More Information
Submitted: September 19, 2023 | Approved: October 09, 2023 | Published: October 10, 2023
How to cite this article: Suliman AA, Abdelrahman GM, Ahmed HSI, Ibrahim AS, Hammad KMA, et al. Postdate Pregnancy Maternal and Fetal Outcomes among Sudanese Women. Clin J Obstet Gynecol. 2023; 6: 165-171.
DOI: 10.29328/journal.cjog.1001146
Copyright License: © 2023 Suliman AA, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Postdate; Pregnancy; Maternal; Fetal; Outcomes; Sudanese; Women
Abbreviations: ANC: Antenatal Care; CTG: Cardiotocography; CRH: Corticotrophin-Releasing Hormone; EDC: Ethics Review Committee; FM: Fetal Movements; FHR: Fetal Heart Rate; ICU: Intensive Care Unit; NICU: Neonatal Intensive Care Unit; PPH: Postpartum Hemorrhage; SMSB: Sudan Medical Specialization Board
Postdate Pregnancy Maternal and Fetal Outcomes among Sudanese Women
Awadalla Abdelwahid Suliman1* , Gawahir Murad Abdelrahman2, Hajar Suliman Ibrahim Ahmed1, Abdelgadir Suliman Ibrahim3, Kabbashi Mohammed Adam Hammad2, Emad Abdalla Siddig Omer4 and Siddig Omer M Handady4
, Gawahir Murad Abdelrahman2, Hajar Suliman Ibrahim Ahmed1, Abdelgadir Suliman Ibrahim3, Kabbashi Mohammed Adam Hammad2, Emad Abdalla Siddig Omer4 and Siddig Omer M Handady4
1Assistant Professor, Consultant of Obstetrics and Gynecology, Faculty of Medicine, Al Neelain University, Sudan
2Specialist of Obstetrics and Gynecology, Sudan Medical Specialization Board (SMSB), Sudan
3Consultant Physician, MD of Internal Medicine Sudan, Sudan Medical Specialization Board (SMSB), Sudan
4Consultant of Obstetrics and Gynecology, Sudan Medical Specialization Board (SMSB), Sudan
*Address for Correspondence: Awadalla Abdelwahid Suliman, Assistant Professor, Consultant of Obstetrics and Gynecology, Faculty of Medicine, Al Neelain University, Khartoum, Sudan, Email: [email protected]
Background: Postdated pregnancy is one of the most common obstetric problems associated with increased maternal morbidity, prenatal morbidity, and mortality. Pregnancy at 37-40 weeks of gestation is called the term from the last menstrual period. If the pregnancy exceeds 40 weeks, it is called a postdated pregnancy, but when pregnancy is prolonged beyond 42 weeks, it is called post-maturity or post-term pregnancy.
Objective: This study aimed to determine the adverse effects of postdate pregnancy on mothers and fetuses.
Methodology: This was a descriptive, prospective, cross-sectional, hospital-based study conducted at Omdurman Maternity Hospital from January 2018 to June 2018.
An interview questionnaire was used to collect data. Data were collected by trained doctors in the labor room. One hundred and thirty-eight (138) postdated pregnant women were included in this study after obtaining informed consent through a structured questionnaire. Demographic and clinical data concerning personal history, booking status, mode of delivery, maternal complications, and fetal complications were recorded.
Results: During the study period, 2751 women delivered, of which 138 were postdated deliveries, with a prevalence of 5%. Most women's age range was 31-34 years 48.6%). Their education level was mostly secondary school (42%). Primigravida 65%), booked were 75.4%. Previous history of postdate pregnancy was 34.1%, normal vaginal delivery was 79 .7%, cesarean section was 14.5%, and instrumental delivery 5.8%.
Cesarean section indications were cervical dystocia (14.4%), cephalopelvic disproportion (9.5%), meconium-stained liquor with fetal distress (33.3%), pathological cardiotocography (CTC) (19%), and failure to progress (23.8%).
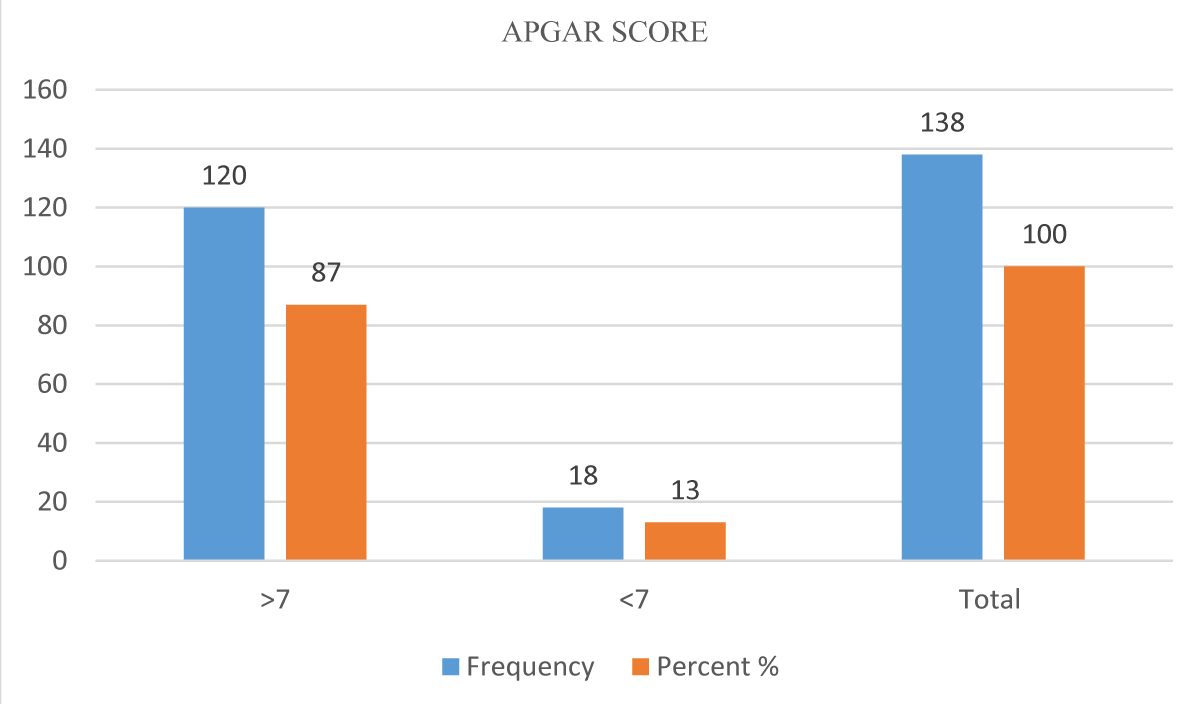
Maternal complications included post-partum hemorrhage (PPH) (7.2%), perineal tears (.7%, cervical tears (1.4%), and postpartum infections (1.4%). Fetal complications were 14.5%, Shoulder Dystocia 2.9%, asphyxia (6.5%), and meconium aspiration (5.1%). The mean APGAR score was 1.1667, less than three in only 3.6%, and > 7 in 86.9%.
