More Information
Submitted: November 07, 2023 | Approved: November 11, 2023 | Published: November 13, 2023
How to cite this article: Eltigani A, Ahmed TU, Suliman AA, SalahEldin A, Siralkatim I, et al. Near-miss Women Causes and Prevalence in Alobied Maternity Hospital. Clin J Obstet Gynecol. 2023; 6: 185-192.
DOI: 10.29328/journal.cjog.1001149
Copyright License: © 2023 Eltigani A, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Maternal; Morbidity; Organ; Damage; Hemorrhage; Infection
Abbreviations: ANC: Antenatal care; ICU: Intensive Care Unit; MNM: Maternal Near-Miss; MNMR: Maternal Near-Miss Rate; WHO: World Health Organization
Near-miss Women Causes and Prevalence in Alobied Maternity Hospital
Ayat Eltigani1, Taha Umbeli Ahmed2, Awadalla Abdelwahid Suliman3* , Abdelsalam SalahEldin1, Isra Siralkatim1 and Hajar Suliman3
, Abdelsalam SalahEldin1, Isra Siralkatim1 and Hajar Suliman3
1Department of Obstetrics & Gynecology, Sudan Medical Specialization Board, Khartoum, Sudan
2Department of Obstetrics & Gynecology, Omdurman Islamic University, Khartoum, Sudan
3Department of Obstetrics & Gynecology, Alneelain University, Khartoum, Sudan
*Address for Correspondence: Awadalla Abdelwahid Suliman, Obstetrician & Gynaecologist Consultant, Head of Department of Obstetrics and Gynecology, Faculty of Medicine, Al Neelain University, Khartoum, Sudan, Email: [email protected]
Background: Maternal near-miss (MNM) events occur more frequently than maternal deaths; therefore, more detailed and comprehensive studies on maternal morbidity have been conducted and are of value to clinical audits and practices.
Purpose: This study aimed to determine the frequency of maternal near misses and the nature of near-missevents.
Methodology: This descriptive, retrospective, cross-sectional study over 12 months duration was conducted at the Alobied Teaching Hospital in 2018.
Data were collected from patient notes, partographs, and other relevant documents.
Demographic and clinical data concerning personal history, obstetric history, and near-miss events.
Results: A total of 15202 women were admitted, 339 cases of maternal near misses, maternal near-missrate (MNMR) of 22.3|1000 live births, 200(59%) had an infection, 80(23.6%) hemorrhage, 20(5.9%) severe pre-eclampsia, 12(3.5%) eclampsia, 20(5.9%) anemia, convulsions 5(1.5%) 17(5%) of the cases were admitted to intensive care unit (ICU), 9(2.7%) had liver dysfunction, 9(2.7%) coagulation dysfunction, 8(2.4%) renal dysfunction, 5(1.5%) cerebral problems, 4(1.2%) cardiac dysfunction, and 2(0.6%) had developed respiratory dysfunction.
Conclusion: The maternal near-miss rate was 22.3|1000 live births. Most near-miss cases occurred before the women arrived at the hospital. The major causes of maternal near misses were infection, hemorrhage anemia, pre-eclampsia, and eclampsia.
A maternal near-missis defined as acute obstetric complications that immediately threaten a woman's survival but does not result in her death either by chance or because of hospital care she received during pregnancy labor or within 6 weeks after termination of pregnancy [1,2] also, defined by WHO as women who nearly died but survived a complication that occurred during pregnancy, childbirth, or within 6 weeks from termination of pregnancy [3], it occurs more frequently and has similar causes as with maternal deaths [4], MNM is useful to examine the quality of obstetric care since pregnancy complications occur in women worldwide [5].
The prevalence of MNM ranges between (0.80% and 8.23%) among studies that used clinical criteria and (0.01% – 2.99%) among studies that use management criteria. A recent study found in sub-Saharan African countries, the median MNM ratio was (24.2 per 1000 live births) [6] the rate ranged between (0.14% and 0.75%) in some of the high-income countries, it ranged between (1.5% and 7.7%) in some of middle- income countries, and, in sub-Saharan African countries, it ranged between (2.21% and 12%) [7] Exploring the similarities, the differences and the relationship between women who died and those who survived life-threatening conditions provide a more complete assessment of quality in maternal health care [8].
The WHO evaluates the quality of care using the maternal near-miss concept and criterion-based clinical audit, and developing the near-miss concept in neonatal health [1]. Criteria to identify potentially life-threatening conditions and maternal near misses include severe postpartum hemorrhage, severe pre-eclampsia, eclampsia, sepsis, or severe systemic infection ruptured uterus, critical interventions which include the use of blood products, laparotomy (including hysterectomy, excluding cesarean delivery) and admission to an intensive care unit or recovery room for 6 hours or clinical organ dysfunction and management-based proxies like hysterectomy after infection or hemorrhage [9,10].
A local study in Sudan found Maternal Near-missIncidence Ratio (MNMIR) was 7.2/1000 live births, the MNM to MD ratio was 5.8:1.Hemorrhage was the most common cause of MNM, followed by eclampsia, sepsis, hepatitis, cardiac disease, and other indirect events: 48.5%, 28.8%, 15.7%, 3.1%, 2.7%, and 1.2%, respectively [11], a study of MNM incidences and causes [6] was conducted done in Addis Ababa, Ethiopia, which provides a maternal near-missincidence ratio of 8.01 per 1000 live births, underlying causes of the were hypertensive disorders and obstetric hemorrhage. Anemia is the major contributing cause [6]. The MNM incidence ratio was 23.6 per 1,000 live births, with an overall case fatality rate of 12.9%, and concluded that maternal morbidity and mortality remain challenging problems in a rural referral hospital in Tanzania [12]. Ethiopia [13] discovered that there was still a significant national prevalence of maternal near misses. It has been discovered that prenatal care protects against maternal near misses. It is advised to modify other chronic medical conditions and prioritize prenatal care to prevent anemia as preventative measures. It is advised to avoid primary cesarean sections unless absolutely necessary [14]. Reported that the incidence of near misses in Kenya was 7.2 per 1000 live births; [15] found that the prevalence of near misses in Uganda was 287.7 per 1000 pregnancies; the MNM rate was also found to be [16] and [17] to be between 4 and 29 percent in Ethiopia; [18] reported a ratio of 50.4 per 1000 live births. Given that MNM cases at the facility level occur more frequently than maternal deaths on average [19], noted that a sufficient number of cases can produce reliable and useful data to raise the standard of care. MNM permits facilities to work on cases as well. According to [20], the use of the WHO MNM tool in low-resource settings has led to an underreporting of life-threatening incidents, which is thought to be caused by a shortage of laboratory and diagnostic resources as well as blood for transfusion.
By implementing evidence-based obstetric interventions and providing ongoing in-service training for healthcare professionals, the quality of maternal health services must be improved [21].
