More Information
Submitted: August 31, 2023 | Approved: September 09, 2023 | Published: September 11, 2023
How to cite this article: Hammad KMA, Suliman AA, Ahmed HSI, Omer EAS, Handady SOM. Impact of Primary Cesarean Section on Grand Multiparous Women. Clin J Obstet Gynecol. 2023; 6: 126-131.
DOI: 10.29328/journal.cjog.1001140
Copyright License: © 2023 Hammad KMA, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Impact; Primary; Cesarean section; Grand multiparous; Sudanese women
Impact of Primary Cesarean Section on Grand Multiparous Women
Kabbashi Mohammed Adam Hammad1, Awadalla Abdelwahid Suliman2*, Hajar Suliman Ibrahim Ahmed2, Emad Abdalla Siddig Omer3 and Siddig Omer M Handady4
1Assistant Professor of Obstetrics and Gynecology, Faculty of Medicine, Al White Nile University, Sudan
2Assistant Professor of Obstetrics and Gynecology, Faculty of Medicine, Al Neelain University, Sudan
3Consultant of Obstetrics and Gynecology, Omdurman maternity hospital, Sudan
4Associated Professor of Obstetrical & Gynecology, Faculty of Medicine, Al Nahda University, Ibrahim Malik teaching Hospital, Sudan
5Facultyof Medicine, University of Medical Sciences and Technology, Sudan
*Address for Correspondence: Awadalla Abdelwahid Suliman, Assistant Professor of Obstetrics and Gynecology, Faculty of Medicine, Al Neelain University, Khartoum, Sudan, Email: [email protected]
Background: Grand multiparty is common obstetrical problem, in Sudan large families is desirable for cultural and religious backgrounds and higher incidence of grandmultipra is expected, the risk factors associated with adverse maternal outcomes have yet to be adequately investigated among grand multiparity need to delivered by primary cesarean section.
Objective: The main objective was to determine impact of primary cesarean section on grand multiparous, it is indications and complications.
Methodology: It was a descriptive prospective cross-sectional hospital-based study conducted at Omdurman Maternity Hospital during period October 2016 to March 2017.
An interview questionnaire was used for data collection. Demographic and clinical data concerning personal history, parity, indications of primary cesarean section, type of Cs, maternal complication and neonatal complications were recorded. Also, multiparous less than five delivery, previous lower segment caesarean section, known medical disorders except anemia and twin pregnancy were excluded.
Results: During the study period total of 113 grand multipara included, incidence of primary cesarean section in grand multipara was 10%. Indication in our study 22.1% due to malpresentation, fetl distress 15% and prolonged first stage 13.4%, prolonged second stage 12.4% and antepartum haemorrhage 11.5%.
Postpartum haemorrhage developed in 9.7%, hysterectomy 1.8%, uterine tear 5.4% bladder injury fetal laceration 3.6%, spinal anesthesia headache 7%, post-partum pyrexia 5.3%, sepsis 4.4%, urinary tract infections were 2.7%.
Conclusion: The finding in this study showed 10% incidence of primary cesarean section in grandmultipra. The most indications of primary cesarean section in grandmultipra malpresentation, fetal distress, prolonged first and second stage of labour. Most CS were emergency.
Grandmultipra is common in Sudan, where large families are normal, primary Caesarean Section (CS) in the grand multipara means the first caesarean section done in patients who had delivered vaginally five or more. Mainly the baby and the placenta are responsible for caesarean section in grandmultipra. Caesarean section is recommended when vaginal delivery might pose a risk to the mother or baby and is also carried out for personal and social reasons.
Grandmultipra may still have cephalopelvic disproportion even having previously delivered a full-term child vaginally. Since the fetus increases in size with multiparty, the size of the fetus and fetal head should be carefully estimated. In multifarious patients, malpresentation is favored by a pendulous abdomen and lordosis of the lumbar spine, and in any case it is usual for the head not to engage in the pelvis until the onset of labour [1].
With the introduction of modern technology in the labor wards and neonatology units, there was a further rise in caesarean sections [2]. It is a common belief among the public that once a mother delivers her child or children normally, all her subsequent deliveries are normal as a result such multifarious mothers often neglect routine antenatal checkups. It is for these reasons that attention has been directed to the indication for caesarean section in women who have previously delivered vaginally.