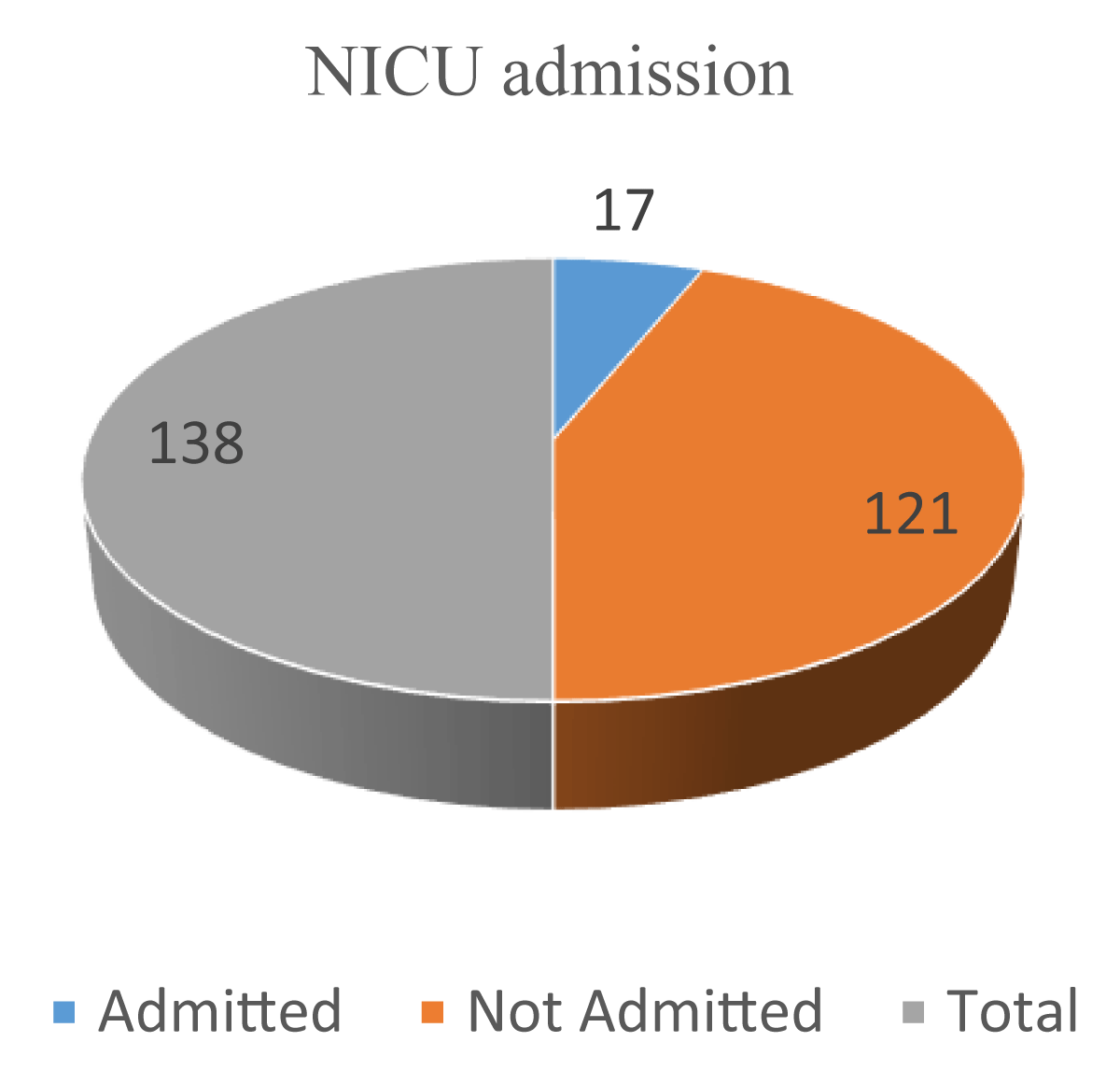
Neonatal death was 3%. Approximately 18 neonates were admitted to the Neonatal Intensive care unit (NICU) and only five of them were admitted for more than one week.
Conclusion: Postdate pregnancy prevalence in this study was 5%, which was associated with maternal risk of cesarean section delivery, instrumental delivery, postpartum hemorrhage, and postnatal infection.
Any pregnancy that has passed beyond the estimated date of delivery is called a postdated pregnancy. However, when pregnancy is prolonged beyond 42 weeks, it is called post-maturity or post-term pregnancy [1]. The incidence of prolonged pregnancy is 3% - 14% in all pregnancies [2]. Adverse perinatal outcomes gradually increase after 40 gestational weeks and substantially increase post-term (≥ 42 weeks (≥ 294 days)). The risk of stillbirth has been shown to increase after term. Worldwide, as much as 14% of stillbirths are associated with prolonged pregnancy [3].
Postdate pregnancies are associated with an increased incidence of pregnancy complications, particularly perinatal mortality, which includes stillbirths and early neonatal deaths [4]. Risk factors for postdate pregnancy include maternal obesity, prolonged pregnancy, male fetuses, and genetic disposition [5]. Although the pathophysiology of prolonged pregnancy is not well understood, the placenta itself may be involved in the expression of corticotrophin-releasing hormone (CRH) by the syncytiotrophoblast, which affects the length of gestation [6].
The management of prolonged pregnancy remains controversial, although most now accept that perinatal mortality and morbidity increase when pregnancy exceeds 42 weeks of gestation.