This was a descriptive, retrospective, cross-sectional hospital-based study conducted at the Alobied Maternity Hospital between January 2018 and December 2018. All women diagnosed with near misses were included and agreed to participate. The principal investigators identified the cases daily with the assistance of trained resident registrars for data collection. It was done through daily participation in morning meetings, meeting reports, and daily rounds of labor wards, intensive care units, operating rooms, and postnatal words.
The participants were interviewed about age, residence, education, parity, gestational age at the time of near miss, nature of obstetric complications, mood of delivery, admission to the ICU, presence of organ and/or system dysfunction, and duration of hospital stay. The patient was classified by the final diagnosis concerning hemorrhage sepsis, hypertension, dystocia, anemia, and other medical disorders. The inclusion criteria were that all women diagnosed with near misses were included, and women with maternal mortality were excluded.
Statistical analysis was performed using SPSS software (SPSS, Chicago, IL, USA), and variables were compared using Student's t - test (for paired data) or post hoc test, Mann–Whitney U test for non-parametric data. For categorical data, comparisons were performed using the chi-square test (X2) or Fisher's exact test, as appropriate. Statistical significance was set at p < 0.05.
Ethical clearance was obtained from the ethical committee of the Sudan Medical Specialization Board, Council of Obstetrics and Gynecology. An official agreement from the general managers of the Alobied Teaching Hospital preceded the study. Ethical considerations were taken, presented to the ethics review committee, and approved, data was handled with a high degree of confidentiality throughout the study, and written informed consent was obtained from all participants in the study.
During the study period, a total of 15202 women were admitted to the Alobied Teaching Hospital, and 339 were diagnosed with maternal near misses. Maternal near-missrate (MNMR) was 22.3/1000 live births, of which 155(45.7%) women were from rural areas and 184(54.3%) from urban areas.
Most women 305(90%) were admitted from home and 34(10%) were referred to emergency. Most women 204(60.2%) aged between 20-30 years and the least aged below 20 years, 5(1.5%), 309(91.2%) of women were married,18(5.2%) were single, divorced 7(2.1%) and 5(1.5%) were widowed. Primary school 111(32.7%), illiterate 96(28.3%), secondary school 71(20.9%), university 37(10.9%), and the post graduated were 24(7.2%) (Table 1).
| Table 1: Sociodemographic distribution of near-misswomen (n = 339). | |||
| Sociodemographic | Frequency | Percent | |
| Age | < 20 | 204 | 60.2 |
| 20 - 30 | 95 | 28 | |
| 31 - 40 | 35 | 10.3 | |
| > 40 | 5 | 1.5 | |
| Marital status | Married | 309 | 91.2 |
| Single | 18 | 5.2 | |
| Divorced | 7 | 2.1 | |
| Wido | 5 | 1.5 | |
| Education | Primary | 111 | 32.7 |
| Illiterate | 96 | 28.3 | |
| Secondary | 71 | 20.9 | |
| University | 37 | 10.9 | |
| Postgraduate | 24 | 7.2 | |
| Total | 339 | 100 | |
Near miss, women presented at less than 28 weeks gestation 130(38.4%), between 28-36 weeks, 97(28.6%), at 37 weeks or more 75(22.1%) and presented in the puerperium period 37(10.9%).
Women without antenatal care were 122(36%), consultant antenatal care for 104(30.6%), midwifery care for 44(13%), registers care for 27( 8%), medical officers care for 27( 8%), and health visitors for 15(4.4%).
Delivery status outcomes, 214(63.1%) not delivered, 57(16.8%) delivered vaginally at the hospital, 38(11.2%) of the cases delivered at home, 27(8%) by emergency cesarean section, 2(0.6%) delivered by using instruments, and 1(0.3%) by elective cesarean section (Table 2).
| Table 2: Obstetric characteristic distribution of near-miss women (n = 339). | |||
| Obstetric characteristic | Frequency | Percent | |
| Gestational Age | < 28weeks | 130 | 38.4 |
| 28 - 36 weeks | 97 | 28.6 | |
| 37 - 42weeks | 75 | 22.1 | |
| Puerperium | 37 | 10.9 | |
| Antenatal care provider | No ANC | 122 | 36 |
| Consultant | 104 | 30.6 | |
| Midwife | 44 | 13 | |
| Medical officer | 27 | 8 | |
| Registrar | 27 | 8 | |
| Health visitor | 15 | 4.4 | |
| Delivery status | Not Delivered | 214 | 63.1 |
| Vaginal delivery | 57 | 16.8 | |
| Home delivery | 38 | 11.2 | |
| Emergency CS | 27 | 8 | |
| Instrumental | 2 | 0.6 | |
| Elective CS | 1 | 0.3 | |
| Total | 339 | 100 | |
Pregnancy outcomes of near-misswomen live births 106(31.3%), fresh still births 10(2.9%), macerated still birth delivery, 4(1.2%), 3(0.9%) were early pregnancy, neonatal death, 2(0.6%) and 214(63.1%) no complications (Table 3).
| Table 3: Pregnancy outcomes distribution of near-miss women (n = 339). | ||
| Pregnancy outcomes | Frequency | Percent |
| Before delivery | 214 | 63.1 |
| Live birth | 106 | 31.3 |
| Fresh stillbirth | 10 | 2.9 |
| Macerated stillbirth | 4 | 1.2 |
| Early pregnancy | 3 | 0.9 |
| Neonatal death | 2 | 0.6 |
| Total | 339 | 100 |
Previous medical history of near near-miss, 309(91.2%) had no medical disorders, 10(2.9%) had hypertension,7(2.1%) Diabetes Mellitus, 5(1.5%) Bronchial Asthma, 4(1.1%) epilepsy, 3(0.9%) had Sickle cell anemia and 1(0.3%) had heart disease (Table 4).
| Table 4: Past medical history distribution of near-miss women (n = 339). | ||
| Past medical history | Frequency | Percent |
| No past medical history | 309 | 91.2 |
| Hypertension | 10 | 2.9 |
| Diabetes Mellitus | 7 | 2.1 |
| Asthma | 5 | 1.5 |
| Epilepsy | 4 | 1.1 |
| Sickle cell anemia | 3 | 0.9 |
| Heart disease | 1 | 0.3 |
| Total | 339 | 100 |
Complications of hemorrhage distribution of near-missshowed that 33(9.7%) of the cases presented with hemorrhage had tachycardia (> 100 b/min), 21(6.2%) had a blood transfusion (with loss of more than 2 litters), 15(4.4%) had systolic blood pressure (< 90 mmhg), 1.5% presented shock, 5(1.5%) from the cases emergency hysterectomy and 1(0.3%) had coagulation defects (Table 5).