With the introduction of modern technology in the labour wards like cardiotocography, color Doppler, and biophysical profile, there was a further increase in caesarian section rates with numerous other medical, social, economic, and medico-legal factors which are responsible for the alarmingly high rate of the caesarian section all over the world [3].
The other responsible factors for the rise in caesarian section rate in grand multipara are the identification of high-risk pregnancies with improved antenatal care and antepartum fetal surveillance techniques, rising rates of elective induction of labour, the decline in operative vaginal deliveries, and vaginal breech deliveries, increased number of women with pregnancies after 30 years with associated medical complications [4].
Caesarian Section (CS) is considered a safer alternative to prolonged and difficult vaginal operative delivery so as to reduce maternal and perinatal morbidity and mortality [5]. Since that time a number of studies have reported the role of high parity on perinatal outcome [6,7].
This was a Prospective descriptive, cross-sectional, and hospital-based study. It was conducted at Omdurman maternity hospital during the period from October 2016 to March 2017.
The Study population included all grand multipara pregnant women presented in labor to the outpatients or labor room and fulfilled study inclusion criteria and they agreed to participate in the study. The study excluded pregnant women with multiparous less than five delivery, previous Lower Segment Caesarean Section (LSCS), and known medical disorders except for anemia and twin pregnancy. About 113 grand multiparous women were included.
Sampling
Every primary CS delivery done at the hospital during the period of the study was reviewed. The sample was made up of women who met the following criteria: women in the delivery room preparing for the fifth to the ninth delivery, or patients seen during the post-partum period following the fifth to ninth delivery and delivered by primary CS.
The sample size was not estimated as we aimed to enroll all grand multiparas delivered by primary CS. We carried out a consecutive enrolment. The duration of the post-partum follow-up was two days.
Variables of the study
Data were recorded by using a self-constructed questionnaire. Information was obtained from medical records of patients and medical reports in the delivery and operating rooms. The variables of the study were:
- Socio-demographic characteristics of patients: age, occupation, educational level
- Delivery parameters: primary CS
- Maternal complications and outcomes.
- Fetal outcomes: weight, APGAR
Data was collected by direct interview by using a well-structured questionnaire. The participants were interviewed about age, education, occupation, gestational age at delivery, parity, indication of CS, type CS, intrapartum complications, postpartum complications, fetal complications, and neonatal complications.
Statistical analysis was performed via SPSS software (SPSS, Chicago, IL, USA). Continuous variables were compared using the student’s t-test (for paired data) or the Mann–Whitney U test for nonparametric data. For categorical data, a comparison was done using the Chi-square test (X2) or Fisher’s exact test when appropriate. A p - value of < 0.05 was considered statistically significant.
Ethical clearance from the ethical committee of the Sudan Medical Specialization Board, Council of Obstetrics and Gynecology was obtained. Official agreement from the general managers of Omdurman maternity has preceded the conduction of the study. Ethical consideration was taken, it was presented to the ethics review committee and approved, permission to conduct the study was requested from authorities of health care in the study area, data was handled with a high degree of confidentiality throughout the study, and written informed Consent was taken from all participants in the study.
During the study period, a total of 113 grand multiparas were included in the study, and they were delivered by primary cesarean section in the hospital, the total number of primary cesarean section deliveries was 1127 and primary cesarean section multipara was 113 (10%).
Most women aged 31 years - 35 years old 59.3%, educational level secondary school 60.2% and 72.6% were housewives.
