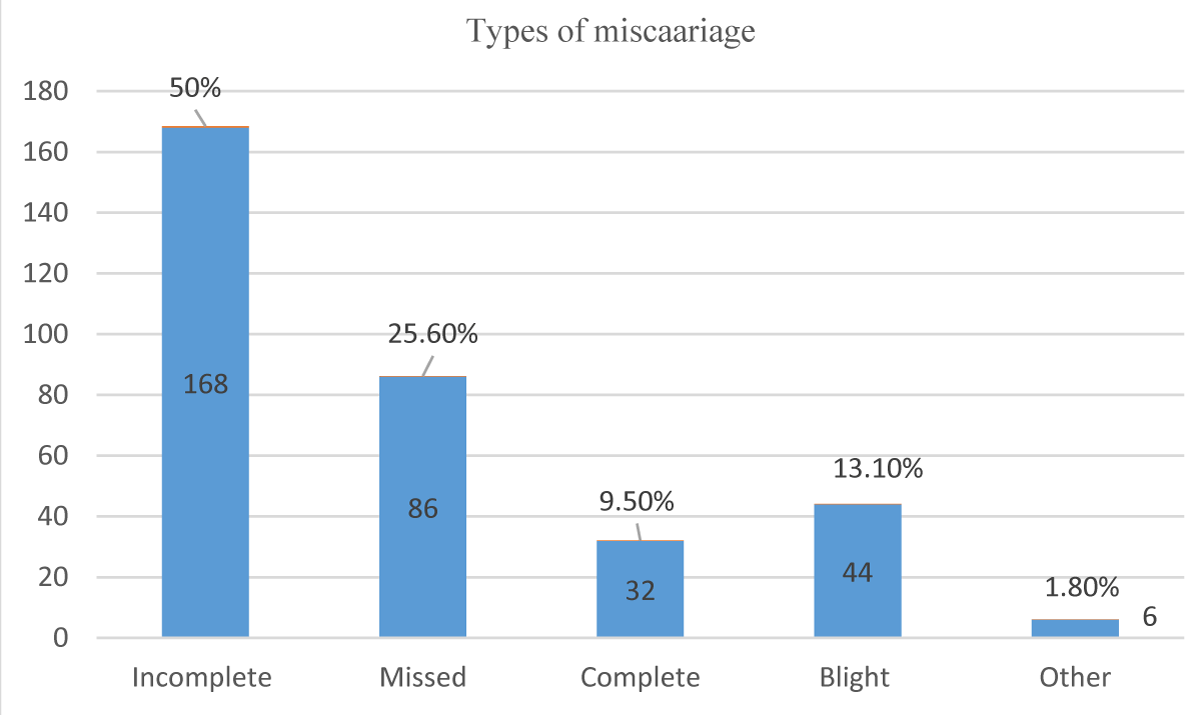
Women were diagnosed by ultrasound, to the type of miscarriages, missed were 86 (25.6%), 168 (50.0%) were incomplete, 44 (13.1%) were blighted and 6 (1.8%) were other (Figure 1).
Figure 1: Type of Miscarriage (n = 336).
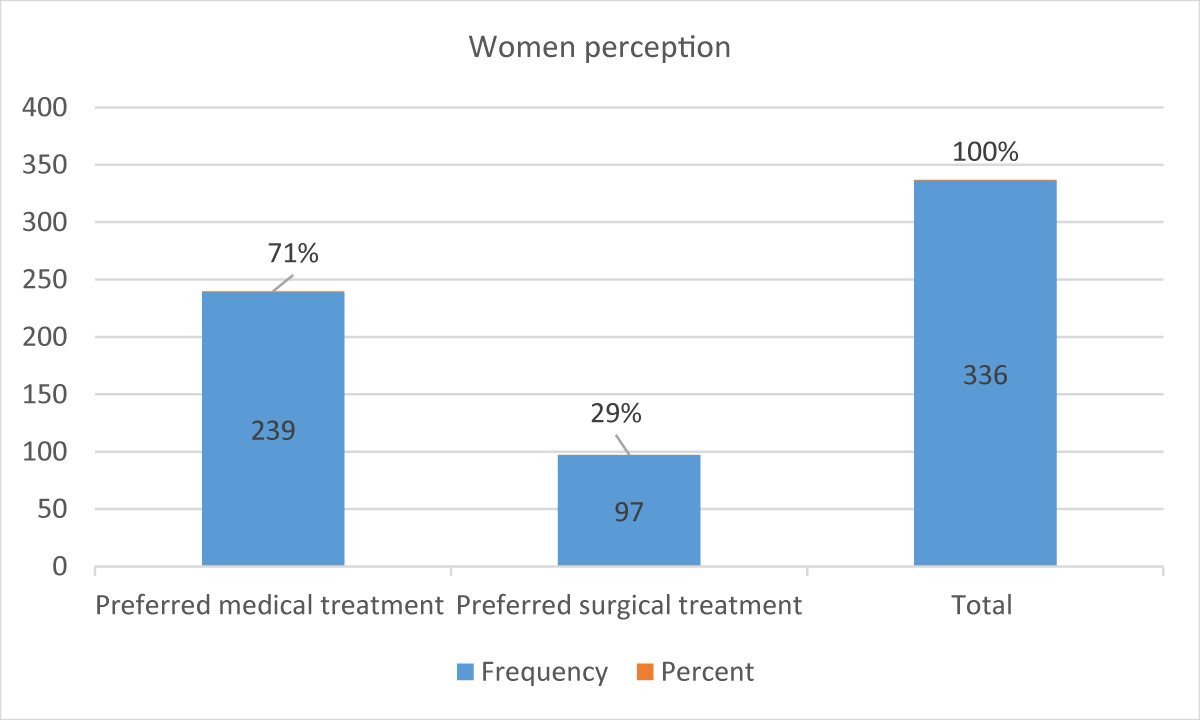
Perception of medical versus surgical management 119 (71%) preferred medical while 49 (29.0%) preferred surgical treatment (Figure 2).