| Table 5: Complications of hemorrhage distribution of near-miss women (n = 339). | ||||
| Complication of hemorrhage | Frequency | Percent | Mean | St. Deviation |
| Tachycardia pulse > 100 Beats/min | 33 | 9.7 | 1.9027 | .29687 |
| Systolic < 90 | 15 | 4.4 | 1.9558 | .20595 |
| Blood transfusion > 2 liter | 21 | 6.2 | 1.9381 | .24142 |
| Patient shock | 5 | 1.5 | 1.9853 | .12073 |
| Emergency hysterectomy | 5 | 1.5 | 1.9853 | .12073 |
| Coagulation defect | 1 | 0.3 | 1.9971 | .05431 |
End organ involvement in this study, 247(72.9%) had no evidence of end-organ damage, 9(2.7%) of the cases had liver dysfunction (abnormal liver function test, jaundice in patients with pre-eclampsia), 9(2.7%) had coagulation dysfunction (acute thrombocytopenia, prolonged bleeding time, abnormal (APTT or PT), coagulopathy), 8(2.4%) had renal dysfunction(oliguria, high urea, and creatinine, electrolyte disturbance), 5(1.5%) had cerebral dysfunction (coma, cerebral edema, seizures other than eclampsia, intracerebral hemorrhage ), 4(1.2%) had cardiac dysfunction (pulmonary edema, cardiac arrest, cardiac failure, pulmonary embolism), 2(0.6%) had respiratory dysfunction (O2 saturation < 90% intubation or ventilation for reasons other than general anesthesia) (Table 6).
| Table 6: End organ damage distribution of near-miss women (n = 339). | ||||
| End organ damage | Frequency | Percent | Mean | St. Deviation |
| Liver dysfunction | 9 | 2.7 | 1.9735 | .16100 |
| Coagulation dysfunction | 9 | 2.7 | 1.9735 | .16100 |
| Renal dysfunction | 8 | 2.4 | 1.9764 | .15202 |
| Cerebral dysfunction | 5 | 1.5 | 1.9853 | .12073 |
| Cardiac dysfunction | 4 | 1.2 | 1.9882 | .10814 |
| Respiratory dysfunction | 2 | 0.6 | 1.9941 | .07670 |
| No end-organ damage | 247 | 72.9 | 1.2714 | .44533 |
Regression analysis of complications of haemorrhage complications, tachycardia had 107.98 likelihood ratio, 95% CI 6.511(5.005-8.469), systolic < 90 had hemorrhage were 15, likelihood ratio 45.652and 95% CI 4.985 (4.011-6.195), Blood transfusion > 2 lite had hemorrhage 21, likelihood ratio 65.389 and 95% CI 5.390(4.281-6.786), near-misswomen had shock were 5 with haemorrhage , likelihood ratio 14.685 and 95% CI 4.453 (3.649-5.435), emergency hysterectomy was undertaken among 5 women with haemorrhage likelihood ratio 14.685 and only one woman with haemorrhage developed coagulation defect likelihood ratio 2.898, p - value. 02 (Table 7).
| Table 7: Regression of hemorrhage complications among near-miss women (n = 339). | |||||
| Complications of hemorrhage | Hemorrhage | Likelihood Ratio | 95% CI | ||
| Yes | No | ||||
| Tachycardia | Yes No |
33 47 |
0 259 |
107.984 | 6.511(5.005 - 8.469) |
| Systolic < 90 |
Yes No |
15 65 |
0 259 |
45.652 | 4.985 (4.011 - 6.195) |
| Blood transfusion > 2 liter |
Yes No |
21 59 |
0 259 |
65.389 | 5.390(4.281 - 6.786) |
| Patient shock | Yes No |
5 75 |
0 259 |
14.685 |
4.453 (3.649 - 5.435) |
| Emergency hysterectomy | Yes No |
5 75 |
0 259 |
14.685 | 4.453 (3.649 - 5.435) |
| Coagulation defect | Yes No |
1 79 |
0 259 |
2.898 | 4.278(3.527 - 5.189) |
| p - value. 02. | |||||
Regression analysis of end-organ damage of liver dysfunction was 9 near-misswomen had end-organ damage, likelihood ratio 24.145,95% CI 3.976(3.301-4.789), all women with coagulation dysfunction 9 had end organ damage likelihood ratio 24.145,95% CI 3.976(3.301-4.789), renal dysfunction were 8 had end-organ damage likelihood ratio 21.394 and 95% C I 3.940 (3.276-4.740), cerebral dysfunction were5likelihood ratio 13.245 and 95% CI3.839 (3.204-4.599), cardiac dysfunction were4, likelihood ratio 10.563and 95% CI 3.807(3.182-4.555) and respiratory dysfunction were two with least likelihood ratio 5.249 and 95% CI 3.744(3.137-4.469), p - value .01 (Table 8).
| Table 8: Regression of end-organ damage among near-miss women (n = 339). | |||||
| End organ damage | Organ damage | Likelihood Ratio | 95% CI | ||
| Yes | No | ||||
| Liver dysfunction | Yes No |
9 83 |
0 247 |
24.145 | 3.976(3.301 - 4.789) |
| Coagulation dysfunction |
Yes No |
9 83 |
0 247 |
24.145 | 3.976(3.301 - 4.789) |
| Renal dysfunction | Yes No |
8 84 |
0 247 |
21.394 | 3.940 (3.276 - 4.740) |
| Cerebral dysfunction | Yes No |
5 87 |
0 247 |
13.245 | 3.839 (3.204 - 4.599 |
| Cardiac dysfunction |
Yes No |
4 88 |
0 247 |
10.563 | 3.807(3.182 - 4.555) |
| Respiratory dysfunction | Yes No |
2 90 |
0 247 |
5.249 | 3.744(3.137 - 4.469) |
| No end organ damage |
Yes No |
92 0 |
155 92 |
70.214 | .628(.570 - .691) |
| p - value. 01. | |||||
Causes of near-miss infection 200(59%), hemorrhage 80(23.6%), anemia hemorrhage evidence 20 (5.9%), convulsions 5(1.5%), uterine ruptured two (.6%), severe pre-eclampsia 20(5.9%), and eclampsia 12(3.5%), p - value. 01 (Table 9).