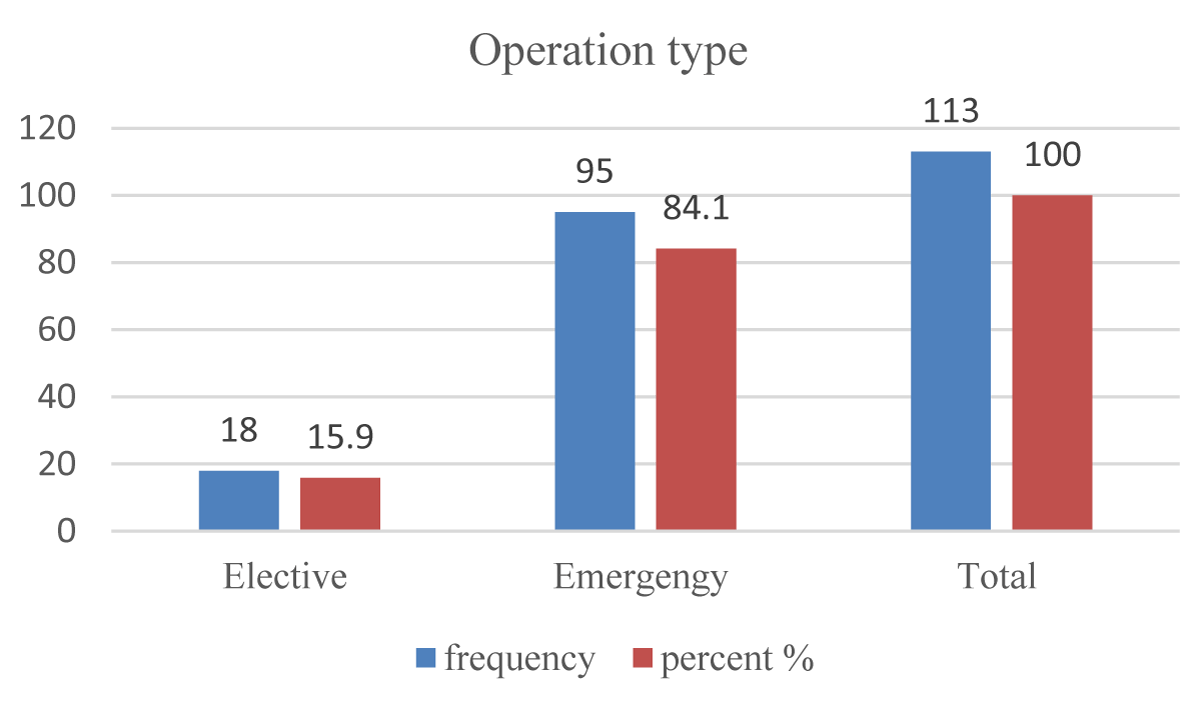
A multipara who has earlier delivered vaginally may still require a caesarean section most common indication in our study was malpresentation 22.1%, fetal distress 15% and prolonged first stage 13.4%, prolonged second stage12.4%, Antepartum Haemorrhage (APH) 11.5%, maternal request 8%, Premature Pre labour Rupture of Membranes (PPROM) 7.1%, eclampsia 6.2%, failed instrumental delivery 4.4%. In this study only 15.9% were delivered by elective CS and 84.1% were delivered by emergency CS, this study demonstrates that the majority of primary CS is most common among Para six 35.4% and Para seven 29.2% and Para nine were least 6.2% and most women underwent primary Caesarean section at 39-40 weeks were 69.9%.
An intrapartum complication noted during surgery was one case of bladder injury, four cases of fetal laceration, six cases of uterine tear, and two women developed massive postpartum hemorrhage not controlled by medical treatment that required a hysterectomy to save a woman's life and Postpartum Haemorrhage (PHH) developed in 9.7%.
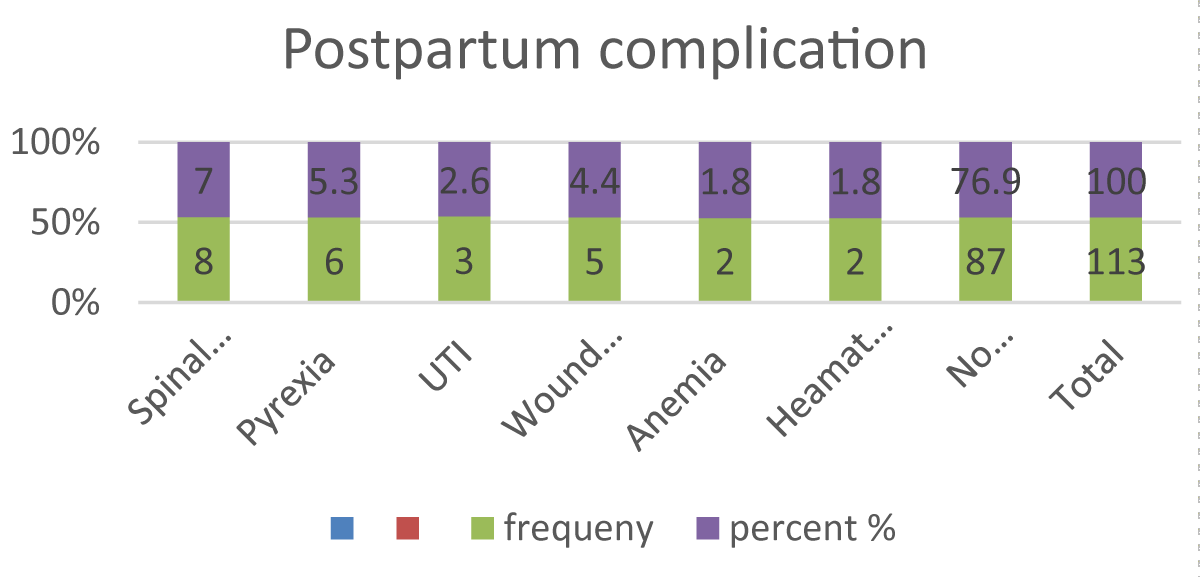
This study of post-operative maternal complication found that 77% had no complication or morbidity, the percentage is higher in post-spinal anesthesia headache at 7%, post-partum pyrexia at 5.3%, sepsis at 4.4%, Urinary Tract Infection (UTI) 2.7%, had anemia 1.8%, hematoma 1.8%, no one had endometritis, no had deep venous thrombosis.
