More Information
Submitted: October 16, 2023 | Approved: November 06, 2023 | Published: November 07, 2023
How to cite this article: Maestri CA, Antoniazzi RB, Maestri IC, Fernandes RC, Fonseca FV, et al. The Effectiveness of Honey-Based Ferric Perchloride Paste on Post-conization in the Cicatricial and Infectious Context: A Randomized Clinical Trial. Clin J Obstet Gynecol. 2023; 6: 179-184.
DOI: 10.29328/journal.cjog.1001148
Copyright License: © 2023 Maestri CA, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Congenital cervical immature teratoma; Immature teratoma; Cervical teratoma; Extrauterine intrapartum treatment procedure; Case report
The Effectiveness of Honey-Based Ferric Perchloride Paste on Post-conization in the Cicatricial and Infectious Context: A Randomized Clinical Trial
Carlos Afonso Maestri1* , Rodolfo Belz Antoniazzi2
, Rodolfo Belz Antoniazzi2 , Isabela Ceschin Maestri2
, Isabela Ceschin Maestri2 , Rafaela Ceschin Fernandes3
, Rafaela Ceschin Fernandes3 and Fernanda Villar Fonseca4
and Fernanda Villar Fonseca4
1Positivo University and Erasto Gaertner Hospital, Curitiba, Paraná, Brazil
2Universidade Positivo, Curitiba, Paraná, Brazil
3Faculdade Pequeno Principe, Curitiba, Paraná, Brazil
4Positivo University, Curitiba, Paraná, Brazil and Erasto Gaertner Hospital, Brazil
*Address for Correspondence: Carlos Afonso Maestri, Positivo University and Erasto Gaertner Hospital, R. Dr Ovande do Amaral, 201- Jardim das Américas, Curitiba, Paraná, Brazil, CEP 81520-060, Brazil, Email: [email protected]
Introduction: The skills, the techniques utilized in the conization and the hemostasis directly affect the healing process of the cervix tissue. Excessively large excisions and unnecessary use of electrocautery or hemostatic sutures are examples of procedures that may negatively affect the scar cascade and wound healing.
Objective: The purpose of this study was to examine the effectiveness of honey-based ferric perchloride paste (HBFPP) in reducing bleeding and infection post-conization procedure.
Methods: Prospective randomized clinical trial with a sample of 142 patients randomized in two groups: 78 patients who used the HBFPP (intervention) and 64 patients who did not use the HBFPP (control). Statistical analysis was performed utilizing a significance level of 95%. The Chi-Square test and Fisher’s exact test were applied.
Results: Results showed that the mean score of the amount of blood lost was lower in the intervention group compared to the control group. The main complaints reported by the two groups in the postoperative period were discomfort in the genitourinary system, heavy bleeding after surgery, and post-operative infection, but not significantly different among both groups. The control group needed further intervention due to excessive bleeding in comparison with the intervention group.
Conclusion: The use of HBFPP reduced the amount of blood lost in the postoperative period of conization surgery.
Preventive measures and early detection had a positive impact on the reduction of cervical cancer [1]. According to the American Cancer Society, the incidence per 100,000 inhabitants [2], in the last 40 years decreased by 7.4%. These measures may also reduce the number of cases of invasive carcinoma and increase the diagnosis of precursor lesions, also called cervical intraepithelial neoplasia (CIN). The ratio between CIN and invasive carcinoma went from 8.3 in 2,000 to approximately 13.8 in 2010 [3].
When CINs are identified as high-grade lesions, conization is the preferred type of treatment because it favors the histopathological diagnosis, as opposed to other aggressive methods, and treatment [4].
The conization consists of complete excision of the lesion and local cauterization. Following the excision, a series of scar cascades appear, which are responsible for the vitality and recovery of the affected area. The professional´s expertise, the techniques applied in the excision procedure, and the hemostasis directly affect the capacity of cervix tissue recovery [5]. Excessively large excisions and unnecessary use of electrocautery or hemostatic sutures are examples of procedures that may affect the scar cascade and interfere negatively with the healing process [6].