Decreased fetal movements (FM) may precede an abnormal fetal heart rate (FHR) or in-utero fetal death by a few days or weeks [7-9], but pregnant women are poorly Informed about what to do when they experience it, and some encounter a significant delay in accessing care or do not even contact healthcare [10-12]. Fetal movement monitoring may be an interesting way to improve neonatal outcomes [13]. Perinatal morbidity has also been noted to be higher in post-term pregnancies, including meconium and meconium aspiration syndrome [14], macrosomia [15,16], fetal birth injury, [17] rate of non-reassuring fetal heart rate or fetal distress in labor, [18] and cesarean delivery rates.
Maternal complications of labor and delivery increased in post-date women with third- or fourth-degree perineal lacerations. Postpartum hemorrhage, chorioamnionitis, and prolonged labor were all increased among women delivered at 40 weeks compared to 39 weeks of gestation. Different induction procedures are used for post-dated pregnancies by institution or area of practice. The World Health Organization and Royal College of Obstetricians and Gynecologists advise labor induction at or after 41 weeks [19,20].
The approach in our hospital units is to induce labor at 40 weeks and 10 days. Irrespective of the practice, the target was to deliver the women before 42 weeks. Expectant management and fetal surveillance are also acceptable for women who decline active management [19]. Compared with term pregnancies, post-date pregnancies had greater rates of intervention and more maternal and fetal problems. 25% of women underwent cesarean sections, while only 1.1% underwent successful vaginal deliveries. Failure to progress during labor was the most common cause of cesarean section [21].
This descriptive cross-sectional, hospital-based study was conducted at the Omdurman Maternity Hospital between January 2018 and June 2018.
The Study population included all postdate (40 weeks +1 day and more) pregnant women who presented in labor to the out patients or labor room and agreed to participate in the study. The inclusion criteria were gestational age (40 weeks+1 day completed and - 42 weeks completed and more), regular menstrual cycles, known last menstrual period, and single ton pregnancy with vertex presentation. The study excluded pregnant women with associated complications, such as previous lower segment caesarean section (LSCS), congenital anomaly, malpresentation, antepartum hemorrhage, and pregnancy-induced hypertension.
About 138 postdate women who presented in labor to the outpatients or labor room agreed to participate in the study and delivered in the hospital. Data were collected through direct interviews, using a well-structured questionnaire. The participants were interviewed about age, residence, education, booking status, previous prolonged pregnancy, gravity, gestational age, mode of delivery, maternal complications (postpartum hemorrhage, postpartum infection, cervical tear, and perineal tear), and fetal complications (shoulder dystocia, asphyxia, and meconium aspiration).
Statistical analysis was performed using SPSS software (SPSS, Chicago, IL, USA). Continuous variables were compared using Student’s t - test (for paired data) or Mann–Whitney U test for nonparametric data. For categorical data, a comparison was performed using the chi-square test (χ2) or Fisher’s exact test, when appropriate. Statistical significance was set at p < 0.05.
Ethical considerations were taken from the Sudan Medical Specialization Board, which was presented to the ethics review committee (EDC) and approved. Permission to conduct the study was requested from the authorities of health care in Omdurman Maternity Hospital. Data were handled with a high degree of confidentiality throughout the study, and written informed consent was obtained from all participants in the study.
During the study period, 2751 women delivered, of which 138 were postdated deliveries; thus, the prevalence of postdated pregnancy was 5%. Most postdate women age range 31-34 years 48.6%. Their education level was mostly secondary school 42%. Primigravida 65%, multipara 26%, and grandmultipra 9%. Most women were homemakers (52%). Table 1.
| Table 1: Sociodemographic distribution of postdate women (n = 138). | ||||
| Sociodemographic | Frequency | Percent | Mean | Std. Deviation |
| Age | ||||
| 20 | 7 | 5.1 | ||
| 20-25 | 18 | 13.0 | ||
| 26-30 | 32 | 23.2 | ||
| 31-35 | 67 | 48.6 | 3.4565 | 1.01175 |
| More 35 | 14 | 10.1 | ||
| Residence | ||||
| Inside Khartoum | 132 | 95.7 | 1.0435 | .20467 |
| Outside Khartoum | 6 | 4.3 | ||
| Education | ||||
| ` illiterate | 23 | 16.7 | ||
| Primary school | 33 | 23.9 | ||
| Secondary school | 58 | 42.0 | 2.6014 | .96311 |
| Graduated | 24 | 17.4 | ||
| Booking status | ||||
| Booked | 104 | 75.4 | 1.2464 | .43247 |
| Unbooked | 34 | 24.6 | ||
| Previous prolonged pregnancy | ||||
| Yes | 47 | 34.1 | ||
| No | 91 | 65.9 | 1.6594 | .47563 |
| Gravity | ||||
| Primigravida | 90 | 65.2 | 1.4348 | .65017 |
| Multipara | 36 | 26.1 | ||
| Grandmultipra | 12 | 8.7 | ||
| Total | 138 | 100.0 | ||
Postdate pregnant women booked were booked 75.4% and unbooked 24.6%, Booked at gestational age 40+1-40+6 weeks were 55.8%, while unbooked 3.6%, booked at gestational 41-41+6 weeks were 16%, and unbooked was 13.7%, booked at gestational > 42 weeks were 3.6% and unbooked were 24.6%. Table 2.
| Table 2: Booking status and gestational age among postdate women (n = 138). | |||
| Gestational Age/weeks | Booking status | ||
| Booked | Unbooked | Total | |
| 40+1 -40+6 | 77 | 5 | 82 |
| 41-41+6 | 22 | 19 | 41 |
| ≥42 | 5 | 10 | 15 |
| Total | 104 | 34 | 138 |
| P - value =.000; Correlation is significant at the 0.01 level | |||
Women with a previous history of postdate pregnancy were 34.1% while 65.9% not have a previous history of prolonged pregnancy, had a previous history of prolonged pregnancy at gestational age 40+1 -40+6 weeks were 27.5%, while not had prolonged pregnancy history 31.9%, had a previous history of prolonged pregnancy at gestational 41-41+6 weeks was 2.2%, while not had prolonged pregnancy history 27.5%, had a previous history of prolonged pregnancy at gestational > 42 weeks were 4.3% not had prolonged pregnancy history 27.5%, had a previous history of prolonged pregnancy at gestational were 6.5%. Table 3. The total number of normal vaginal delivery was 79 .7%, cesarean section was 14.5%, and instrumental delivery was 5.8%. At gestational age, 40+1 -40+6 weeks vaginal delivery was 54.3%, cesarean section 4.3%, instrumental delivery 0.7%, at gestational 41-41+6 weeks vaginal delivery was 23.2%, cesarean section 3.6%, instrumental delivery 2.9%at gestational > 42 weeks vaginal delivery was 2.2%, cesarean section 14.5%, instrumental delivery 2.2%, Table 4. Cesarean section indications were cervical dystocia (14.4%), cephalopelvic disproportion (9.5%), meconium-stained liquor with fetal distress (33.3%), pathological CTC (19%), and failure to progress (23.8%).