| Table 9: Obstetrics event of near-miss women (n = 339). | ||
| Obstetric event | Frequency | Percent |
| Eclampsia | 12 | 3.5 |
| Severe pre-eclampsia | 20 | 5.9 |
| Uterine ruptured | 2 | 0.6 |
| Clinical anemia no hemorrhage | 20 | 5.9 |
| Infection | 200 | 59 |
| Hemorrhage | 80 | 23.6 |
| Convulsions | 5 | 1.5 |
| Total | 339 | 100 |
| p - value. 01. | ||
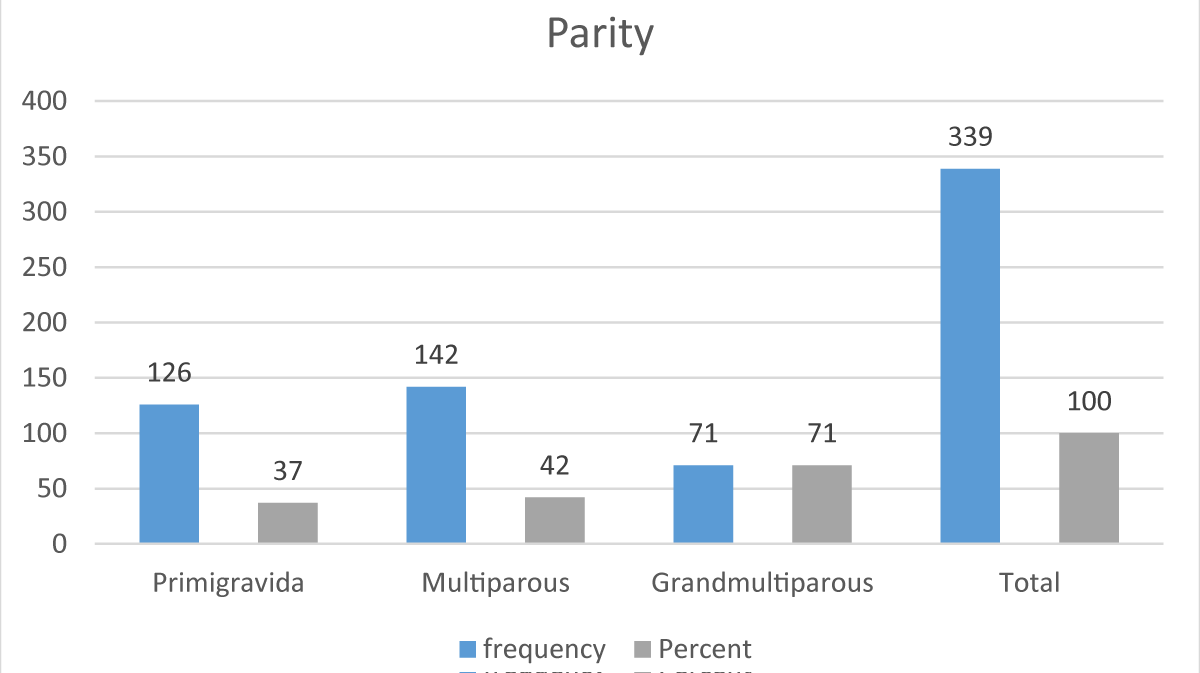
Most women were multigravida (had between 2 to4 past deliveries) 142(42%), 127(37%) were primigravida and the Gan multiparous women were 70(21%) (Figure 1).
Figure 1: Distribution of maternal near miss cases according to parity (n = 339).
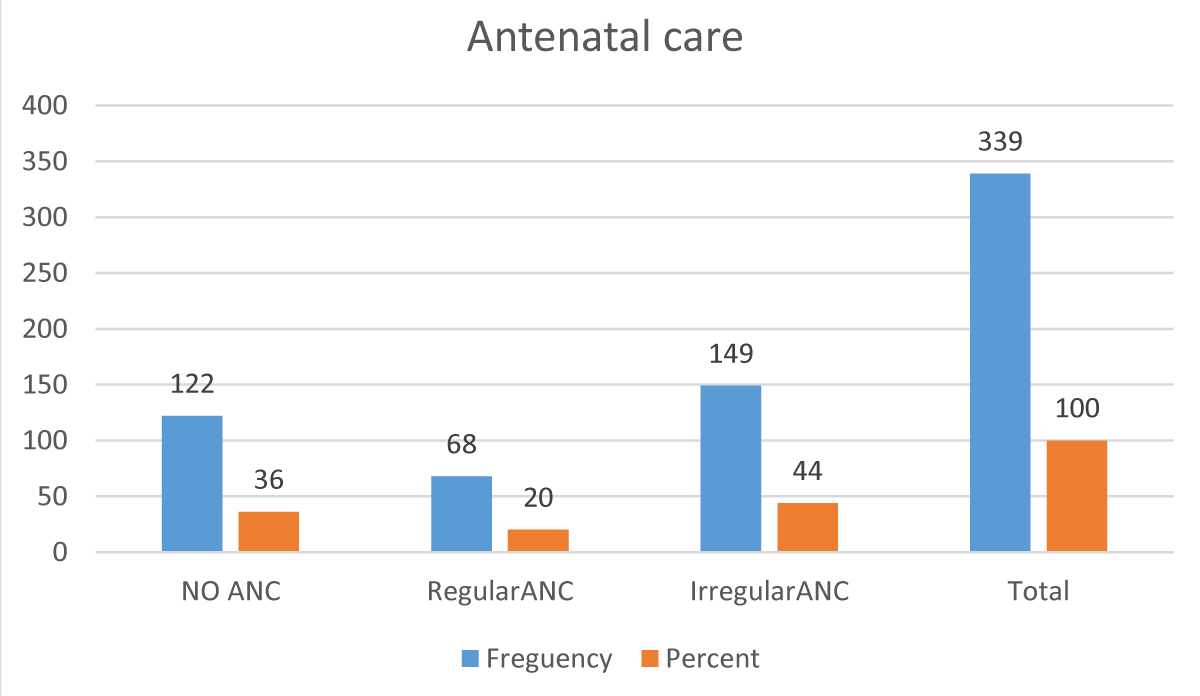
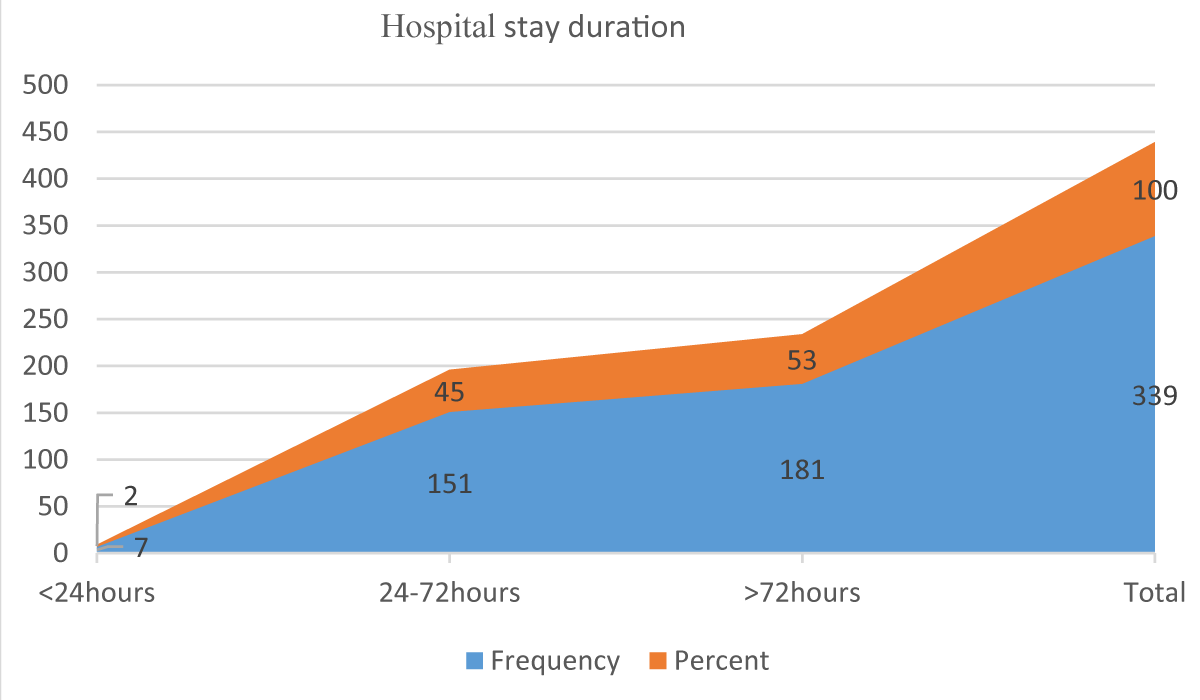
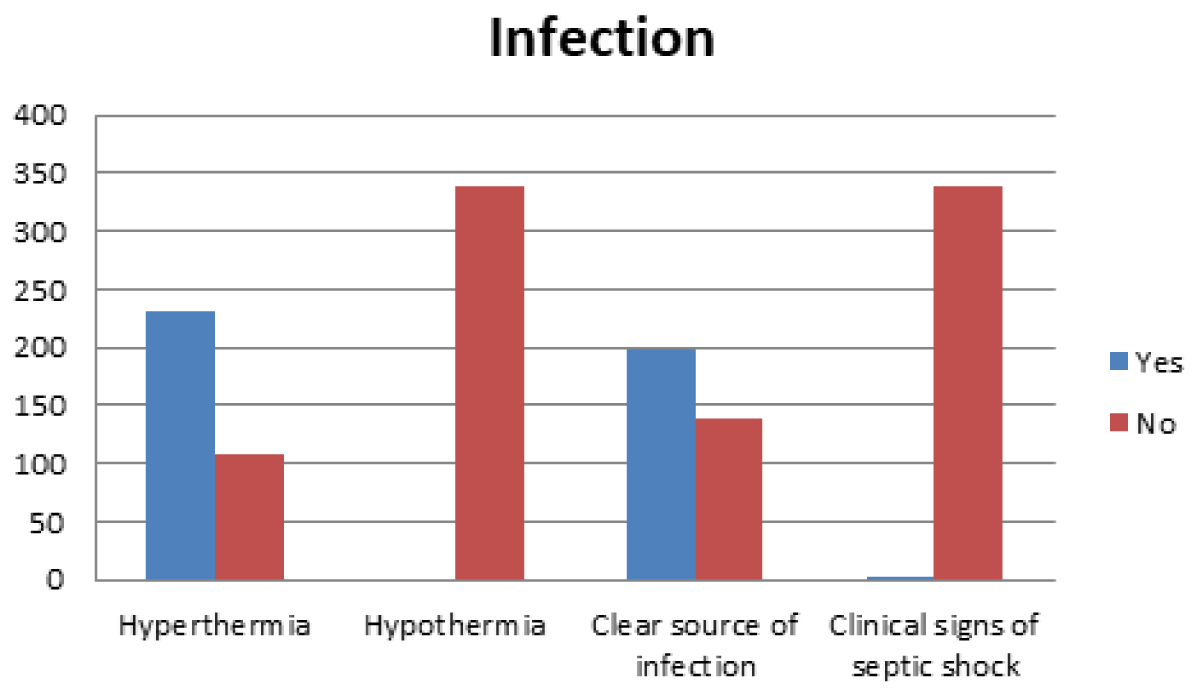
Antenatal care was irregular (less than 4 visits) in 148(44%), while 122(36%) from the cases without antenatal care and 69 (20%) from the cases had regular antenatal care (Figure 2). Duration of admission to the hospital stays found that 181(53%) were admitted more than 72 hours, 151(45%) between 24 hours up to 72 hours, and 7(2%) were admitted at intervals less than 24 hours. (Figure 3) women with infections, 231(68.1%) of the cases presented with hyperthermia, 199(58.7%) had no source of infection, and 1(0.3%) had clinical signs of septic shock (Figure 4).
Figure 2: Distribution of maternal near miss cases according to their antenatal care during current pregnancy (n = 339).
Figure 3: Distribution of maternal near miss cases according to the duration of hospital admission (n = 339).
Figure 4: Histogram of the distribution of maternal near miss cases according to the event of Infection.
This study showed a maternal near-miss rate (MNMR) of 22.3/1000 live births. Our MNMR was higher than that reported in a study conducted at the Omdurman Maternity Hospital in Sudan [11] which found that MNMR was 7.2/ 1000 live births, and another study [9], in the same line MNMR was 22.1/1000 live births. The higher rate of MNM in our study may be because our hospital is a secondary hospital in the state and all the cases were admitted after complications occurred, in comparison with Omdurman maternity hospital, which is a tertiary hospital in Khartoum state received referred cases from all states and hospitals, which lead to an increase in the total population, might also be partially due to differences in the definition and identification of cases, which are major limitations in comparison of near-miss data across hospitals and institutions. Ethiopian study reported MNMR 20.8% (Geleto 2019).