In this study fetal outcome was good most babies delivered of birth weight, 2.5-2.999 kg were 46%, and the macrosomic baby was 4.5 kg and more were 7% which may reflect a failure to progress in labor and the need for emergency CS, 5 Minute Apgar Score was 88 (77.8%), 5Minute Apgar Score zero in only two cases 1.8%, those distressed babies were attended by a pediatrician and admitted to NICU only .9% admitted for more than 7 days, 4.4% need 1 - 3 days admission, In our study we did not have any maternal mortality (Figures 1-3) (Tables 1-3).
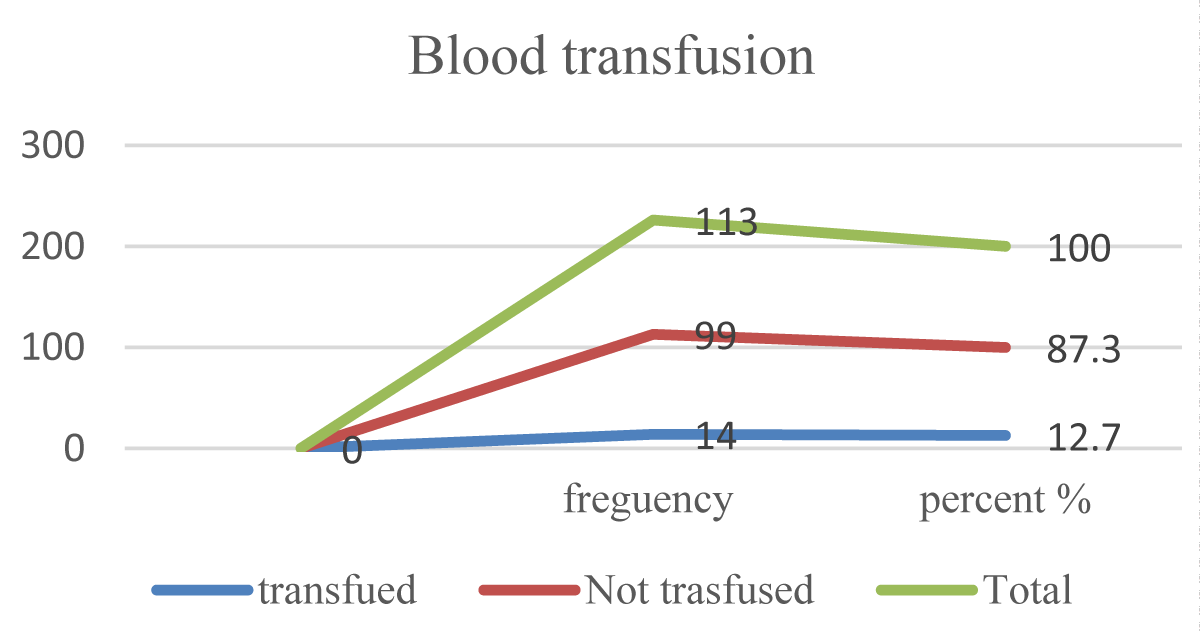
Figure 1: Blood transfusion in Primary Cs GM (n = 113).
Figure 2: Postpartum complications in primary CS GM (n = 113).