| Table 3: History of prolonged pregnancy and gestational age among postdate women (n = 138). | |||
| Gestational Age/weeks | History of prolonged pregnancy | ||
| ` Had Prolonged Pregnancy | Not had prolonged pregnancy | Total | |
| 40+1 -40+6 | 38 | 44 | 82 |
| 41-41+6 | 3 | 38 | 41 |
| ≥ 42 | 6 | 9 | 15 |
| Total | 47 | 91 | 138 |
| p - value =.01; Correlation is significant at the 0.01 level | |||
Maternal complications were present in 11% of women, PPH was found in 7.2%, perineal tear was present in .7% cervical tear was found in 1.4% and postpartum infection was 1.4%. At gestational age 40+1 -40+6 weeks 52.9% had no complications, 4.3% postpartum hemorrhage, 0.7% postnatal infection, 0.7% cervical tear, and 0.7% perineal trauma, at gestational 41-41+6 weeks 27.5% had no complications, 0.7% postpartum hemorrhage, 0.7% postnatal infection, 0.7% cevical tear, at gestational > 42 weeks had no complications 8.6%, 2.2%postpartum hemorrhage, no postnatal infection, 0no cervical tear and no perineal trauma. Table 5.
| Table 4: Mode of delivery and gestational age among postdate women (n = 138). | ||||
| Gestational Age/weeks | Mode of delivery | |||
| Vaginal delivery | Cesarean section | Instrumental delivery | Total | |
| 40+1 -40+6 | 75 | 6 | 1 | 82 |
| 41-41+6 | 32 | 5 | 4 | 41 |
| ≥ 42 | 3 | 9 | 3 | 15 |
| Total | 110 | 20 | 8 | 138 |
| p - value =.01; Correlation is significant at the 0.05 level | ||||
Fetal complications were found in twenty of the study women 14.5%), Shoulder Dystocia (2.9%), asphyxia (6.5%), and meconium aspiration (5.1%). At gestational age 40+1 -40+6 weeks 1.4% had shoulder dystocia, 2.2% asphyxia, 2.9% meconium aspiration, and 52.9% had no complications, at gestational 41-41+6 weeks 0.7% had shoulder dystocia, 1.4% asphyxia, 1.4% meconium aspiration, and 26.1% had no complications at gestational, at gestational > 42 weeks 0.7% had shoulder dystocia, 2.9% asphyxia, 0.7% meconium aspiration, and 6.5% had no complications at gestational. Table 6.