The mean age of the participants was 27(minimum14 years maximum 45 years), 37.5% were primigravida,20.6% grand multipara, 91.2% of the cases were married, 28.3% were illtreated, and the primary school level was 32.7%. Some studies reported that age, marital status, and parity, well-known predictors of maternal death, it comparable to those of a study [22] which found that being > 35 years of age, not having a partner, and being primipara or para > 3 were independently associated with the occurrence of a near miss, and also reported that low maternal education was found to be protective against the occurrence of a maternal near miss. A study of the profile of maternal near-missand determinant factors [23] showed that advancing maternal age was found to be a determinant of MNM, and in his study, where more than half of the maternal deaths occurred in the older age group also reported that the occurrence of MNM was commonly found among women with low education [23].
In contrast, the WHO global survey revealed that the near-miss ratio was significantly associated with higher educational levels [24] Our data did not investigate the total population of pregnant women to find the relationship between those factors and maternal near-miss; our study finding is comparable to study done in Ethiopia [6] found women who did not have formal education 47.5%), primary education 36.2%) had a higher incidence of near maternal miss, the most women age 20-34 years 65%, not married 10%, unbooked 58.8%, primigravida 33.8%), and grand multiparous 25.0%).
Also, in our study, we reported that 45.3% of the patient cases were from rural areas. 122(36%) without antenatal care. 34(10%) were referred to as emergencies from other hospitals, and the majority 305(90%) were emergencies from home [25], as reported in their studies that analyzed women who resided in rural, most near-miss women in Nigeria are from rural areas, according to [26].