Figure 3: Operation type in primary CS GM (n = 113).
| Table 1: Sociodemographic of primary Cs in grand multiparous (n = 113). | ||
| Age | Frequency | Percent% |
| 20 - 25 | 3 | 2.7 |
| 26 - 30 | 24 | 21.2 |
| 31 - 35 | 67 | 59.3 |
| 36 - 40 | 14 | 12.4 |
| >40 | 5 | 4.4 |
| Total | 113 | 100 |
| Educational | ||
| illiterate | 9 | 8 |
| Primary | 25 | 22.1 |
| Secondary | 68 | 60.2 |
| Graduated | 11 | 9.7 |
| Total | 113 | 100 |
| Occupation | ||
| Housewife | 82 | 72.6 |
| Worker | 19 | 16.8 |
| Employer | 12 | 10.6 |
| Total | 113 | 100 |
| Table 2: Indications of primary Cs in Grand multiparous (n = 113). | |||||
| Indication of cs | Frequency | Percent% | Mean | Std. Deviation | p - value |
| Fetal distress | 17 | 15.0 | 1.8496 | .35910 | .002 |
| APH | 13 | 11.5 | 1.8850 | .32050 | .028 |
| Malpresentation | 25 | 22.1 | 1.7788 | .41693 | .00 |
| PPROM | 8 | 7.1 | 1.9292 | .25763 | .030 |
| Prolonged 1st stage | 16 | 14.2 | 1.8584 | .35019 | .060 |
| Prolonged 2nd stage | 14 | 12.4 | 1.8584 | .35019 | .030 |
| Maternal request | 9 | 8.0 | 1.9204 | .27195 | .000 |
| Failed Instrumental | 5 | 4.4 | 1.9912 | .09407 | .021 |
| Eclampsia | 6 | 5.3 | 1.9375 | .24315 | .023 |
| Total | 113 | 100 | |||
| Table 3: Complications of primary CS in grand multiparous (n = 113). | ||
| Complications | Frequency | Percent% |
| PPH | 11 | 9.7 |
| Hysterectomy | 2 | 1.8 |
| Uterine tear | 6 | 5.4 |
| Bladder injury | 1 | .9 |
| Fetal laceration | 4 | 3.6 |
| No complication | 89 | 78.6 |
| Total | 113 | 100 |
Grand multipara who has earlier delivered vaginally may still require a caesarean section for safe delivery. During the study period total of 113 were of different risk but were grand multipara included in the study, and they were delivered by primary cesarean section in the hospital with different indications and different gestational ages.
The total number of primary cesarean section delivery were 1127 and primary cesarean section multipara were 113 (10%) which is quite less than primary caesarean in nullipara, and para1-4 but they are actually associated with high maternal and fetal morbidity which is lower to study conducted in India has shown total caesarean rates in the public, were 20% [8], comparable to study demonstrated that primary cesarean rate among grand multipara women was 13.3% as compared to 18% in nulliparous women, a study conducted in United States showed rates of 13.3% [9], and higher than the study done in Netherlands observed caesarean rates in grand multiparous women 5.33% [10].
Grand multiparty is a problem associated with poverty, illiteracy, ignorance, and lack of knowledge of the available antenatal care and family planning methods, who have earlier delivered vaginally may still require a caesarean section.
Indication in our study was malpresentation 22.1%, fetal distress 15% prolonged first stage 13.4%, prolonged second stage%, APH 11.5%, maternal request 8%, PPROM 7.1%, eclampsia 6.2%, failed instrumental delivery 4.4% p - value .001. which similar to other studies by Jacob & Bhargava [11,12], in another study, antepartum or intrapartum fetal distress was leading indication in 41% of women.
Electronic fetal monitoring which is commonly used to detect fetal distress is known to have poor specificity resulting in an increase in the number of cesarean sections carried out for fetal distress [9,13-15].
The breech is malpresentation associated with higher maternal mortality and morbidly irrespective of the route of delivery due to its association with fetal abnormalities and premature delivery. However, vaginal delivery for term breech does not increase morbidity and mortality, if the case for vaginal delivery is well selected but there is an increase in caesarean section for breech presentation, as most obstetricians consider it to be safer and easier than giving a trial of labor. This has led to an increase in the elective caesarean section for breech in this study. To reduce the CS rate external cephalic version should be offered and a trial of breech vaginal delivery should be advisable.
Primary CS in grand multipara due to failed progress in the first and second stages of labour was 25.8%, in the first stage of labour malposition and a sizable fetus could be explanation while in the second stage, maternal exhaustion and malposition are underline causes, it seems that the decision of caesarean section depends upon the department policy where the safety of caesarean section has encouraged the obstetricians towards caesarean section. Antepartum haemorrhage is an important cause of primary CS in grandmultipra 11.5% which is caused by placenta praevia and placental abruption, so cesarean section is life saving procedure to mother and her fetus, a definitive risk for both child and mother if any delay is done [16].