| Table 5: Maternal complications and gestational age among postdate women (n = 138). | ||||||
| Gestational Age/weeks | Maternal complications | |||||
| Perineal trauma | Cervical tear1 | Postpartum hemorrhage | Postpartum infection | No complication | Total | |
| 40+1 -40+6 | 1 | 1 | 6 | 1 | 73 | 82 |
| 41-41+6 | 0 | 1 | 1 | 1 | 38 | 41 |
| ≥ 42 | 0 | 0 | 3 | 0 | 12 | 15 |
| Total | 1 | 2 | 10 | 2 | 123 | 138 |
| p - value =.003; Correlation is significant at the 0.01 level | ||||||
| Table 6: Fetal complication and gestational age among postdate women (n = 138). | |||||
| Gestational Age/weeks | Fetal complications | ||||
| Shoulder Dystocia | Asphyxia | Meconium aspiration | No complication | Total | |
| 40+1 -40+6 | 2 | 3 | 4 | 73 | 82 |
| 41-41+6 | 1 | 2 | 2 | 36 | 41 |
| ≥ 42 | 1 | 4 | 1 | 9 | 15 |
| Total | 4 | 9 | 7 | 118 | 138 |
| p - value =.03; Correlation is significant at the 0.05 level | |||||
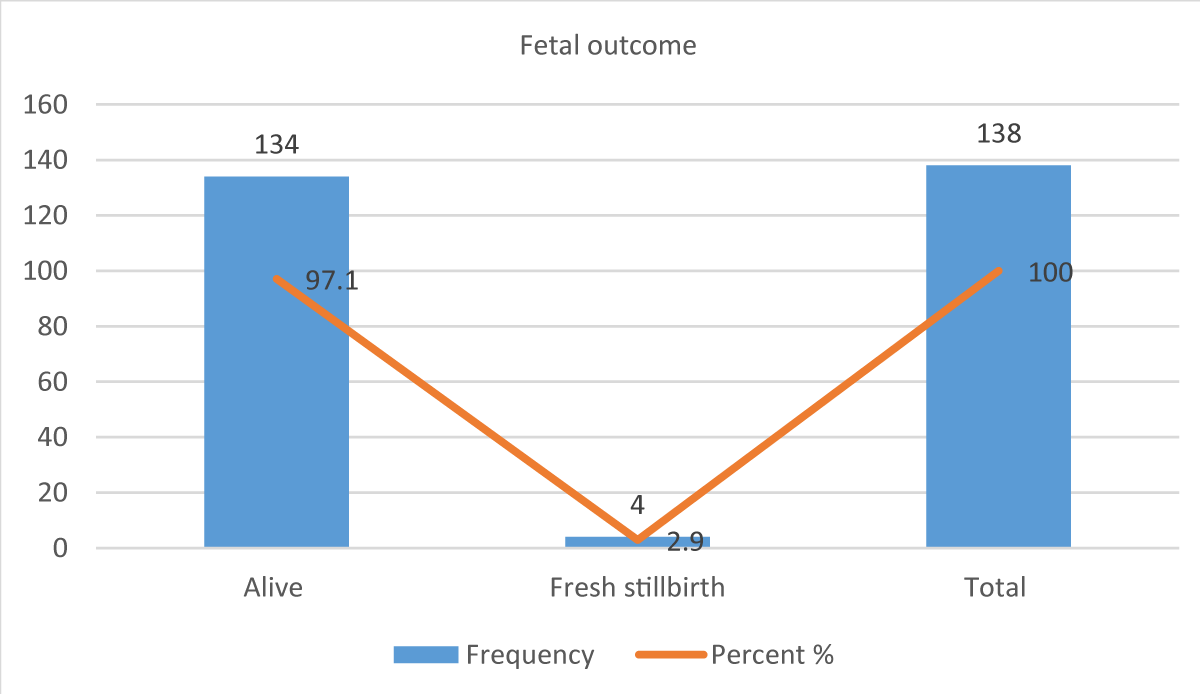
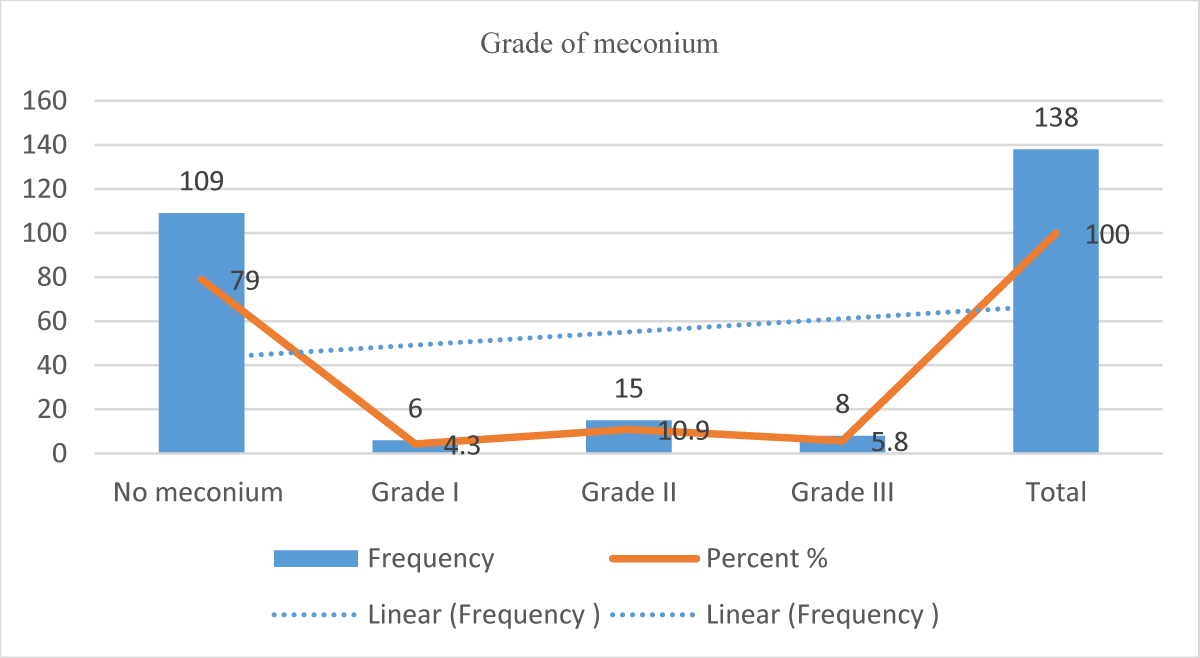
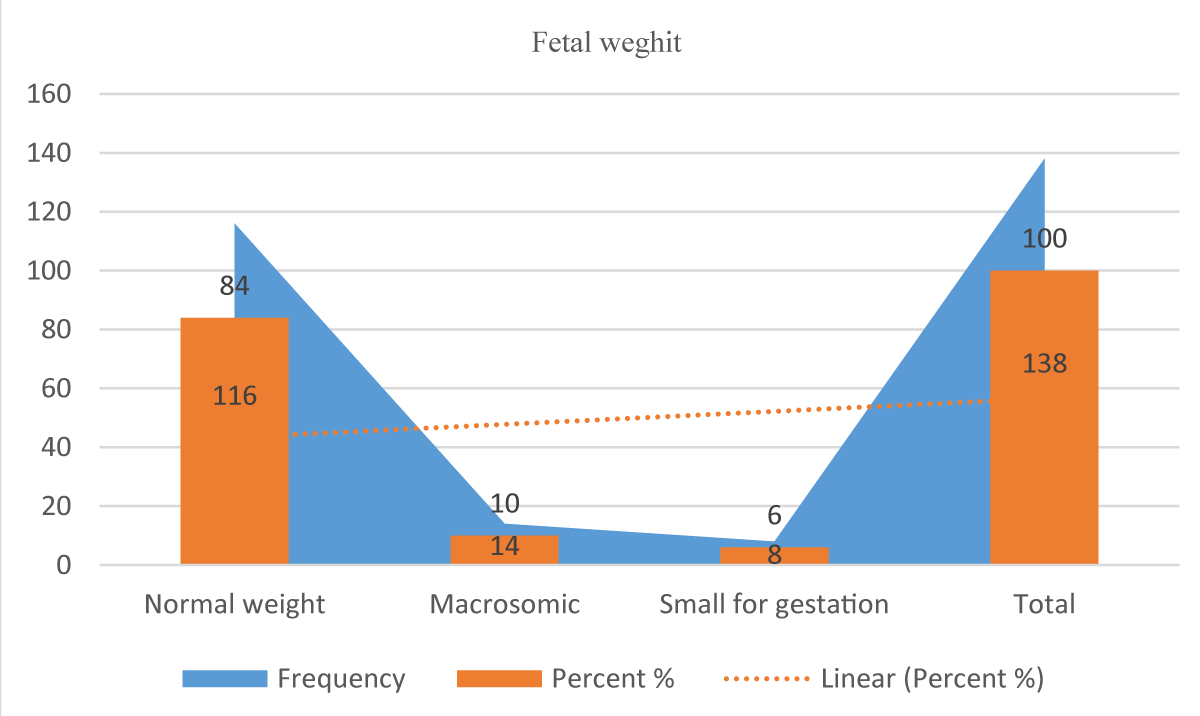
The fetal outcome is 97.1% alive while 2.9% fresh stillbirth Figure 1, Grad of meconium, grade I meconium in 4.3%, grade II in 10.9%, and grade III 5.8%. Figure 2 Feta weight, normal fetal weight 2.5 kg -3.7 kg was 84%, macrosomia fetal weight 4 kg and more in 10% and small for gestational age less than 2.5 kg were 6%. Figure 3. APGAR ASCORE less than 7 was 13% and > 7 was 87%, the mean APGAR score was 1.1667, less than three in only 3.6%, and > 7 in 86.9%, Figure 4. In NICU admission 12.3% were admitted and 87.7% were not admitted only five were admitted for more than a week. Figure 5.