The leading underlying cause of maternal near-miss infections, obstetrical hemorrhage, hypertensive disorders (Eclampsia and pre-eclampsia) and anemia, respectively, These results differed from the study [9] which found hemorrhage to be the major cause, followed by septicemia [9], and a study by [11] found that hemorrhage and hypertensive disorders the leading cause behind hemorrhage to be the second cause in this study was that all cases of maternal near-misscases have already occurred at home or at the hospital and areas that refereed the patients from it, the delay in seeking and reaching appropriate care because of lack of proper referral system, involvement of miscarriages that causes life-threatening bleeding in the criteria of MNM, all of which these contributed to an increase in the ratio of patients presented with hemorrhage and anemia. Hypertensive disorders of pregnancy accounted for 41% of the causes in an Egyptian study [27] (24%) pre-eclampsia, (15%) eclampsia, and (2%) chronic hypertension). The most common morbidities were bleeding (62%), hypertensive complications (24%), and abortion (6%) in Chad [28]. Pregnancy-related hypertension (29%) and obstetric hemorrhage/disseminated intravascular coagulation (40%) were the main causes in Italia according to [29].
Medical disorders associated with maternal near miss, 309(91.2%) were free from medical disorders, and the other chronic diseases that were confirmed from the history were, diabetes 7(2.1%); chronic hypertension, 10(2.9%);, 5(1.5%) known to be Asthmatic, 1(0.3%), heart disease; and 4(1.1%) had epilepsy, in the study [6] reported that pre-existing medical conditions such as previous chronic hypertension, previous anemia, and history of cardiac problems should be known, and women with maternal near- miss were more likely to report a previous history of chronic hypertension and cardiac problems [6]. We did not include the entire population of pregnant women in the Alobied hospital in our study to find a relationship between chronic disease and adverse effects in patients.
In our study status of delivery, 38(11.2%) of the patients were delivered at home, fifty-seven (16.8%) were delivered vaginally at the hospital, 2(0.6%) were delivered by using instruments, 27(8%) were by emergency cesarean section, and 1(0.3%) by elective cesarean section. In low-risk pregnancies, cesarean sections are known to pose potential risks to women’s health and a modifiable risk factor for maternal mortality when compared with vaginal delivery due to the increase in thromboembolism, puerperal infection, hemorrhage, and anesthetic complications [30] conversely, in the case of MNMs, the high rates of cesarean sections may be found because this is a population of high-risk pregnant women who urgently require pregnancy resolution and cesarean section may more frequent [25] in contrast to studying by [31] where 25.5% had a history of cesarean section deliveries in the previous pregnancies MNMR 28.74%, severe pre-eclampsia 35(24%).
Our incidence of cesarean section is less than that reported by [6] in their study of maternal near misses (80%) and 18 reported that the incidence of cesarean section in his study was 34.1%. However, it is similar to the [32] cesarean section rate, which is between (10% -15%). The difference in the ratio could be due to the small size of our study group and the involvement of all other gestational ages in our study, in addition to home deliveries.
The study found the number of major organ dysfunctions seen in the maternal near-miss cases of liver dysfunction; 9(2.7%) of those cases were mainly associated with eclampsia and pre-eclampsia, and 9(2.7%) of the cases also showed coagulation dysfunction followed by renal dysfunction 8(2.4%), 5(1.5%) cerebral dysfunctions (coma, cerebral edema, seizures other than eclampsia, intracerebral hemorrhage), Cardiac dysfunction 4(1.2%), and respiratory dysfunction 2(0.6%). Our data on organ failure is higher if compared to the study 13were no cases were reported of organ or system dysfunction and less than the study of 15 where organ dysfunction was reported in 73 cases [10], this is due to low admission to intensive care unit (ICU) in that were 17(5%), women with potential life-threatening conditions, and MNM might require levels of care that differ from one to another, ranging from basic obstetric care to comprehensive obstetric care, including surgery and intensive care, as the case may need [22]. This low percentage of admissions in our study due to the shortage of ICU beds and some of the cases referred to other private ICUs, also raised in the organ dysfunction rate, may be due to late referral to the hospital for appropriate management. It is comparable to a study in South Sudan [33-40] MNM prevalence of 9.41% on morbidity-based criteria and 3.1% on organ failure-based criteria.
Study strengths and limitations
This study is considered the first in the Al-Obeid region. One of the strengths of this study is that the samples and information were collected according to the WHO definition of maternal near misses and criteria for diagnosis and end-organ damage. The information was collected by registrars who administer the treatment, which had a positive impact on the inclusion of patients.
The study period of one year resulted in the involvement of adequate near-miss women which makes the study possible so the study population's characteristics can be generalized to Sudan and countermeasures can be developed in countries with similar characteristics.
One of the limitations of this study is that it was conducted in one hospital, so it cannot be compared.
The study demonstrates a higher prevalence of maternal near misses compared with a previous study in Sudan (22.3|1000 live births) the major causes are maternal infection, hemorrhage, hypertensive disorders (pre-eclampsia and eclampsia), and anemia. MNMR is more common among rural, low educational level, multiparous, and unbooked individuals. The patient's condition had a significantly prolonged hospital stay and intensive care unit admission.
Recommendations
Maternal advice of antenatal care, a good referral system potentially reduces severe maternal outcomes. Adequate provision of critical care, along with appropriate staffing, equipment, and management strategies. Staff training in emergency obstetric services. Access to ICU depends on facility protocols and availability, and the substantial proportion of study women who experienced severe maternal outcomes without access to ICU care indicates a shortage of ICU beds. Further studies on maternal near misses and death.
Summary
A maternal near-missis increasingly being recognized as a useful means to examine the quality of obstetric care. Hemorrhage, infection, eclampsia, pre-eclampsia, and medical disorders during pregnancy were common causes of maternal near misses.
The prevalence of maternal near misses was 22.3|1000 live births which is higher than previous studies in Sudan in different cities the causes of MNM included in this study were infections, obstetric hemorrhage, hypertensive disorder, anemia, and convulsions. End organ damage mostly involves the liver and coagulation system, and is less involved in the respiratory system.
The material near-miss plan of the referral system and management will improve, and end-organ damage and ICU admission with the World Health Organization (WHO) protocol should be applied to reduce maternal miss and maternal death. Auditing obstetrics practice of management of obstetrical hemorrhage, infection, anemia with pregnancy, and hypertensive disorders is a challenge.
The authors would like to express their sincere thanks and gratitude to Prof Taha Umbeli for his helpful supervision during this study.
Consent: All participants provided informed consent.
Approval: Ethical clearance and supportive letters were obtained from the Sudan Medical Specialization Board (SMSB) and& the Educational Development Centre (EDC). Written permission was obtained from Alobeid Hospital.