Following conization, the most common complications include infertility, cervical stenosis, difficulty or inability to screen new lesions problems in childbirth, and potential increased risk of prematurity [7]. The incidence of genital tract infection varies from 0.8 to 36%, depending on several factors such as the operative technique and even the definition of infection. Additionally, the incidence of genital tract infection may be higher if major bleeding occurs. If prolonged vaginal bleeding appears following cervical transformation zone excision (24 hours after the procedure), the incidence of infectious complications would be significantly greater. However, excisional procedures are often associated with prolonged vaginal discharge, which is not necessarily infectious but may be the result of the healing processes and edema induced by the procedure [8,9].
The most common complication in the postoperative period is hemorrhage, usually occurring in 10% - 20% of the cases. Hemorrhages are frequent causes of re-hospitalization, blood transfusion, and late interventions [10]. The surgical technique used during the procedure is a critical step in achieving complete hemostasis and eliminating the possibilities of future morbidities [10].
A wide variety of conization methods and techniques have been described over the past decades. Nevertheless, gynecologists are still debating the optimal cost-benefit options of the procedure and its many possibilities and effectiveness [11].
The honey-based ferric perchloride paste (HBFPP) was created by the Cervical Pathology team at Hospital Erasto Gaertner and manufactured by the hospital pharmacy to improve the results of the postoperative period following conization. The paste contains ferric perchloride, honey (Apis mellifera), and stabilizers.
The purpose of this study was to examine the effectiveness of HBFPP in preventing postoperative bleeding, and as secondary objectives to evaluate infections and the side effects of using HBFPP. The addition of honey in the ferric perchloride solution provides better adhesion to the postoperative wound of hemostatic materials, such as gauze and tampons, with better administration and, consequently, may have a better therapeutic response. In addition, honey has a high osmolarity due to its glucose concentration and antiseptic properties7. In addition, we analyzed whether these characteristics can help reduce postoperative infection and contribute to hemostasis.
A randomized prospective clinical trial with 142 patients, aged 18 to 65 years, undergoing conization surgery, treated at the cervical pathology outpatient clinic of the Erasto Gaertner hospital, who answered the research evaluation questionnaires to assess factors influencing bleeding and its evolution and bleeding. Questionnaires completed by the patient and returned correctly in the postoperative consultation about 20 days after the procedure. The patients were further divided into two groups: 78 were in the intervention group that used the HBFPP and 64 were in the control group. The intervention group used a tampon brand OB, large-size Johnsons & Johnson with its distal third soaked with HBFPP immediately after the conization procedure and the control group used a tampon brand OB, large-size Johnsons & Johnson without any product. Exclusion criteria were: women with hematological diseases interfering with coagulation, menstrual bleeding, previous pelvic radiotherapy, continuous use of heparin or another coagulation inhibitor, and failure to complete a questionnaire with the menstrual pictogram.
All participants signed the Informed Consent Form. The Institutional Review Board of “Hospital Erasto Gaertner” approved the study, CAEE (submission for ethical review) number 03394418.2.0000.0098 and registered at “The Brazilian Registry of Clinical Trials (ReBEC)”, id 14332/subm id 17147.
The loop electrosurgical excision procedure (LEEP) was adopted for all the study samples, including large loop excision of the transformation zone or cone biopsy with loop excision. To improve postoperative hemostasis, a tampon was placed on the vaginal vault in both groups after the surgical procedure. Both the surgeon and the patient were informed at that time whether or not HBFPP would be administered to the tampon. The use of the HBFPP was randomly selected, with the assistance of a virtual tool [12].
To examine the effectiveness of the HBFPP, the study was divided into two parts. The first part included a questionnaire administered by the researchers who attended the preoperative and intraoperative periods and the follow-up outpatient consultations. The second part consisted of the patient's subjective assessment using a menstrual pictogram, filled in by the patient and returned at the follow-up appointment.
In a systematic review of methods for assessing menstrual blood loss, pictographic methods, which are graphic representations of bloody pads, have had consistently high sensitivity and specificity (> 80%), and unlike other illustrative methods, it is comparable to the aforementioned alkaline hematin method, regarded as the gold standard [13].