Figure 2: Women's Perception of Treatment (n = 336).
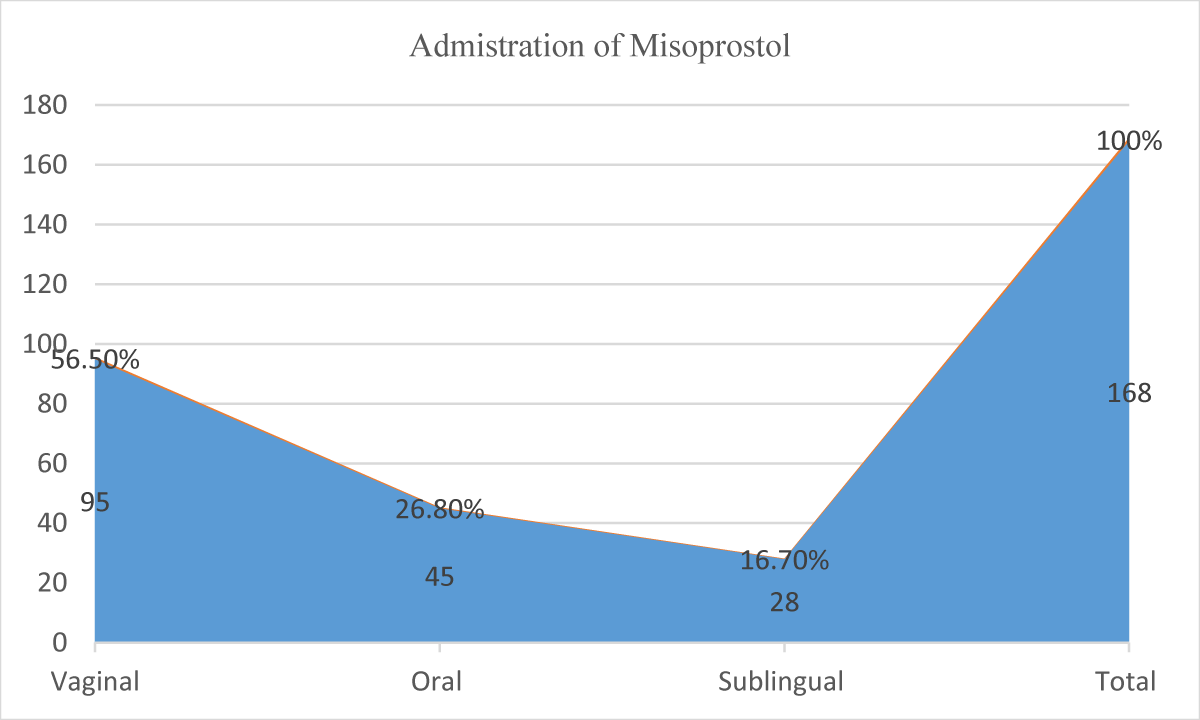
Administration of medical management vaginal were 95 (56.5%), 45 (26.8%) were oral and 28 (16.7%) were used sublingual (Figure 3).
Figure 3: Administration of Misoprostol (n = 168).