Figure 1: APGAR SCORE of postdate women fetuses.
Figure 2: Fetal NICU admission among postdate women (n = 138).
Figure 3: Fetal outcome of postdate women (n = 138).
Figure 4: Grade of Meconium among postdate women (n = 138).
Figure 5: Fetal weight of postdate women.
Figure 5: Fibrohyalinized tissue with lymphangiectasis.
Postdated pregnancy is a high-risk pregnancy associated with increased maternal morbidity, fetal and neonatal morbidity, and mortality, and this study was conducted at the Omdurman Maternity Hospital to assess maternal and fetal outcomes of postdated women. The study included 138 women, and the total number of deliveries during the study period was 2751 so the prevalence of postdates was 5%, which is similar to the study by Singh, et al. [22].
Most of the postdate women's age range 31-34 years 48.6% and this reproductive age of our population which different from another study Akhtar P, et al. [23] observed in their study on pregnancy beyond 41 weeks of gestation that 82% of cases were in the age group of 18 to 29 years. In addition, Alrubaee, et al. [24] found that the majority of women were aged between (18 and 30 years) of age; (62.4% and 56.3%, respectively). The educational level is a secondary school in 42% of postdate women, which indicates a reverse relation in contrast to [25] and had primary education (57%).
Primigravida among postdate women was 65%, which is comparable with another study by Mahapatra, et al. who found that a maximum (of 72%) of patients were primigravida [26,27] and contrast with [28], which found multigravida 51.2%, while primigravida was (48.7%).
Postdate pregnant women booked were 75.4%, and women with a previous history of postdate pregnancy were 34.1%. In this study women presented between 40+1 to 40+6 weeks of gestation age were 59.4%, in between 41-41+6 weeks of gestation age were 29.7% and 10.9% were ≥ 42 weeks of gestation age. In a study conducted by Patel, et al. [29], the maximum number of patients was between 40 and 40.6 weeks which is similar to the results of this study.
The total number of normal vaginal delivery was 79.7%, cesarean section was 14.5%, and instrumental delivery was 5.8%. Shingle N, et al. [30] reported that most of the women 53.7% underwent spontaneous vaginal delivery, 9.5% of patients required instrumental delivery, and 37% of patients required cesarean section as a mode of delivery [30,31] whereas In Mahapatro’s [32] study, it was found to be 5.72% (26) and lower than [28] found 22.1%.
In the present study, the indications for cesarean section were cervical dystocia 14.4%, cephalopelvic disproportion9.5%, meconium-stained liquor with fetal distress 33.3%, pathological CTC 19%, and failure to progress 23.8%, which is comparable with and similar to Mahapatro's study [32] in which fetal distress was found to be the most common indication for cs and similar to Akhtar, et al. cesarean section was performed given fetal distress in 32% cases [23] and comparable to [33], which found that common causes of LSCS were meconium liquor post-rupture of the membrane, which accounted for 43.75%, followed by non-reassuring NST consisting of decelerations or fetal tachycardia or bradycardia, which accounted for 32.81%.
No maternal mortality was observed, but maternal complications occurred in 11% of postdate women, of which PPH was found in 7.2%, which is lower than (33), the perineal tear was present in .7% and cervical tear was found in 1.4%, and postpartum infection was 1.4% lower than [33] found 12.7% which was comparable to Neetu Singh, et al. study [22], which found most common 6% complication was postpartum hemorrhage, others were perineal tears in 5%, cervical tears in 2% of cases.
Fetal complications were found in twenty of the study women (14.5%), Shoulder Dystocia (2.9%), macrosomia asphyxia was nine cases at 6.5% which is lower than [34] found at 13.4%, and meconium aspiration (5.1%).
Fetal outcomes with an APGAR score of more than 7 was 86.9%, less than three in only 3.6%, and neonatal death was 3% which is lower than Akhter S and Thakur, et al. [23], 5.4%, and similar to [35,36] the neonatal death was because of meconium aspiration syndrome which is higher too [37] the five minutes APGAR scores the majority (70%) of the sample group APGAR score was between 7-10.
About 17 neonates were admitted to the NICU only five of them were admitted for more than one week which is higher than [33-37] and NICU admissions of 7.44%.
Fetal weight was measured by ultrasound scan and clinically, fetal macrosomia was present in 14 cases, contributing to 10% of postdate women, which was lower than previous studies, which showed about 14% and 25.7%, respectively [38,39] and similar to [34,40-41]. There was a higher incidence of cesarean section due to arrest and protraction disorders in postdate pregnancies in which the infant was macrosomic.
Study strengths and limitations
One of the strengths of the study is that women’s information was collected by deputy obstetrician-gynecologist registrars who administer the treatment, which had a positive impact on the inclusion of patients. The hospital is a referral hospital so it is easy to find women who meet the criteria, which makes the study possible; in addition, the study population characteristics can be generalized to Sudan and countermeasures can be developed with similar characteristics.
One of the limitations of the study is that it was conducted in one hospital; therefore, it cannot be compared, and the type of induction was not included to determine the effect of induction of labor on postdate pregnancy.
Postdate pregnancy is associated with an increased fetal risk of morbidity and mortality, neonatal risk of morbidity, NICU admission, and mortality, and increased maternal risk of operative delivery, instrumental delivery, postpartum hemorrhage, and postpartum infection. Early detection and diagnosis with an early ultrasound scan and proper pregnancy and labor management will optimize maternal and fetal outcomes; therefore, booking an early pregnancy ultrasound will reduce the risk of postdates, and any pregnancy that goes beyond 40 weeks of confirmed gestational age fetal well-being must be assessed.
Recommendations
Increasing the awareness of mothers about the importance of antenatal (ANC) and early booking to avoid postdated pregnancy and post-term pregnancy will reduce adverse maternal and fetal outcomes. Adequate provision of a local protocol for postdate pregnancy management and induction of labor by licensed prostaglandin drugs. Fetal surveillance in the third trimester with advanced ultrasound and cardiotocography (CTG) should be introduced in practice.