Maternal requests for CS increase the CS rate it is an issue behind which various rationales and life experiences need carefully targeted attention and health care so it should be regarded partly as an iatrogenic problem. Previous traumatic birth experiences prompted a preference for a planned cesarean to avoid a repetition of the trauma which is a necessary need for proper women's counselling.
In this study only 15.9% were delivered by elective CS and 84.1% were delivered by emergency CS, rate of emergency caesarean section is much higher than the elective caesarean section it is similar to Saxena N, et al. study [17] and Shazia Aftab, et al. [18] which might be because of the prevalence of factors such as prolonged labour or cephalo-pelvic disproportion which are diagnosed in the labour are could be the possible explanation for emergency cesarean sections instead of instrumental vaginal delivery also the reason may be due to a greater number of unbooked cases who either refer or come without any antenatal care which may lead to an emergency caesarean section or they may come in labour with complications like malpresentation, fetal distress undiagnosed placenta previa which led to emergency caesarean section. Those women delivered by elective CS were due to transverse lie, placenta praevia, breech presentation, and maternal request for CS with tubal ligation.
This study demonstrates that the majority of primary CS is most common among Para Six 35.4% Para Seven 29.2% and Para Nine were least 6.2% which similar to a study that showed most of the six parties had increased incidence of primary caesarean section in multipara its percentage in the present study is 35.4%. which is correlating with all the other studies with percentage in each study being Erika DesaI [19] 23.26%, Sethi Pruthwiraj 35%, P. Himabindhu [20] 63.9%.
In the present study, most of the women undergoing primary caesarean section in grand multipara were in the age group of (31-35) years 59.3% which is similar to other studies of Rao Jyothi H [21], J K Saluja [22], Sethi Pruthwiraj.
The maximum primary CS undergone among the age group 31 - 40 years was 71.7% which was also found in the Partha Saradhi, et al. study [23].
Most women who underwent Primary Caesarean section at 39 weeks - 40 weeks were 69.9% and 11.5% who delivered at 41 - 41 weeks most of them had no antenatal care.
Regarding post-partum hemorrhage required blood transfusion during and after Caesarean section 9.7%, of those were due to antepartum hemorrhage rather than surgical technique, those complicated by PPH had received a blood transfusion and blood products, massive PPH was seen in 2.7%, while moderate PPH in 5.3% and mild in 1.8% and found due to placenta previa and atonia which is comparable to [24].
An intrapartum complication that was noted during surgery was one case of bladder injury, four cases of fetal laceration, six cases of uterine tear, and two women developed massive postpartum hemorrhage not controlled by medical treatment that required a hysterectomy to save women's lives.
In our study of post-operative maternal late complication, 78% had no complication or morbidity, the percentage is more in post-spinal anesthesia headache at 7%, post-partum pyrexia 5.3%, sepsis 4.4%, UTI at 2.7%, had anemia 1.8%, hematoma 1.8%, no one had endometritis not had deep venous thrombosis which is comparable with another study, J.K.Saluj, but it is not compatible with two studies of Rao Jyothi H and Sethi Pruthwira [21,22] grand multiparous women had a higher risk of adverse maternal outcomes, according to our finding which is similar to [25].
The fetal outcome was good most babies delivered of birth weight, 2.5 - 2.999 kg were 46%, and the macrosomic baby was 4.5 kg and more were 7% which may reflect a failure to progress in labour and need for emergency CS, 5 Minute Apgar Score were 88 (77.8%), 5 Minute Apgar Score zero in only two cases 1.8%, those distressed babies were attended by a pediatrician and admitted to NICU only .9% admitted for more than 7 days, 4.4% needed 1 - 3 days admission.,
There were two perinatal deaths due to meconium aspiration syndrome one case of respiratory distress syndrome one case mortality rate at tertiary care hospitals is less because of good antepartum and intrapartum care Most babies delivered Alive at 98.2%, and only three were Fresh still Birth 1.8% in our study less number of still births which is accounting for 1.8% and it is less than other studies where there is more percentage of still born as in Rao Jyothi H [21] it is 7%, J.K. Saluja [22] is 12%, Sethi Pruthwiraj [20] it is 3%.