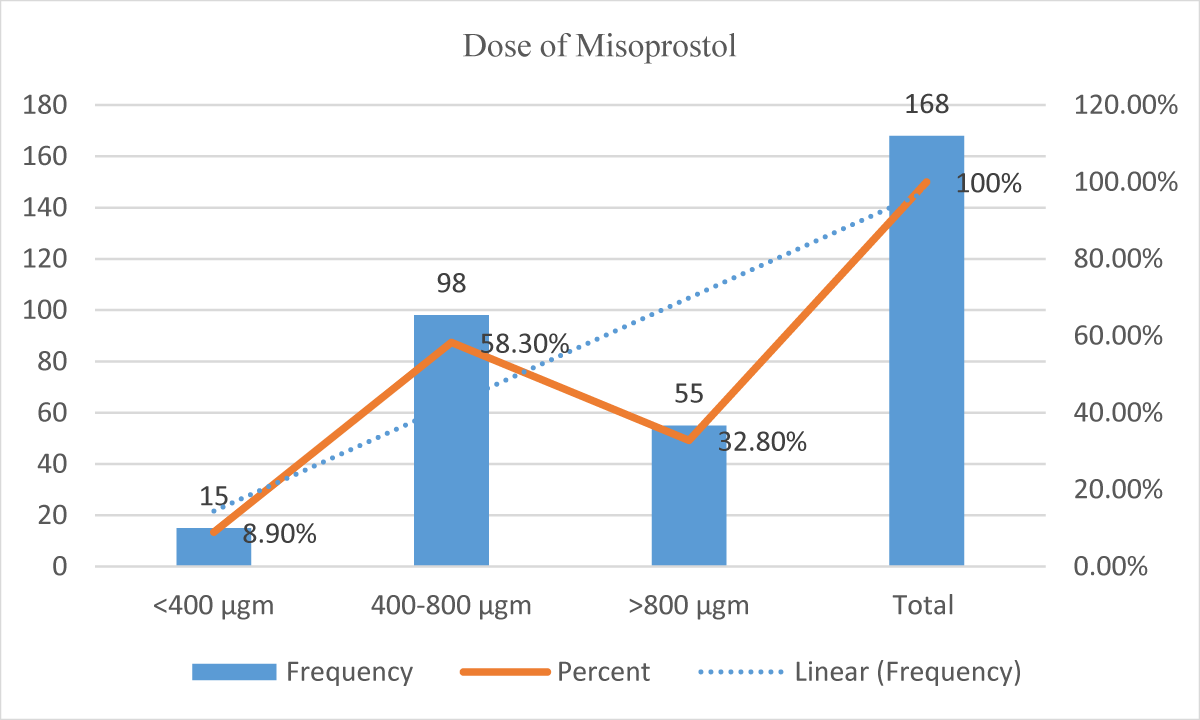
Misoprostol administrated doses of < 400 mcg were 15 (8.9%), 90 (58.3%) were between 400 – 800 mcg and 55 (32.8%) used more than 800mcg (Figure 4).
Figure 4: Dose of Misoprostol in medical treatment (n = 168).
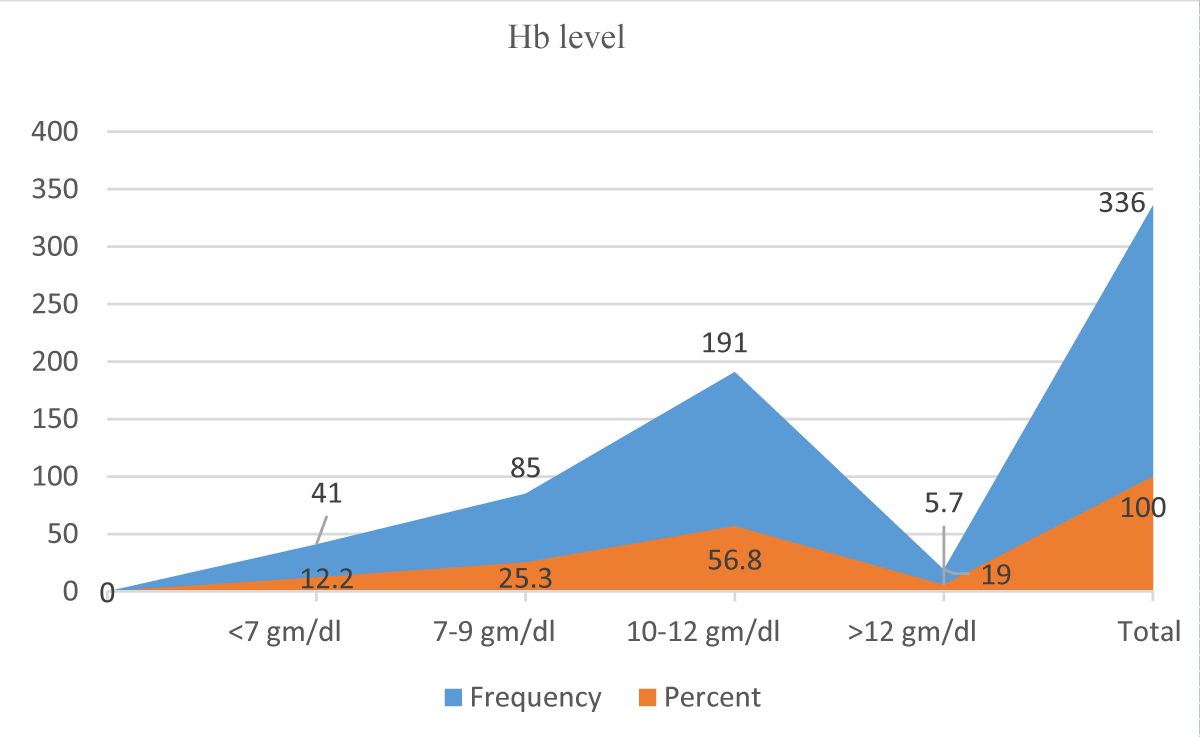
Women Hb level HB/gm, < 7 gm were 41 (12.2%), 85 (25.3%) were between 7 - 9 gm/d, 191 (56.8%) were between 10 - 12 gm/d and 19 (5.7%) were > 12 gm/dl (Figure 5).