The menstrual pictogram, described by Wyatt, et al. [14], was utilized. It assesses the total blood loss and has its own score, correlating the image with the blood volume in milliliters.
The software Prisma 5.0 was utilized for the statistical analysis. The Chi-square test and Fisher´s Exact test were applied to analyze the statistically significant relations of the groups and the variables. A p - value < 0.05 was defined as statistically significant.
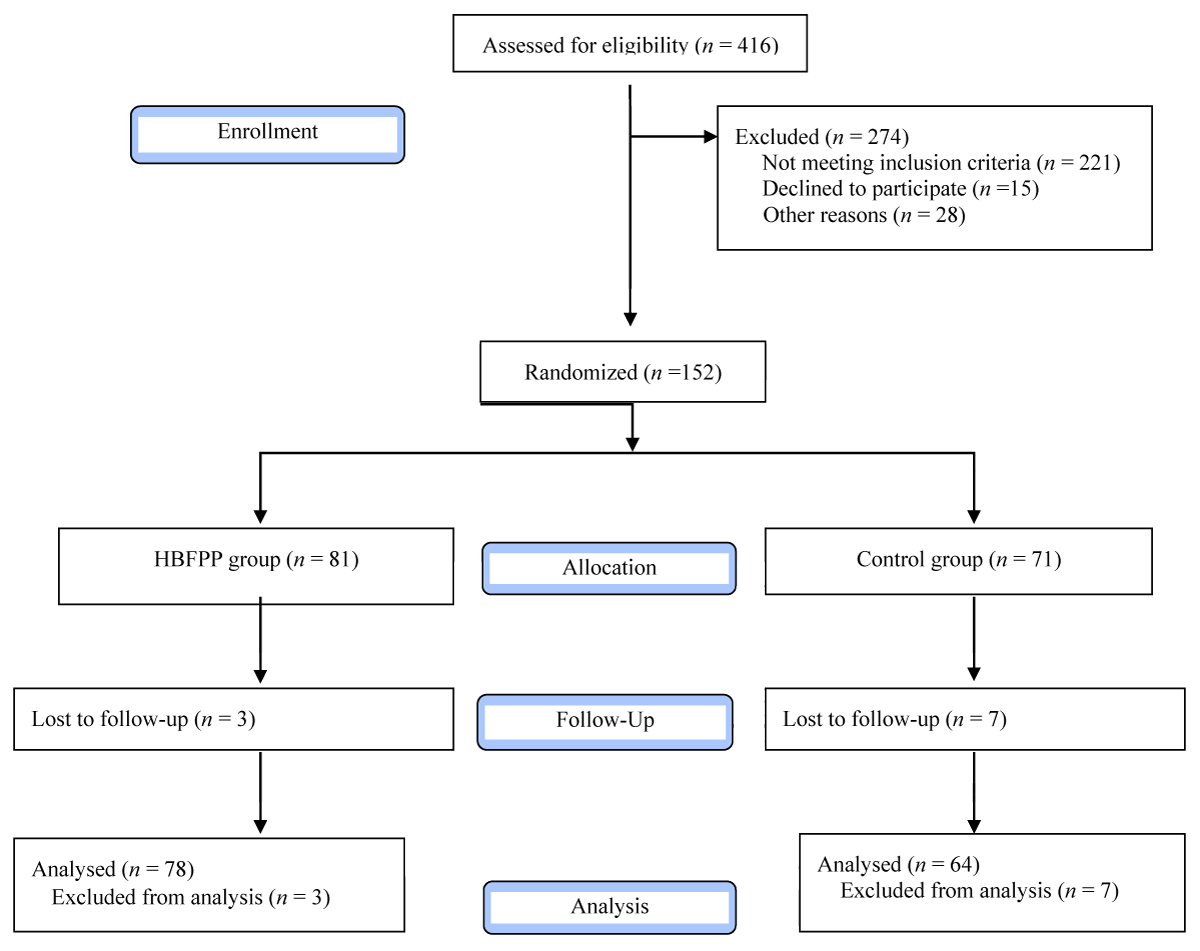
The flowchart describing the study design is shown in Figure 1.