In our study, we did not have any maternal mortality Although cesarean section has a mortality rate < 1%, in many developing countries it is 10 - 20 times greater with cesarean section compared to vaginal delivery [26]. No significant difference in maternal mortality was found between elective cesarean delivery and planned vaginal delivery delivered by emergency CS [27-41].
The study concluded that primary cesarean section in grandmultipra is commonly indicated among unbooked women, done emergency rather than an elective, commonest indication of malpresentation, fetal distress prolonged first and second stage of labour, and antepartum haemorrhage. Primary cesarean section in grand multipara is associated with increased intrapartum risk of PPH, blood transfusion, uterine tear, and hysterectomy also associated with high risk of postpartum pyrexia, wound infection, UTI, anemia, and Fetal risk of NICU admission increased. There should be effective health education and free provision of effective contraception. To reduce cesarean section rate among grand multiparous instrumental delivery should be encouraged, the trial of breech delivery should be conducted, and maternal requests for CS should be studied and clarified.
- Krishnan MV, Rao BK. Caesarean deliveries- Changing Trends. In: Arulkumaran S, Ratnam SS, Bhasker Rao K, Editors. The Management of Labour, 2nd Ed. Hyderabad, Orient Longman. 2015; 351-63.
- Basak S, Lahri D. Dystocia in eutocia multigravida. J Obstet Gynae Col India. 2015; 25:502.
- Rao JH, Rampure N. Study of Primary Caesarean Section in Multiparous Women. Journal of Evolution of Medical and Dental Sciences. 2013; l2(24):4414-18.
- Desai E, Leuva H, Leuva B, Kanani M. A study of primary caesarean section in multipara. Int J Reprod Contracept Obstet Gynecol. 2013; 2(3):320-324.
- Jacob S, Bhargava H. Primary caesarean section in multipara. J Obstet Gynaecol India. 2012; 22(6):642- 50.
- Solomons B. The dangerous multipara. Lancet. 1934; 2:8-11.
- Eidelman AI, Kamar R, Schimmel MS, Bar-On E. The grandmultipara: is she still a risk? Am J Obstet Gynecol. 1988 Feb;158(2):389-92. doi: 10.1016/0002-9378(88)90161-5. PMID: 3341414.
- Sreevidya S, Sathiyasekaran BW. High caesarean rates in Madras (India): a population-based cross sectional study. BJOG. 2003 Feb;110(2):106-11. PMID: 12618152.
- Elferink-Stinkens PM, Brand R, Van Hemel OJ. Trends in caesarean section rates among high- and medium-risk pregnancies in The Netherlands 1983-1992. Eur J Obstet Gynecol Reprod Biol. 1995 Apr;59(2):159-67. doi: 10.1016/0028-2243(95)02050-3. PMID: 7657010.
- Declercq E, Menacker F, Macdorman M. Maternal risk profiles and the primary cesarean rate in the United States, 1991-2002. Am J Public Health. 2006 May;96(5):867-72. doi: 10.2105/AJPH.2004.052381. Epub 2006 Mar 29. PMID: 16571712; PMCID: PMC1470600.
- Jacob S. Hitesh Bhargava. Primary caesarean in multipara. J Obstet & Gynec India. 1972; 22(6):642-50.
- Palanichamy G. A study of 900 primary caesarean sections with special reference to 151 primary caesarean sections in grand multipara. J Obstet & Gynec India. 1976; 26:374-379.
- Goonewardene M, Manawadu MH, Priyaranjana DV. Audit: The Strategy to Reduce the Rising Caesarean Section Rates. J South Asian Feder Obst Gynae. 2012; 4(1):5-9.
- Shehata AI, Hashim TJ. Decrease in perinatal mortality and increase in cesarean section rates. Int J Gynaecol Obstet. 1995 Mar;48(3):261-7. doi: 10.1016/0020-7292(94)02282-4. PMID: 7781867.
- Guihard P, Blondel B. Trends in risk factors for caesarean sections in France between 1981 and 1995: lessons for reducing the rates in the future. BJOG. 2001 Jan;108(1):48-55. doi: 10.1111/j.1471-0528.2001.00009.x. PMID: 11213004.
- Al-Shaikh GK, Ibrahim GH, Fayed AA, Al-Mandeel H. Grand multiparity and the possible risk of adverse maternal and neonatal outcomes: a dilemma to be deciphered. BMC Pregnancy Childbirth. 2017 Sep 19;17(1):310. doi: 10.1186/s12884-017-1508-0. PMID: 28927391; PMCID: PMC5606064.