Figure 5: Distribution of the patients according to their Hemoglobin level (n = 336).
This comparative study included 336 patients and had been split into two groups, A and B, each comprising 168 patients. Group A underwent medical treatment for first-trimester miscarriage, while group B underwent surgical procedure for first-trimester miscarriage.
The study aimed to reveal patients’ perceptions of medical versus surgical treatments and the complications associated with each regarding first-trimester miscarriage treatment. Women with early pregnancy miscarriage were counseled about medical and surgical treatment also the advantages and disadvantages of each method should be explained in a sympathetic approach, and her preference should be respected. Also, their satisfaction with the methods they choose is determined after treatment. Women's education positively affects their counseling and options for medical treatment.
This study initially showed that (71%) of patients favored medical over surgical management of first-trimester miscarriage and (29%) favored surgical management, which agreed with a previous study [18,19], which found the women who underwent medical miscarriage treatment reported greater satisfaction than surgical treatment.
On the other point of view, this was not similar to other rates of satisfaction found in other studies [20] that have reported no difference in satisfaction with surgical medical or conservative management of miscarriage.
Our study shows that the medical management of the first-trimester miscarriage has a (100%) success rate using intravaginally Misoprostol was a highly effective modality. The success rate of (80.7%) reported in our study is in line with the previous study [21].
The success rates of medical evacuation vary from (25%) up to (97%) for oral, sublingual, or vaginal Misoprostol in different studies [22]. These variations between studies probably reflect the different Misoprostol regimens used, routes of administration, and the route of administration. Also, a study [23] found that medical methods are effective, safe, and acceptable whether used Misoprostol alone or combined with Mifepristone.
Women who underwent surgical evacuation developed complications, (7.7%) of the patients had an infection, (16.1%) of the patients presented with bleeding, (10.7%) of the patients presented with incomplete evacuation, (1.8%) of the patients had uterine perforation and (63.7%) were without obvious complications. The complications associated with medical treatment were that (4.2%) of the patients had an infection, (0.6%) of the patients presented with bleeding, and (95.2%) were without obvious complications. The high success rate observed in the Misoprostol group is similar to that reported by [24] and Chigbu, et al. in Abia [25]. Similarly, the result of this study is consistent with studies done in Uganda [26], Tanzania [27], Egypt [28], and Burkina Faso [29] and also a recent Cochrane review [30] which indicates that surgical management is more likely to induce complete evacuation of the uterus than medical management, although it did not reach statistically significant difference in these studies. in contrast study [31] revealed that in the surgical evacuation group, only one woman (1.8%) had a post-abortion infection, and no cases had a cervical laceration, perforation, or required blood transfusion. According to one study [32], the mean duration of bleeding in women undergoing medical termination of pregnancy ranges from 8 to 17 days [33] but may be more prolonged. In this study [32], as an example, 9 percent of women reported mild bleeding after 30 days and 1 percent after 60 days [33]. The perception among women is that the bleeding is more pronounced after medical than surgical procedures because of the duration, rather than the volume of blood loss. The prolonged bleeding is annoying to many women; attempts to reduce this by administration of oral contraception or methotrexate were ineffective [34,35].
However, this study showed a relatively small percentage of patients (0.6%) reported bleeding compared to (16.1%) of patients who reported bleeding after surgical treatment. Additionally, (4.2%) of the medical group had an infection and (7.7%) of the patients who underwent surgical evacuation had an infection p - value .02, so our finding regarding infection agrees with other studies [20] which state that the incidence of infection following a medical miscarriage is lower than after a surgical miscarriage [33].