Figure 1: Flowchart of the Study design.
The epidemiological data for both study groups is shown in Table 1.
| Table 1: Epidemiological data of the intervention and control groups. | |||
| Data | Intervention Group (n = 78) |
Control Group(n = 64) |
|
| Smoker | Yes | 23(29%) | 17(27%) |
| No | 55(71%) | 47(73%) | |
| Menopause | Yes | 12(15%) | 6(9%) |
| No | 66(85%) | 58(91%) | |
| Use of Contraception | Yes | 63(81%) | 48(75%) |
| No | 15(19%) | 16(25%) | |
| Comorbidities | Yes | 26(33%) | 14(22%) |
| No | 52(67%) | 50(78%) | |
| Nulliparous | Yes | 12(15%) | 12(19%) |
| No | 66(85%) | 52(81%) | |
| Indication of LEEP | CIN1 | 10 (13%) | 7 (11%) |
| CIN2 | 33 (42%) | 30 (47%) | |
| CIN3 | 34 (44%) | 24 (38%) | |
| HSIL | 1 (1%) | 2 (3%) | |
| LSIL | 0(0%) | 1 (1%) | |
| Who performed the procedure | Medical resident | 49 (63%) | 43 (67%) |
| Research fellow | 19 (24%) | 14 (22%) | |
| Medical staff | 10 (13%) | 7 (11%) | |
| Necessity of suture | Yes | 2 (3%) | 2 (3%) |
| No | 76 (97%) | 62 (97%) | |
| CIN: Cervical Intraepithelial Neoplasia; LSIL: Low-grade Squamous Intraepithelial Lesions; HSIL: High grade Squamous Intraepithelial Lesions; LEEP: Loop Electrosurgical Excision Procedure Source: Authors (2022) |
|||
The groups were homogeneous in terms of patient profile, with one of the few differential characteristics being the use or non-use of perchloride paste.
All the analyses were related to the amount of bleeding measured by the menstrual pictogram score [14] to assess the postoperative bleeding.
Table 2 shows the analysis of the postoperative bleeding score for the first seven days following the surgical procedure. The points were added until the seventh day and divided into: Day 1, Day 3 (the sum of the first three days), Day 5 (the sum of the first five days), and Day 7 (the sum of the first seven days).
| Table 2: Analysis of the postoperative bleeding score during a 7-day period. | |||||
| Day 1 (1st post-op) |
Day 3 (∑3 days) |
Day 5 (∑5 days) |
Day 7 (∑7 days) |
||
| Control | Mean | 3.53 | 7.32 | 10.39 | 14.10 |
| Intervention | Mean | 2.16 | 5.30 | 7.59 | 10.26 |
| Control | Standard deviation | 4.94 | 7.22 | 9.52 | 12.65 |
| Intervention | Standard deviation | 1.89 | 4.46 | 6.39 | 8.21 |
| p - value | 0.02 | 0.03 | 0.02 | 0.02 | |
| Source: Authors (2022) | |||||
There was a statistically significant difference between the two groups. Compared to the control group, the intervention group had a lower bleeding score.
The complaints reported by both groups during the postoperative period were divided into three major categories: 1) gynecological complaints, which included any genitourinary symptom or discomfort; 2) bleeding complaints, which included patients who specifically reported a problem at the follow-up visit, whether it was a perception of severe bleeding after surgery or a disruption in the menstrual cycle; 3) infection complaints, which included those suggestive of genitourinary infection, such as leukorrhea, vulvar pruritus, dysuria, and others, as shown in Table 3.