Author contribution
All authors contributed to the manuscript writing of the manuscript. Prof. Taha Umbeli and Ayat Eltigani were involved in the conception, and design of the study, writing the proposal, analysis, interpretation of data, and manuscript writing. Awadalla Abdelwahid, Abdelasam Salah Eldin, Isra Sir Alkhatim, and Hajar Suliman were involved in the analysis and, interpretation of data, methodology, and manuscript writing written.
Data sharing
The authors agreed on the date-sharing policy of this journal.
Data are ethically correct to do so, where this does not violate the protection of human subjects, or other valid ethical, privacy, or security concerns.
- Lozano R. Progress towards Millennium Development Goals 4 and 5 on Maternal and Child Mortality: An Updated Systematic Analysis. Lancet. 2011; 378: 1139-1165. Https://Doi.Org/10.1016/S0140-6736(11)61337-8.
- Bongaarts J. WHO, UNICEF, UNFPA, World Bank Group, and United Nations Population Division Trends in Maternal Mortality: 1990 to 2015 Geneva: World Health Organization, 2015. Population and Development Review. 42: 726-726. Https://Doi.Org/10.1111/Padr.12033.
- Chhabra P. Maternal Near Miss: An Indicator for Maternal Health and Maternal Care. Indian Journal of Community Medicine. 2014; 39: 132. Https://Doi.Org/10.4103/0970-0218.137145.
- World Health Organization (WHO). Encyclopedia of Disaster Relief. 2011; Https://Doi.Org/10.4135/9781412994064.N318.
- Say L, Souza JP, Pattinson RC; WHO working group on Maternal Mortality and Morbidity classifications. Maternal near miss--towards a standard tool for monitoring quality of maternal health care. Best Pract Res Clin Obstet Gynaecol. 2009 Jun;23(3):287-96. doi: 10.1016/j.bpobgyn.2009.01.007. Epub 2009 Mar 19. PMID: 19303368.
- Liyew EF, Yalew AW, Afework MF, Essén B. Incidence and causes of maternal near-miss in selected hospitals of Addis Ababa, Ethiopia. PLoS One. 2017 Jun 6;12(6):e0179013. doi: 10.1371/journal.pone.0179013. PMID: 28586355; PMCID: PMC5460898.
- Geleto A, Chojenta C, Taddele T, Loxton D. Incidence of maternal near miss among women in labour admitted to hospitals in Ethiopia. Midwifery. 2020 Mar;82:102597. doi: 10.1016/j.midw.2019.102597. Epub 2019 Dec 4. PMID: 31862558.
- Hirshberg A, Srinivas SK. Epidemiology of maternal morbidity and mortality. Semin Perinatol. 2017 Oct;41(6):332-337. doi: 10.1053/j.semperi.2017.07.007. Epub 2017 Aug 18. PMID: 28823579.
- Ali AA, Khojali A, Okud A, Adam GK, Adam I. Maternal near-miss in a rural hospital in Sudan. BMC Pregnancy Childbirth. 2011 Jun 29;11:48. doi: 10.1186/1471-2393-11-48. PMID: 21714881; PMCID: PMC3141596.
- Pattinson RC, Hall M. Near misses: a useful adjunct to maternal death enquiries. Br Med Bull. 2003;67:231-43. doi: 10.1093/bmb/ldg007. PMID: 14711767.
- Taha U. Reducing Maternal Mortality from Direct Obstetric Causes during 2013 in Sudan. Journal of US-China Medical Science. 2014; 11: 4. Https://Doi.Org/10.17265/1548-6648/2014.04.006.
- Nelissen EJ, Mduma E, Ersdal HL, Evjen-Olsen B, van Roosmalen JJ, Stekelenburg J. Maternal near miss and mortality in a rural referral hospital in northern Tanzania: a cross-sectional study. BMC Pregnancy Childbirth. 2013 Jul 4;13:141. doi: 10.1186/1471-2393-13-141. PMID: 23826935; PMCID: PMC3716905.
- Negash A, Sertsu A, Mengistu DA, Tamire A, Birhanu Weldesenbet A, Dechasa M, Nigussie K, Bete T, Yadeta E, Balcha T, Debele GR, Dechasa DB, Fekredin H, Geremew H, Dereje J, Tolesa F, Lami M. Prevalence and determinants of maternal near miss in Ethiopia: a systematic review and meta-analysis, 2015-2023. BMC Womens Health. 2023 Jul 19;23(1):380. doi: 10.1186/s12905-023-02523-9. Erratum in: BMC Womens Health. 2023 Aug 1;23(1):402. PMID: 37468876; PMCID: PMC10357694.
- Owolabi O, Riley T, Juma K, Mutua M, Pleasure ZH, Amo-Adjei J, Bangha M. Incidence of maternal near-miss in Kenya in 2018: findings from a nationally representative cross-sectional study in 54 referral hospitals. Sci Rep. 2020 Sep 16;10(1):15181. doi: 10.1038/s41598-020-72144-x. PMID: 32939022; PMCID: PMC7495416.
- Nansubuga E, Ayiga N, Moyer CA. Prevalence of maternal near miss and community-based risk factors in Central Uganda. Int J Gynaecol Obstet. 2016 Nov;135(2):214-220. doi: 10.1016/j.ijgo.2016.05.009. Epub 2016 Aug 1. PMID: 27553504.
- Kumela L, Tilahun T, Kifle D. Determinants of Maternal Near Miss in Western Ethiopia. Ethiop J Health Sci. 2020 Mar;30(2):161-168. doi: 10.4314/ejhs.v30i2.3. PMID: 32165805; PMCID: PMC7060379.
- Gedefaw M, Gebrehana H, Gizachew A, Taddess F. Assessment of maternal near-missat Debre Markos referral hospital, Northwest Ethiopia: five years’ experience. Open Journal of Epidemiology. 2014; 4(04): 199-207.
- Woldeyes WS, Asefa D, Muleta G. Incidence and determinants of severe maternal outcome in Jimma University teaching hospital, south-West Ethiopia: a prospective cross-sectional study. BMC Pregnancy Childbirth. 2018 Jun 20;18(1):255. doi: 10.1186/s12884-018-1879-x. PMID: 29925329; PMCID: PMC6011243.
- Firoz T, Trigo Romero CL, Leung C, Souza JP, Tunçalp Ö. Global and regional estimates of maternal near miss: a systematic review, meta-analysis and experiences with application. BMJ Glob Health. 2022 Apr;7(4):e007077. doi: 10.1136/bmjgh-2021-007077. PMID: 35387768; PMCID: PMC8987675.
- Tura AK, Stekelenburg J, Scherjon SA, Zwart J, van den Akker T, van Roosmalen J, Gordijn SJ. Adaptation of the WHO maternal near miss tool for use in sub-Saharan Africa: an International Delphi study. BMC Pregnancy Childbirth. 2017 Dec 29;17(1):445. doi: 10.1186/s12884-017-1640-x. PMID: 29284433; PMCID: PMC5747119.