In the US, infection with Clostridium is responsible for a small number of deaths following medical abortion. The initial report was four septic deaths that occurred in California within one week after medical abortion. The most appropriate explanation for these differences may be due to those other studies that included high-risk pregnant women, while our study included women without consideration for risk factors. Also, other studies were population-based studies while our current study was hospital-based. We found a substantially lower risk of complications among women who underwent medical treatment (bleeding and infection, additionally, Ultrasound findings revealed post evacuation that almost (99.3%) of patients had empty uteruses while (0.7%) were with retained products p - value .01.
Most of the women in this study (68.5%) were between 5 weeks - 9 weeks, the study found that medical miscarriage is very effective in ending pregnancies in the first trimester. A study of 128 women in their second week's follow-up [36-39] found five to 9 weeks was the most appropriate effective period for the efficacy of the medical treatment.
This study showed good follow-up for the patients who underwent medical and surgical treatment and that was in a referring clinic 2 weeks after the procedure [40-42].
A limitation was that the study used a small sample size. Patient selection, sampling, intervention, and data collection were all done by the same observer. Furthermore, the severity of vaginal bleeding and its grade (mild, moderate, severe) is subjective rather than objective.
The study found that medical management of miscarriage is very effective in ending pregnancies in the first trimester also it disclosed that more than two-thirds of patients favored medical miscarriage over surgical miscarriage.
This study found that bleeding, infection, and uterine perforation were the most common complications associated with surgical miscarriage, while infection was the most common complication associated with medical miscarriage.
The study disclosed that successful completion of medical miscarriage in pregnancies up to 12 weeks of gestation was (98.1%).
Recommendations
Medical treatment is recommended for patients with first-trimester miscarriage due to the associated high success rate and lesser complications, using a population health approach to determine the types of miscarriages and to identify the root of administration, dose, and frequency of medical miscarriage can help to identify the determinants of miscarriage complications that put patients at further risk. We need to teach and counsel women about the benefits of medical miscarriage but meticulous follow-up is necessary and is required to manage complications for excellent outcomes. Oral administration of Misoprostol is less effective and results in more side effects than vaginal. It is not recommended with amenorrhea of beyond 49 days. Vaginal dosing appears to be associated with an increased risk of serious post-miscarriage infection. The study quantified the problems of medical miscarriage versus surgical and further studies on a large scale are needed to measure the magnitude of the problem.
The authors would like to express their sincere thanks and gratitude to Yousif Suliman Ibrahim who provided technical help, writing assistance, and material support.
Approval
Ethical clearance and supportive letters were obtained from the Sudan Medical Specialization Board (SMSB) and the Educational Development Centre (EDC) and approved. Written permission was obtained from Bashir Teaching Hospital. All participants were consented.
Author contribution: All authors contributed to the manuscript writing of the manuscript.
Data sharing: The authors agreed on the date-sharing policy of this journal.
Data are ethically correct to do so, where this does not violate the protection of human subjects, or other valid ethical, privacy, or security concerns.
Data availability (where applicable)
All data supporting the results reported in the manuscript can be found and data sharing includes, where applicable, from Scientific Data Bank and additional unpublished data from the study, if any, are available, to whom and how these can be obtained. The authors agreed on the date-sharing policy of this journal. The authors agree to make the data and materials supporting the results or analyses presented in their paper available upon reasonable request. The authors agree to cite any data sets referenced in the article and provide a Data Availability Statement. Data are ethically correct to do so, where this does not violate the protection of human subjects or other valid ethical, privacy, or security concerns.
- Ghosh J, Papadopoulou A, Devall AJ, Jeffery HC, Beeson LE, Do V, Price MJ, Tobias A, Tunçalp Ö, Lavelanet A, Gülmezoglu AM, Coomarasamy A, Gallos ID. Methods for managing miscarriage: a network meta-analysis. Cochrane Database Syst Rev. 2021 Jun 1;6(6):CD012602. doi: 10.1002/14651858.CD012602.pub2. PMID: 34061352; PMCID: PMC8168449.
- Henderson JT, Hwang AC, Harper CC, Stewart FH. Safety of mifepristone abortions in clinical use. Contraception. 2005 Sep;72(3):175-8. doi: 10.1016/j.contraception.2005.03.011. PMID: 16102550.
- Hasan R, Baird DD, Herring AH, Olshan AF, Jonsson Funk ML, Hartmann KE. Patterns and predictors of vaginal bleeding in the first trimester of pregnancy. Ann Epidemiol. 2010 Jul;20(7):524-31. doi: 10.1016/j.annepidem.2010.02.006. PMID: 20538195; PMCID: PMC2884141.
- Turesheva A, Aimagambetova G, Ukybassova T, Marat A, Kanabekova P, Kaldygulova L, Amanzholkyzy A, Ryzhkova S, Nogay A, Khamidullina Z, Ilmaliyeva A, Almawi WY, Atageldiyeva K. Recurrent Pregnancy Loss Etiology, Risk Factors, Diagnosis, and Management. Fresh Look into a Full Box. J Clin Med. 2023 Jun 15;12(12):4074. doi: 10.3390/jcm12124074. PMID: 37373766; PMCID: PMC10298962.