| Table 3: Postoperative complaints. | ||
| Variable | Control Group | Intervention Group |
| Gynecological Complaints | 12 (19%) | 12 (15%) |
| No complaints | 52 (81%) | 66 (85%) |
| Total | 64 | 78 |
| p - value | 0.59 | |
| Bleeding Complaints | 4 (6%) | 4 (5%) |
| No complaints | 60 (94%) | 74 (95%) |
| Total | 64 | 78 |
| p - value | 0.81 | |
| Infection Complaints | 6 (9%) | 7 (9%) |
| No complaints | 58 (91%) | 71 (91%) |
| Total | 64 | 78 |
| p - value | 0.93 | |
| Source: Authors (2022) | ||
Lastly, a comparison was established between the two groups, assessing the need for a re-approach due to excessive bleeding, either with a second cauterization attempt or a change in the hemostatic technique, suturing, or substance use, as shown in Table 4.
| Table 4: Comparison due to excessive bleeding between the two groups, assessing the need for a re-approach. | ||
| Variable | Control group |
Intervention group |
| re-approach | 5 (8%) | 2 (2%) |
| No re-approach | 59 (92%) | 76 (98%) |
| Total | 64 | 78 |
| The control group did not use HBFPB, intervention group used HBFPP p - value = 0.15 | ||
The objective of this study was to assess the effectiveness of the honey-based ferric perchloride paste (HBFPP) developed at Hospital Erasto Gaertner, following a post-conization procedure. The HBFPP was used to reduce the postoperative complications of the LEEP technique. So far, this is the first study on the use of the paste.
The ferric sulfate (Monsel Solution) has been used since the end of the 19th century because it creates hemostasis in epithelial ruptures, which is comparable to ferric perchloride [15]. The use of sulfate and ferric perchlorate was not investigated in any study, which may be explained by their chemical nature and the almost identical hemostatic response.
Epstein & Malbach (1964) concluded that the coagulative effect of Monsel’s solution was one of protein precipitation and denaturing, which mechanically sealed off small, bleeding vessels. Because they found no such coagulative effect when hemostasis was attempted with hydrochloric acid, they concluded that the ferric ions and not the acidic nature of the ferric subsulfate were responsible for the hemostatic qualities of Monsel’s solution [16].
A literature review on the use of Monsel's Solution (MS) compared to other topical hemostatic agents in obstetric bleeding states that most of the evidence on the effectiveness of the MS is anecdotal, and minor bleeding is commonly accepted. There is a paucity of well-designed studies and clinical trials comparing their effectiveness with other hemostatic agent [17].
Martin, et al. in their review provided only two comparisons between MS and other approaches, which favored the use of MS, specifically for interventions to prevent blood loss in the treatment of cervical intraepithelial neoplasia [18].
Compared to hemostatic suturing, the use of MS reduced significantly perioperative blood loss (mean difference (MD) = -22.00, 95% confidence interval CI -23.09 to -20.91), but not the risk of primary and secondary hemorrhage. MS also showed favorable results in decreasing the risk of dysmenorrhea, cervical stenosis, and unsatisfactory colposcopy. Compared to electrocautery, it did not show a statistically significant difference in perioperative blood loss (MD = 4.82, 95% CI -3.45 to 13.09) [18].
A clinical trial conducted in 1995 by Tangtrakul, et al. with 142 patients, compared suturing and the use of MS in two groups. The results showed that there was no statistical significance in the operative blood loss while using the MS. However, there was a significant difference in the assessment of hemorrhage requiring treatment after the first 24 hours. The trial concluded that the traditional method using suture should be replaced by MS [19].
A study performed by Hilal, et al. in 2016, used a score from a menstrual pictogram for the quantitative assessment of blood loss, with a sample of 145 patients randomized into two groups after puncture for cervical biopsy: the intervention group, who used the MS and the control group who did not. The results showed lower amounts of bleeding with MS after 15 minutes, 3 hours, and 6 hours after the procedure. However, after 24 hours, there was no significant difference in scores between the two groups. The complication rate was 9% in the intervention group and 3% in the control group and was not statistically significant (p = 0.2) [11].