Cervical sweeping should be practiced among postdate pregnancy and women with a previous history of postdate pregnancy. Further study on the induction of labor among prolonged pregnancy and auditing prenatal mortality of prolonged pregnancy.
The author would like to express his sincere thanks and gratitude to Prof: Mandour Mohamed Ibrahim Mohamed for his helpful suggestions, continuous support, guidance, advice, and assistance during this study, as well as to the respondents for their participation in this study.
Consent: All participants were consented
Approval: Ethical clearance and the supportive letter were obtained from the Sudan Medical Specialization Board (SMSB) & Educational Development Center (EDC).
Written permission was obtained from Omdurman Maternity Hospital.
Author contribution: All authors contributed to the manuscript writing.
Data sharing: The authors agreed to the data sharing policy of this journal which applies to the HSPI publisher group.
- Hauth JC, Goodman MT, Gilstrap LC 3rd, Gilstrap JE. Post-term pregnancy. I. Obstet Gynecol. 1980 Oct;56(4):467-70. PMID: 7422191.
- Savitz DA, Terry JW Jr, Dole N, Thorp JM Jr, Siega-Riz AM, Herring AH. Comparison of pregnancy dating by last menstrual period, ultrasound scanning, and their combination. Am J Obstet Gynecol. 2002 Dec;187(6):1660-6. doi: 10.1067/mob.2002.127601. PMID: 12501080.
- Wennerholm UB, Saltvedt S, Wessberg A, Alkmark M, Bergh C, Wendel SB, Fadl H, Jonsson M, Ladfors L, Sengpiel V, Wesström J, Wennergren G, Wikström AK, Elden H, Stephansson O, Hagberg H. Induction of labour at 41 weeks versus expectant management and induction of labour at 42 weeks (SWEdish Post-term Induction Study, SWEPIS): multicentre, open label, randomised, superiority trial. BMJ. 2019 Nov 20;367:l6131. doi: 10.1136/bmj.l6131. Erratum in: BMJ. 2021 Dec 15;375:n3072. PMID: 31748223; PMCID: PMC6939660.
- Carroll A, Lee S, Desforges M, Heazell A. A review of the evidence for placental aging in prolonged pregnancy. Medical Research Archives. 2020; 8(8). https://doi.org/10.18103/mra.v8i8.2188.
- Galal M, Symonds I, Murray H, Petraglia F, Smith R. Postterm pregnancy. Facts Views Vis Obgyn. 2012;4(3):175-87. PMID: 24753906; PMCID: PMC3991404.
- Dunn-Fletcher CE, Muglia LM, Pavlicev M, Wolf G, Sun MA, Hu YC, Huffman E, Tumukuntala S, Thiele K, Mukherjee A, Zoubovsky S, Zhang X, Swaggart KA, Lamm KYB, Jones H, Macfarlan TS, Muglia LJ. Anthropoid primate-specific retroviral element THE1B controls expression of CRH in placenta and alters gestation length. PLoS Biol. 2018 Sep 19;16(9):e2006337. doi: 10.1371/journal.pbio.2006337. PMID: 30231016; PMCID: PMC6166974.
- Linde A, Georgsson S, Pettersson K, Holmström S, Norberg E, Rådestad I. Fetal movement in late pregnancy - a content analysis of women's experiences of how their unborn baby moved less or differently. BMC Pregnancy Childbirth. 2016 Jun 1;16(1):127. doi: 10.1186/s12884-016-0922-z. PMID: 27245990; PMCID: PMC4888620.
- Warland J, O'Brien LM, Heazell AE, Mitchell EA; STARS Consortium. An international internet survey of the experiences of 1,714 mothers with a late stillbirth: the STARS cohort study. BMC Pregnancy Childbirth. 2015 Aug 15;15:172. doi: 10.1186/s12884-015-0602-4. PMID: 26276347; PMCID: PMC4537542.
- Heazell A. The role of maternal awareness of reduced fetal movements to reduce perinatal mortality remains unclear. BJOG. 2020 Jun;127(7):838. doi: 10.1111/1471-0528.16173. Epub 2020 Mar 9. PMID: 32061004.
- Sergent F, Lefèvre A, Verspyck E, Marpeau L. Diminution des mouvements actifs du foetus au troisième trimestre: que faire? [Decreased fetal movements in the third trimester: what to do?]. Gynecol Obstet Fertil. 2005 Nov;33(11):861-9. French. doi: 10.1016/j.gyobfe.2005.07.041. Epub 2005 Oct 21. PMID: 16243568.
- Chauveau L, Raia-Barjat T, Noblot E, Fanget C, Gallot D, Chaleur C. Évaluation des connaissances des femmes enceintes sur les mouvements actifs fœtaux lors de la visite de terme [Maternal knowledge of fetal movements in late pregnancy]. J Gynecol Obstet Biol Reprod (Paris). 2016 Apr;45(4):360-5. French. doi: 10.1016/j.jgyn.2015.06.006. Epub 2015 Jun 27. PMID: 26123016.
- Linde A, Rådestad I, Pettersson K, Hagelberg L, Georgsson S. "Better safe than sorry"-Reasons for consulting care due to decreased fetal movements. Women Birth. 2017 Oct;30(5):376-381. doi: 10.1016/j.wombi.2017.02.007. Epub 2017 Mar 27. PMID: 28359754.
- Moniod L, Hovine A, Trombert B, Rancon F, Zufferey P, Chauveau L, Chauleur C, Raia-Barjat T. Fetal Movement Counting in Prolonged Pregnancies: The COMPTAMAF Prospective Randomized Trial. Healthcare (Basel). 2022 Dec 18;10(12):2569. doi: 10.3390/healthcare10122569. PMID: 36554092; PMCID: PMC9778956.
- Usher RH, Boyd ME, McLean FH, Kramer MS. Assessment of fetal risk in postdate pregnancies. Am J Obstet Gynecol. 1988 Feb;158(2):259-64. doi: 10.1016/0002-9378(88)90134-2. PMID: 3341404.
- McLean FH, Boyd ME, Usher RH, Kramer MS. Postterm infants: too big or too small? Am J Obstet Gynecol. 1991 Feb;164(2):619-24. doi: 10.1016/s0002-9378(11)80035-9. PMID: 1992713.
- Arias F. Predictability of complications associated with prolongation of pregnancy. Obstet Gynecol. 1987 Jul;70(1):101-6. PMID: 3299174.