- Sanchez-Morales JE, Rodriguez-Contreras JL, Ruiz-Lara L, Ochoa-Torres B, Zaragoza M, Padilla-Zuniga K. Cost Analysis of Surgical and Medical Uterine Evacuation Methods for First-Trimester Abortion Used in Public Hospitals in Mexico. Health Serv Insights. 2022 Sep 23; 15:11786329221126347. doi: 10.1177/11786329221126347. PMID: 36171763; PMCID: PMC9511298.
- Nweke NA, Anikwe CC, Ewah RL, Umeononihu OS, Eze JN. Analgesic efficacy and safety of paracervical block versus conscious sedation in the surgical evacuation of the uterus following first-trimester incomplete miscarriages: A randomised controlled trial. SAGE Open Med. 2022 Jul 24; 10:20503121221113227. doi: 10.1177/20503121221113227. PMID: 35910816; PMCID: PMC9326839.
- Safe Abortion: Technical and Policy Guidance for Health Systems. 2nd ed. Geneva: World Health Organization; 2012. PMID: 23700650.
- McEvoy A, Sabir S. Physiology, Pregnancy Contractions. 2022 Sep 19. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan–. PMID: 30422522.
- Zhang J, Gilles JM, Barnhart K, Creinin MD, Westhoff C, Frederick MM; National Institute of Child Health Human Development (NICHD) Management of Early Pregnancy Failure Trial. A comparison of medical management with misoprostol and surgical management for early pregnancy failure. N Engl J Med. 2005 Aug 25;353(8):761-9. doi: 10.1056/NEJMoa044064. PMID: 16120856.
- Neilson JP, Gyte GM, Hickey M, Vazquez JC, Dou L. Medical treatments for incomplete miscarriage. Cochrane Database Syst Rev. 2013 Mar 28;(3):CD007223. doi: 10.1002/14651858.CD007223.pub3. Update in: Cochrane Database Syst Rev. 2017 Jan 31;1:CD007223. PMID: 23543549.
- Rausch M, Lorch S, Chung K, Frederick M, Zhang J, Barnhart K. A cost-effectiveness analysis of surgical versus medical management of early pregnancy loss. Fertil Steril. 2012 Feb;97(2):355-60. doi: 10.1016/j.fertnstert.2011.11.044. Epub 2011 Dec 21. PMID: 22192348; PMCID: PMC3269545.
- Barghazan SH, Hadian M, Rezapour A, Nassiri S. Economic evaluation of medical versus surgical strategies for first trimester therapeutic abortion: A systematic review. J Educ Health Promot. 2022 Jun 30;11:184. doi: 10.4103/jehp.jehp_1274_21. PMID: 36003248; PMCID: PMC9393924.
- Whitehouse KC, Kim CR, Ganatra B, Duffy JMN, Blum J, Brahmi D, Creinin MD, DePiñeres T, Gemzell-Danielsson K, Grossman D, Winikoff B, Gülmezoglu AM. Standardizing abortion research outcomes (STAR): a protocol for developing, disseminating and implementing a core outcome set for medical and surgical abortion. Contraception. 2017 May;95(5):437-441. doi: 10.1016/j.contraception.2016.12.009. Epub 2017 Jan 5. PMID: 28065833; PMCID: PMC5473939.
- Cubo AM, Soto ZM, Haro-Pérez A, Hernández Hernández ME, Doyague MJ, Sayagués JM. Medical versus surgical treatment of first trimester spontaneous abortion: A cost-minimization analysis. PLoS One. 2019 Jan 10;14(1):e0210449. doi: 10.1371/journal.pone.0210449. Erratum in: PLoS One. 2019 Mar 29;14(3):e0214707. PMID: 30629715; PMCID: PMC6328124.
- Roy TS, Saha PK, Roy S. Efficacy of Vaginal Misoprostol Administered for Rapid Management of First Trimester Spontaneous Onset Incomplete Abortion in Comparison to Manual Vacuum Aspiration: A Randomised Clinical Trial. Journal of Clinical & Diagnostic Research. 2023; 17(6).
- Neill S. Management of Early Pregnancy Loss. JAMA. 2023 Apr 25;329(16):1399-1400. doi: 10.1001/jama.2023.0933. PMID: 37027174.
- Schaff EA, Fielding SL, Eisinger SH, Stadalius LS, Fuller L. Low-dose mifepristone followed by vaginal misoprostol at 48 hours for abortion up to 63 days. Contraception. 2000 Jan;61(1):41-6. doi: 10.1016/s0010-7824(99)00119-5. PMID: 10745068.