- Egal JA, Kiruja J, Litorp H, Osman F, Erlandsson K, Klingberg-Allvin M. Incidence and causes of severe maternal outcomes in Somaliland using the sub-Saharan Africa maternal near-miss criteria: A prospective cross-sectional study in a national referral hospital. Int J Gynaecol Obstet. 2022 Dec;159(3):856-864. doi: 10.1002/ijgo.14236. Epub 2022 May 23. PMID: 35490394; PMCID: PMC9790269.
- Aduloju OP. Profile of Maternal Near-missand Determinant Factors in a Teaching Hospital, Southwestern Nigeria. International Journal of Reproduction, Contraception, Obstetrics and Gynecology. 2018’; 7: 3450. Https://Doi.Org/10.18203/2320-1770.Ijrcog20183752.
- Souza JP, Cecatti JG, Faundes A, Morais SS, Villar J, Carroli G, Gulmezoglu M, Wojdyla D, Zavaleta N, Donner A, Velazco A, Bataglia V, Valladares E, Kublickas M, Acosta A; World Health Organization 2005 Global Survey on Maternal and Perinatal Health Research Group. Maternal near miss and maternal death in the World Health Organization's 2005 global survey on maternal and perinatal health. Bull World Health Organ. 2010 Feb;88(2):113-9. doi: 10.2471/BLT.08.057828. Epub 2009 Sep 11. PMID: 20428368; PMCID: PMC2814475.
- Mpembeni RN, Killewo JZ, Leshabari MT, Massawe SN, Jahn A, Mushi D, Mwakipa H. Use pattern of maternal health services and determinants of skilled care during delivery in Southern Tanzania: implications for achievement of MDG-5 targets. BMC Pregnancy Childbirth. 2007 Dec 6;7:29. doi: 10.1186/1471-2393-7-29. PMID: 18053268; PMCID: PMC2222241.
- de Lima THB, Amorim MM, Buainain Kassar S, Katz L. Maternal near miss determinants at a maternity hospital for high-risk pregnancy in northeastern Brazil: a prospective study. BMC Pregnancy Childbirth. 2019 Aug 1;19(1):271. doi: 10.1186/s12884-019-2381-9. PMID: 31370813; PMCID: PMC6670122.
- Mbachu II, Ezeama C, Osuagwu K, Umeononihu OS, Obiannika C, Ezeama N. A cross sectional study of maternal near miss and mortality at a rural tertiary centre in southern nigeria. BMC Pregnancy Childbirth. 2017 Jul 28;17(1):251. doi: 10.1186/s12884-017-1436-z. PMID: 28754161; PMCID: PMC5534124.
- Ismail MT, Ramadan MC, Mohamed AS, Elshishini AM. Clinical Intervention for Maternal Near-missCases in El Galaa Teaching Hospital. The Egyptian Journal of Hospital Medicine (July 2018). 2018; 72(1): 3839-3845.
- Madouea GB, Abdelsalama S, Aliou DMB, Offi A, Emile S, Pallai E, Obelix A. Maternal near-miss in N’Djamena Mother and Child Hospital, Chad. South Sudan Medical Journal. 2017; 10(2): 28-31.
- Donati S, Senatore S, Ronconi A; Regional Maternal Mortality Working Group. Obstetric near-miss cases among women admitted to intensive care units in Italy. Acta Obstet Gynecol Scand. 2012 Apr;91(4):452-7. doi: 10.1111/j.1600-0412.2012.01352.x. Epub 2012 Feb 22. PMID: 22229438.
- Ministry of Health. Smoking Habit of Brazilians Drops by 40% According to Ministry of Health. Nursing (São Paulo). 2019; 22: 302.
- Donati S, Senatore S, Ronconi A. Obstetric Near-missCases among Women Admitted to Intensive Care Units in Italy. Scandinavian Journal of Obstetrics and Gynecology. US. National Library of Medicine, Pubmed. Ncbi. Nlm.Nih. Gov/22229438/.
- Who statement on cesarean section rates. Reproductive Health Matters, vol. 23, no. 45, Jan. 2015, pp. 149–150, https://doi.org/10.1016/j.rhm.2015.07.007.
- Alemu FM, Fuchs MC, Martin Vitale T, Abdalla Mohamed Salih M. Severe maternal morbidity (near-miss) and its correlates in the world's newest nation: South Sudan. Int J Womens Health. 2019 Mar 19;11:177-190. doi: 10.2147/IJWH.S160022. PMID: 30936753; PMCID: PMC6429996.
- Dessalegn FN, Astawesegn FH, Hankalo NC. Factors Associated with Maternal Near Miss among Women Admitted in West Arsi Zone Public Hospitals, Ethiopia: Unmatched Case-Control Study. J Pregnancy. 2020 Jul 2;2020:6029160. doi: 10.1155/2020/6029160. PMID: 32695514; PMCID: PMC7352151.
- Domingues RM, Dias MA, Schilithz AO, Leal MD. Factors associated with maternal near miss in childbirth and the postpartum period: findings from the birth in Brazil National Survey, 2011-2012. Reprod Health. 2016 Oct 17;13(Suppl 3):115. doi: 10.1186/s12978-016-0232-y. PMID: 27766973; PMCID: PMC5073804.
- El-Agwany Samy A. Severe Maternal Outcomes: World Health Organization Maternal near-missand Maternal Mortality Criteria in University Tertiary Hospital Egypt. Apollo Medicine. 2019; 16: 74. Https://Doi.Org/10.4103/Am.Am_10_19.
- Maternal near-missOperational Guidelines. Scribd, Scribd. Www.Scribd.Com/Document/440452737/Maternal-Near-Miss-Operational-Guidelines-1. Accessed 5 Oct. 2023.
- Profile of Maternal near-missand Determinant Factors in a Teaching. Www.Researchgate.Net/Profile/OlusolaAduloju/Publication/323376727_Profile_of_Maternal_Near_Miss_and_Determinant_Factors_in_a_Teaching_Hospital_Southwestern_Nigeria/Links/5a90e728aca27214056238f8/Profile-of-Maternal-Near-Miss-and-Determinant-Factors-in-a-Teaching-Hospital-Southwestern-Nigeria.Pdf. Accessed 5 Oct. 2023.
- Tunçalp O, Hindin MJ, Souza JP, Chou D, Say L. The prevalence of maternal near miss: a systematic review. BJOG. 2012 May;119(6):653-61. doi: 10.1111/j.1471-0528.2012.03294.x. PMID: 22489760.
- Zargar M. Severe Maternal Morbidity and Near Misses in Two Tertiary Referral Hospitals in Iran. Jentashapir Journal of Health Research. 2015; 6: 2. Https://Doi.Org/10.5812/Jjhr.6(2)2015.25886.