Tam, et al. also examined the hemostatic response of the MS following a biopsy of the cervical region in a sample of 96 individuals [20]. The results showed that 95% of the women presented bleeding at less than 10 ml, assessed by the colposcopist. However, a considerable proportion of the women experienced bleeding for more than one week (20.8% for 7 to 13 days, and 11.5% for 14 days or more), and 35% did not heal completed 4 weeks post-procedure, apparently suggesting that prolonged bleeding and delayed healing is related to the use of MS. The authors found no association between the severity and duration of bleeding and menopausal status, number of biopsies, histology, or blood loss during biopsy [20]. In addition, 4.1% of the patients reported vaginal pain in the perineal region and MS leakage to the outside. It was emphasized that the irritation that the product may bring to the skin, leading to tissue necrosis is well recognized, and it is critical to use a minimal amount [20].
Given its more pasty and astringent consistency, the honey-based solution used in this study had no issues related to its exteriorization, unlike the conventional liquid solution. The administration of MS, whether done directly on the lesion or using a tissue (e.g., gauze or tampon), is considerably easier to handle and resembles a pasty glue.
Kietpeerakool, et al. conducted a randomized controlled trial with 297 patients, divided into two groups. The intervention group used the MS and the control group used povidone-iodine with a cotton swab [21]. The authors concluded that MS reduced the duration and the persistence of bleeding for 2 weeks or more. However, no significant difference was found for complications that required intervention due to severe blood loss and infections. Application of the product may not be necessary if there is adequate hemostasis [21]. The trial has also presented an interesting assessment: the complaint of vaginal irritation (8.57%) was higher in the MS group, but there was no significant difference (p = 0.07). The authors also reported that some adverse effects have already been observed, however, apparently, they are related to the amount, recommending that the solution should be applied with a cotton swab only on the injured area [21]. This finding reinforces the Effectiveness of a pasty solution, such as honey, to improve the results and to reduce adverse effects.
In another study that examined the use of MS after a conization procedure, Doyle, et al evaluated 125 women randomly assigned to two groups. The intervention group used the MS after the procedure and the control group did not use it. Compared to the control group, the intervention group did not have a reduction in the amount and duration of bleeding. They also found that the size of the excision was decisive for the quantitative determination of blood loss and bleeding for more than 14 days was found to have a statistically significant relationship with larger excisions (odds ratio 3.5.95% CI 1.2- 9.9).
The authors concluded that the use of MS did not appear to significantly affect bleeding and based on the evidence from the study, it cannot be recommended routinely [22].
Unlike Doyle, et al, the present findings showed a statistically significant difference in blood loss between the two groups. It was also found that the mean and variability of the scores of the control group were higher than those of the intervention group. This may suggest less variation and unpredictability in the outcome of patients who used HBFPP, reducing blood loss, making the amount of blood loss more predictable and therefore resulting in fewer negative outcomes or post-surgical complications.
No other studies published that evaluated Monsel's solution or ferric perchloride as a prospective randomized clinical trial associated with tampons were found. In the institution where this study was conducted before the pandemic, over 1,000 conizations were performed a year. The use of this technique was quite evident and beneficial in reducing the number of late interventions to treat cervical bleeding. This presents evidence to address issues raised by some studies that showed that MS is not effective on hemostasis, and perhaps the possible reduction in bleeding is attributable only to the use of adequate mechanical hemostasis (such as gauze) for its administration.
There was no difference between intervention and control groups in terms of complaints brought up by the patient during the postoperative follow-up visit, whether they were more generalized in the genitourinary system, or more specific in terms of the perception of bleeding or suggestive of infection.
Using the current methodology, it was not possible to verify a statistically significant difference between the need to modify the surgical technique or to begin a new intervention after surgery due to bleeding (p = 0.26). This may be explained by the small sample size. Larger samples may be required to assess surgical complications and the use of a mechanical hemostatic method such as tampons, in reducing bleeding complications, although it still quantitatively exhibits greater bleeding.
There were no complaints of pain in the perianal area due to solution extravasation, as reported by 4.1% of patients in a previous study [20] published. In Kietpeerakool, et al, the complaint of vaginal irritation was reported by 8.57% of patients who used MS [21]. According to the anamnesis report, in this study, only two women with nonspecific complaints of pruritus in the HBFPP group were found, one associated with discharge, and one in the control group with a suspected allergy to the tampon.