- Wedisinghe L, Elsandabesee D. Flexible mifepristone and misoprostol administration interval for first-trimester medical termination. Contraception. 2010 Apr;81(4):269-74. doi: 10.1016/j.contraception.2009.09.007. Epub 2009 Oct 29. PMID: 20227541.
- Berkley HH, Greene HL, Wittenberger MD. Mifepristone Combination Therapy Compared With Misoprostol Monotherapy for the Management of Miscarriage: A Cost-Effectiveness Analysis. Obstet Gynecol. 2020 Oct;136(4):774-781. doi: 10.1097/AOG.0000000000004063. PMID: 32925621.
- Borchert K, Adam P. Which management option for first-trimester miscarriage has the highest patient satisfaction: expectant, medical, or surgical? Evidence-Based Practice. 2018; 21(7):14.
- Shankar M, Economides DL, Sabin CA, Tan B, Kadir RA. Outpatient medical management of missed miscarriage using misoprostol. J Obstet Gynaecol. 2007 Apr;27(3):283-6. doi: 10.1080/01443610701213927. PMID: 17464813.
- Chen BA, Creinin MD. Medical management of early pregnancy failure: efficacy. Semin Reprod Med. 2008 Sep;26(5):411-22. doi: 10.1055/s-0028-1087107. Epub 2008 Sep 29. PMID: 18825609.
- Abubeker FA, Lavelanet A, Rodriguez MI, Kim C. Medical termination for pregnancy in early first trimester (≤ 63 days) using combination of mifepristone and misoprostol or misoprostol alone: a systematic review. BMC Womens Health. 2020 Jul 7;20(1):142. doi: 10.1186/s12905-020-01003-8. PMID: 32635921; PMCID: PMC7339463.
- Ani VC, Enebe JT, Dim CC, Dim NR, Ozumba BC. Sublingual misoprostol versus manual vacuum aspiration for treatment of incomplete abortion in Nigeria: a randomized control study. Pan Afr Med J. 2022 Feb 1;41:90. doi: 10.11604/pamj.2022.41.90.29364. PMID: 35432695; PMCID: PMC8977358.
- Chigbu B, Onwere S, Aluka C, Kamanu C, Ezenobi O. IS MISOPROSTOL A SUITABLE ALTERNATIVE TO THE SURGICAL EVACUATION OF INCOMPLETE ABORTION IN RURAL SOUTH-EASTERN NIGERIA? East Afr Med J. 2012 May;89(5):172-7. PMID: 26875224.
- Weeks A, Alia G, Blum J, Winikoff B, Ekwaru P, Durocher J, Mirembe F. A randomized trial of misoprostol compared with manual vacuum aspiration for incomplete abortion. Obstet Gynecol. 2005 Sep;106(3):540-7. doi: 10.1097/01.AOG.0000173799.82687.dc. PMID: 16135584.
- Jin H, Zhang M, Yang X, Liu J, Muhetaer M, Chen Y, Liu X. Comparison of misoprostol and manual vacuum aspiration in treating first-trimester incomplete miscarriage: a systematic review and meta-analysis of randomized controlled trials. 2023.
- Dabash R, Ramadan MC, Darwish E, Hassanein N, Blum J, Winikoff B. A randomized controlled trial of 400-μg sublingual misoprostol versus manual vacuum aspiration for the treatment of incomplete abortion in two Egyptian hospitals. Int J Gynaecol Obstet. 2010 Nov;111(2):131-5. doi: 10.1016/j.ijgo.2010.06.021. PMID: 20801444.
- Dao B, Blum J, Thieba B, Raghavan S, Ouedraego M, Lankoande J, Winikoff B. Is misoprostol a safe, effective and acceptable alternative to manual vacuum aspiration for postabortion care? Results from a randomised trial in Burkina Faso, West Africa. BJOG. 2007 Nov;114(11):1368-75. doi: 10.1111/j.1471-0528.2007.01468.x. Epub 2007 Sep 5. PMID: 17803715.
- Kim C, Barnard S, Neilson JP, Hickey M, Vazquez JC, Dou L. Medical treatments for incomplete miscarriage. Cochrane Database Syst Rev. 2017 Jan 31;1(1):CD007223. doi: 10.1002/14651858.CD007223.pub4. PMID: 28138973; PMCID: PMC6464743.
- Shuaib AA, Alharazi AH. Medical versus surgical termination of the first trimester missed miscarriage. Alexandria Journal of Medicine. 2013; 49(1):13-16.
- Spitz IM, Bardin CW, Benton L, Robbins A. Early pregnancy termination with mifepristone and misoprostol in the United States. N Engl J Med. 1998 Apr 30;338(18):1241-7. doi: 10.1056/NEJM199804303381801. PMID: 9562577.