- Campbell MK, Ostbye T, Irgens LM. Post-term birth: risk factors and outcomes in a 10-year cohort of Norwegian births. Obstet Gynecol. 1997 Apr;89(4):543-8. doi: 10.1016/s0029-7844(97)00049-5. PMID: 9083310.
- Boyd ME, Usher RH, McLean FH, Kramer MS. Obstetric consequences of postmaturity. Am J Obstet Gynecol. 1988 Feb;158(2):334-8. doi: 10.1016/0002-9378(88)90150-0. PMID: 3277431.
- RCOG Evidence-Based Clinical Guidelines Induction of Labour, www.researchgate.net/publication/266045914_RCOG_Evidence-based_Clinical_Guidelines_Induction_of_labour.
- Who Recommendations on Induction of Labour, at or beyond Term. World Health Organization, World Health Organization, www.who.int/publications-detail-redirect/9789240052796.
- Onyebuchi A, Okafor L, Mamah J, Obi V, Esike C, Umeora O, Out C. International Journal of Women’s Health and Reproduction Sciences. 2023; 11: 33–36.
- Neetu S. Postdated pregnancy: Its maternal and fetal outcome. International Journal of Reproduction, Contraception, Obstetrics and Gynecology. 2020; 9: 3223. https://doi.org/10.18203/2320-1770.ijrcog20203299.
- Parul A. Maternal outcome of prolonged pregnancy. Journal of Bangladesh College of Physicians and Surgeons. 2015; 32:66-70, https://doi.org/10.3329/jbcps.v32i2.26033.
- Methal AA. Postdate Pregnancy: Maternal & Neonatal Outcome. The Medical Journal of Basrah University, University of Basrah, 30 June 2022. mjbu.uobasrah.edu.iq/article_176735.html.
- Tarimo CS, Mahande MJ, Obure J. Prevalence and risk factors for caesarean delivery following labor induction at a tertiary hospital in North Tanzania: a retrospective cohort study (2000-2015). BMC Pregnancy Childbirth. 2020 Mar 18;20(1):173. doi: 10.1186/s12884-020-02861-8. PMID: 32188409; PMCID: PMC7079438.
- Mahapatro A, Samal S. Feto maternal outcome in pregnancy beyond 40 weeks. Int J Pharma Bio Sci. 2015; 6(2):53-8.
- Kilby MD. To induce or not to induce? the management of a pregnancy near ‘post-term.’ Current Obstetrics & Gynaecology. 1994; 4(2): 85–89. https://doi.org/10.1016/0957-5847(94)90021-3
- Shivani S, Hemprobba G, Urvashi V, Gunjan Y. The study of maternal and perinatal outcomes in prolonged pregnancy. Int Report contracept Obstet Gyenecol. 2017; 6(3): 1067-1070.
- Pransukhbhai PY, Londhe P. Study of maternal and fetal outcome in postdate pregnancy in Tertiary Care Hospital. International Journal of Reproduction, Contraception, Obstetrics and Gynecology. 2020; 9(9):3585. https://doi.org/10.18203/2320-1770.ijrcog20203556.
- Smith ER, Oakley E, Grandner GW, Ferguson K, Farooq F, et al. Adverse maternal, fetal, and newborn outcomes among pregnant women with SARS-CoV-2 infection: an individual participant data meta-analysis. BMJ Glob Health. 2023 Jan;8(1):e009495. doi: 10.1136/bmjgh-2022-009495. PMID: 36646475; PMCID: PMC9895919.
- Caughey AB, Washington AE, Laros RK Jr. Neonatal complications of term pregnancy: rates by gestational age increase in a continuous, not threshold, fashion. Am J Obstet Gynecol. 2005 Jan;192(1):185-90. doi: 10.1016/j.ajog.2004.06.068. PMID: 15672023.
- Mahapatro A, Samal S. Feto maternal outcome in pregnancy beyond 40 weeks. Int J Pharma Bio Sci. 2015; 6(2):53-8.
- Nair PP, Jungari ML, Tiwari MR, Butola LK. Study of induction of labor with oral misoprostol and its maternal and perinatal outcome. International Journal of Current Research and Review. 2020; 77–81. https://doi.org/10.31782/ijcrr.2020.7781.
- Nofiasari T, Utami FS. Characteristics of Child Birthing Women and Fetal Outcome in Postdate Pregnancy. Advances in Social Science, Education, and Humanities Research. 2019; 436: 671-674.
- Agrawal M, Bhriegu R, Hariharan C. Assessment of maternal and perinatal outcome in postdated pregnancy. Journal of Datta Meghe Institute of Medical Sciences University. 2017; 12(1): 35. https://doi.org/10.4103/jdmimsu.jdmimsu_20_17 .
- Caughey AB, Washington AE, Laros RK Jr. Neonatal complications of term pregnancy: rates by gestational age increase in a continuous, not threshold, fashion. Am J Obstet Gynecol. 2005 Jan;192(1):185-90. doi: 10.1016/j.ajog.2004.06.068. PMID: 15672023.
- Mohammed AK. The relationship between some variables with birth outcome among postdate pregnant women delivering at Maternity Teaching Hospital Sulaymaniyah City, Iraq. Journal of Zankoy Sulaimani - Part A. 2020; 22(1): 389–398. https://doi.org/10.17656/jzs.10800.
- Kuller JA, Katz VL, McMahon MJ, Wells SR, Bashford RA. Pharmacologic treatment of psychiatric disease in pregnancy and lactation: fetal and neonatal effects. Obstet Gynecol. 1996 May;87(5 Pt 1):789-94. doi: 10.1016/0029-7844(95)00476-9. PMID: 8677088.
- Kuznetsova IV, Konovalov VA. Use of folic acid during pregravid preparation and pregnancy. Russian Bulletin of Obstetrician-Gynecologist. 2015; 15(1): 24. https://doi.org/10.17116/rosakush201515124-31.
- Indonesian Ministry of Health. 2016 National Health Indicator Survey Report. Indonesian Ministry of Health, Jakarta, 2017.
- Morken NH, Klungsøyr K, Skjaerven R. Perinatal mortality by gestational week and size at birth in singleton pregnancies at and beyond term: a nationwide population-based cohort study. BMC Pregnancy Childbirth. 2014 May 22;14:172. doi: 10.1186/1471-2393-14-172. PMID: 24885576; PMCID: PMC4037279.