The most remarkable finding of the present study is the use of a paste with medium adherence, which allowed the use of a smaller amount in the tampon, with less risk of extravasation and contact with the intact vaginal mucosa or skin of the perianal area, which may cause discomfort or even a more severe outcome, such as wound necrosis. Due to the small sample size, it was not possible to demonstrate a reduction in the incidence of pelvic inflammatory disease (PID) in the postoperative course. Because it is a hyperosmolar honey-based solution, it may have a bactericidal effect (a characteristic of honey), and as a result, there have been no further incidences of PID, as intra or postoperative antibiotics were not utilized at all.
This study showed that the honey-based ferric perchloride product, developed at Hospital Erasto Gaertner, was able to reduce the amount of blood loss in the postoperative period of conization surgery. Based on the menstrual pictogram score utilized, which corresponded to milliliters of blood volume, during the 7-day evaluation, the intervention group had statistically significantly lower bleeding mean compared to the control group.
Although the results did not achieve a statistically significant difference in relation to the necessity of rechallenging due to bleeding, it suggests that the use of HBFPP may reduce the probability of negative outcomes and postoperative complications, based on the lower average post-operative bleeding volume, which may result in improved post-operative recovery.
Contributions
All the authors contributed to the study design, data collection, interpretation, wording, and critical review. They approved the final version for publication.
Funding sources: The study was funded by the investigators and their institutions.
- INCA. Instituto Nacional do Câncer. https://www.inca.gov.br/controle-do-cancer-do-colo-do-utero/acoes-de-controle/deteccao-precoce.
- ACS. Analysis Tool. American Cancer Society - Cancer Facts & AMP; Statistics. https://cancerstatisticscenter.cancer.org/#!/data-analysis/IncidenceTrend.
- Mnistry of Health. 3 2013 Primary Care Notebooks from the Virtual Health Library of the Ministry of Health www.saude.gov.br/bvs control of cervical and breast cancers 13 2013 primary care notebooks from the Virtual Health Library of the Ministry of Health www.saude .gov.br/bvs control of cervical and breast cancers. 5 Sep. 2006.
- Juliato CRT. Correlation between the Histological Report of Biopsy and Conization by the Loop Electrosurgical Excision Procedure (LEEP) in the Treatment of Cervical Intraepithelial Neoplasia. Rev Bras Ginecol Obstet. 2000; 22: 65-70.
- Kauvar A, Hruza G. Principles and Practices in Cutaneous Laser Surgery. In: Kauvar A, Hruza G. (Eds.). Principles and Practices in Cutaneous Laser Surgery. 1. ed. Boca Raton: CRC Press, 2005; 1: 3-75.
- Maffini CF. Cervix healing after excisional treatments for intraepithelial neoplasias: a practical view.
- Monteiro AC, Russomano FB, Camargo MJ, Silva KS, Veiga FR, Oliveira RG. Cervical stenosis following electrosurgical conization. Sao Paulo Med J. 2008 Jul;126(4):209-14. doi: 10.1590/s1516-31802008000400002. PMID: 18853028.
- Kietpeerakool C, Chumworathayi B, Thinkhamrop J, Ussahgij B, Lumbiganon P. Antibiotics for infection prevention after excision of the cervical transformation zone. Cochrane Database Syst Rev. 2017 Jan 21;1(1):CD009957. doi: 10.1002/14651858.CD009957.pub2. PMID: 28109160; PMCID: PMC6464760.
- Dane C, Dane B, Cetin A, Erginbas M. Haemostasis after cold-knife conisation: a randomised prospective trial comparing cerclage suture versus electro-cauterization. Aust N Z J Obstet Gynaecol. 2008 Jun;48(3):343-7. doi: 10.1111/j.1479-828X.2008.00853.x. PMID: 18532969.