- Christin-Maitre S, Bouchard P, Spitz IM. Medical termination of pregnancy. N Engl J Med. 2000 Mar 30;342(13):946-56. doi: 10.1056/NEJM200003303421307. PMID: 10738054.
- Aubeny E, Chatellier G. A randomized comparison of mifepristone and self-administered oral or vaginal misoprostol for early abortion. Eur J Contracept Reprod Health Care. 2000 Sep;5(3):171-6. doi: 10.1080/13625180008500394. PMID: 11131781.
- Schaff EA, Fielding SL, Westhoff C. Randomized trial of oral versus vaginal misoprostol at one day after mifepristone for early medical abortion. Contraception. 2001 Aug;64(2):81-5. doi: 10.1016/s0010-7824(01)00229-3. PMID: 11704083.
- Chu JJ, Devall AJ, Beeson LE, Hardy P, Cheed V, Sun Y, Roberts TE, Ogwulu CO, Williams E, Jones LL, La Fontaine Papadopoulos JH, Bender-Atik R, Brewin J, Hinshaw K, Choudhary M, Ahmed A, Naftalin J, Nunes N, Oliver A, Izzat F, Bhatia K, Hassan I, Jeve Y, Hamilton J, Deb S, Bottomley C, Ross J, Watkins L, Underwood M, Cheong Y, Kumar CS, Gupta P, Small R, Pringle S, Hodge F, Shahid A, Gallos ID, Horne AW, Quenby S, Coomarasamy A. Mifepristone and misoprostol versus misoprostol alone for the management of missed miscarriage (MifeMiso): a randomised, double-blind, placebo-controlled trial. Lancet. 2020 Sep 12;396(10253):770-778. doi: 10.1016/S0140-6736(20)31788-8. Epub 2020 Aug 24. PMID: 32853559; PMCID: PMC7493715.
- Musik T, Grimm J, Juhasz-Böss I, Bäz E. Treatment Options After a Diagnosis of Early Miscarriage: Expectant, Medical, and Surgical. Dtsch Arztebl Int. 2021 Nov 19;118(46):789-794. doi: 10.3238/arztebl.m2021.0346. PMID: 34696822; PMCID: PMC8864670.
- Aiken A, Lohr PA, Lord J, Ghosh N, Starling J. Effectiveness, safety and acceptability of no-test medical abortion (termination of pregnancy) provided via telemedicine: a national cohort study. BJOG. 2021 Aug;128(9):1464-1474. doi: 10.1111/1471-0528.16668. Epub 2021 Mar 24. PMID: 33605016; PMCID: PMC8360126.
- Nwafor JI, Agwu UM, Egbuji CC, Ekwedigwe KC. Misoprostol versus manual vacuum aspiration for treatment of first-trimester incomplete miscarriage in a low-resource setting: A randomized controlled trial. Niger J Clin Pract. 2020 May;23(5):638-646. doi: 10.4103/njcp.njcp_379_19. PMID: 32367870.
- Spechler SJ, Hunter JG, Jones KM, Lee R, Smith BR, Mashimo H, Sanchez VM, Dunbar KB, Pham TH, Murthy UK, Kim T, Jackson CS, Wallen JM, von Rosenvinge EC, Pearl JP, Laine L, Kim AW, Kaz AM, Tatum RP, Gellad ZF, Lagoo-Deenadayalan S, Rubenstein JH, Ghaferi AA, Lo WK, Fernando RS, Chan BS, Paski SC, Provenzale D, Castell DO, Lieberman D, Souza RF, Chey WD, Warren SR, Davis-Karim A, Melton SD, Genta RM, Serpi T, Biswas K, Huang GD. Randomized Trial of Medical versus Surgical Treatment for Refractory Heartburn. N Engl J Med. 2019 Oct 17;381(16):1513-1523. doi: 10.1056/NEJMoa1811424. PMID: 31618539.
- Borstlap WAA, Musters GD, Stassen LPS, van Westreenen HL, Hess D, van Dieren S, Festen S, van der Zaag EJ, Tanis PJ, Bemelman WA. Vacuum-assisted early transanal closure of leaking low colorectal anastomoses: the CLEAN study. Surg Endosc. 2018 Jan;32(1):315-327. doi: 10.1007/s00464-017-5679-6. Epub 2017 Jun 29. PMID: 28664443; PMCID: PMC5770507.
- Borregaard B, Dahl JS, Riber LPS, Ekholm O, Sibilitz KL, Weiss M, Sørensen J, Berg SK, Møller JE. Effect of early, individualised and intensified follow-up after open heart valve surgery on unplanned cardiac hospital readmissions and all-cause mortality. Int J Cardiol. 2019 Aug 15; 289:30-36. doi: 10.1016/j.ijcard.2019.02.056. Epub 2019 Apr 11. PMID: 31006596.