- Santesso N, Mustafa RA, Wiercioch W, Kehar R, Gandhi S, Chen Y, Cheung A, Hopkins J, Khatib R, Ma B, Mustafa AA, Lloyd N, Wu D, Broutet N, Schünemann HJ. Systematic reviews and meta-analyses of benefits and harms of cryotherapy, LEEP, and cold knife conization to treat cervical intraepithelial neoplasia. Int J Gynaecol Obstet. 2016 Mar;132(3):266-71. doi: 10.1016/j.ijgo.2015.07.026. Epub 2015 Nov 28. PMID: 26643302.
- Hilal Z, Rezniczek GA, Tettenborn Z, Hefler LA, Tempfer CB. Efficacy of Monsel Solution After Cervical Biopsy: A Randomized Trial. J Low Genit Tract Dis. 2016 Oct;20(4):312-6. doi: 10.1097/LGT.0000000000000234. PMID: 27428608.
- Sorteador. Sorteio de Nomes. Sorteador.com.br. https://sorteador.com.br/sorteio-de-nomes.
- Magnay JL, O'Brien S, Gerlinger C, Seitz C. A systematic review of methods to measure menstrual blood loss. BMC Womens Health. 2018 Aug 22;18(1):142. doi: 10.1186/s12905-018-0627-8. PMID: 30134884; PMCID: PMC6106944.
- Wyatt KM, Dimmock PW, Walker TJ, O'Brien PM. Determination of total menstrual blood loss. Fertil Steril. 2001 Jul;76(1):125-31. doi: 10.1016/s0015-0282(01)01847-7. PMID: 11438330.
- Garrett AP, Wenham RM, Sheets EE. Monsel's Solution: A Brief History. J Low Genit Tract Dis. 2002 Oct;6(4):225-7. doi: 10.1097/00128360-200210000-00006. PMID: 17051027.
- Epstein E, Maibach HI. Monsel's solution; history, chemistry, and efficacy. Arch Dermatol. 1964 Aug;90:226-8. doi: 10.1001/archderm.1964.01600020094022. PMID: 14162333.
- Miller DT, Roque DM, Santin AD. Use of Monsel solution to treat obstetrical hemorrhage: a review and comparison to other topical hemostatic agents. Am J Obstet Gynecol. 2015 Jun;212(6):725-35. doi: 10.1016/j.ajog.2014.12.029. Epub 2015 Jan 8. PMID: 25577672; PMCID: PMC4457701.
- Martin-Hirsch PP, Bryant A. Interventions for preventing blood loss during the treatment of cervical intraepithelial neoplasia. Cochrane Database Syst Rev. 2013 Dec 4;2013(12):CD001421. doi: 10.1002/14651858.CD001421.pub3. PMID: 24302533; PMCID: PMC6513534.
- Tangtrakul S, Srisupundit S, Linasmita V, Bullangpoti S, Israngura N, Wilailak S, Panijayanusondthi O. A randomized study comparing suture with non-suture cold-knife conization. J Obstet Gynaecol (Tokyo 1995). 1995 Dec;21(6):587-91. doi: 10.1111/j.1447-0756.1995.tb00917.x. PMID: 8640470.
- Tam KF, Lee TP, Ngan HY. Hemostasis following cervical punch biopsy using Monsel's solution. Int J Gynaecol Obstet. 2005 Feb;88(2):160-1. doi: 10.1016/j.ijgo.2004.11.017. Epub 2005 Jan 7. PMID: 15694100.
- Kietpeerakool C, Srisomboon J, Suprasert P, Cheewakriangkrai C, Charoenkwan K, Siriaree S. Routine prophylactic application of Monsel's solution after loop electrosurgical excision procedure of the cervix: is it necessary? J Obstet Gynaecol Res. 2007 Jun;33(3):299-304. doi: 10.1111/j.1447-0756.2007.00528.x. PMID: 17578359.
- Doyle M, Warwick A, Redman C, Hillier C, Chenoy R, O'Brien S. Does application of Monsel's solution after loop diathermy excision of the transformation zone reduce post operative discharge? Results of a prospective randomised controlled trial. Br J Obstet Gynaecol. 1992 Dec;99(12):1023-4. doi: 10.1111/j.1471-0528.1992.tb13714.x. PMID: 1341890.