- Saxena N, Sharma B, Gupta V, Kamal S. Negi. A six-year appraisal of caesarean delivery at a teaching hospital in Uttarakhand. Int J Reprod Contracept Obstet Gynecol. 2016; 5(12):4369-72.
- Desai E, Leuva H, Leuva B, Kanani M. A study of primary caesarean section in multipara. Int J Reprod Contracept Obstet Gynecol. 2013; 320-324.
- Sethi P, Vijaylaxmi S, Shailaja G, Bodhare T, Devi S. A study of primary caesarean section in multigravidae. Perspectives in medical research. 2014; 2:37.
- Rao J, Rampure N. Study of primary caesarean section in multiparous women. jemds. 2013; 2(24):4414-4418.
- Saluja JK, Roy PK, Mahadik K. Study of primary caesarean section in multiparous women. NJIRM. 2014; 5(2).
- Reddy PSG, Ramana VS, Bhanu S. Clinical Study of Primary Caesarean Section inMultiparous Women. Indian Journal of Research. 2015; 4(10).
- Aftab S, Ali N, Saleh F, Ghafoor S. Indications of Primary Cesarean Section in Multipara JBUMDC. 2019; 9(2):105-108.
- Dasa TT, Okunlola MA, Dessie Y. Effect of grand multiparity on adverse maternal outcomes: A prospective cohort study. Front Public Health. 2022 Oct 13;10:959633. doi: 10.3389/fpubh.2022.959633. PMID: 36311606; PMCID: PMC9608575. Front. Public Health .202210: 959633.
- Baldo MH. Caesarean section in countries of the Eastern Mediterranean Region. East Mediterr Health J. 2008 Mar-Apr;14(2):470-88. PMID: 18561740.
- Carbonne B. Increase in cesarean delivery: are we facing a pandemic? Int J Gynaecol Obstet. 2009 Dec;107(3):183-4. doi: 10.1016/j.ijgo.2009.07.030. Epub 2009 Aug 27. PMID: 19716127.
- Liu S, Liston RM, Joseph KS, Heaman M, Sauve R, Kramer MS; Maternal Health Study Group of the Canadian Perinatal Surveillance System. Maternal mortality and severe morbidity associated with low-risk planned cesarean delivery versus planned vaginal delivery at term. CMAJ. 2007 Feb 13;176(4):455-60. doi: 10.1503/cmaj.060870. PMID: 17296957; PMCID: PMC1800583.
- Tadevosyan M, Ghazaryan A, Harutyunyan A, Petrosyan V, Atherly A, Hekimian K. Factors contributing to rapidly increasing rates of cesarean section in Armenia: a partially mixed concurrent quantitative-qualitative equal status study. BMC Pregnancy Childbirth. 2019 Jan 3;19(1):2. doi: 10.1186/s12884-018-2158-6. PMID: 30606147; PMCID: PMC6318900.
- Betrán AP, Temmerman M, Kingdon C, Mohiddin A, Opiyo N, Torloni MR, Zhang J, Musana O, Wanyonyi SZ, Gülmezoglu AM, Downe S. Interventions to reduce unnecessary caesarean sections in healthy women and babies. Lancet. 2018 Oct 13;392(10155):1358-1368. doi: 10.1016/S0140-6736(18)31927-5. PMID: 30322586.
- Samal R, Palai P, Ghose S. Clinical study of primary cesarean section in multiparous women in a tertiary care hospital. Int J Reprod Contracept Obstet Gynecol. 2016; 5:1506-9.
- Raudaskoski T, Gissler M. Monisynnyttäjän obstetriset erityispiirteet [Obstetric characteristics of a grand multipara]. Duodecim. 2014;130(13):1309-17. Finnish. PMID: 25095478.
- Roy R, Vernekar M. Feto-maternal outcome in grand multipara. Int J Reprod Contracept Obstet Gynecol. July 7, 2017; 6: 2846-2851.
- Khan NR, Perveen S, Begum Z, Qayyum R, Malik R. Grand multiparity and maternal outcome in absence of adequate antenatal care J Postgrad Med Inst. 2017; 31(1):67-71.
- Alhainiah MH, Abdulljabbar HSO, Bukhari YA. The Prevalence, the Fetal and Maternal Outcomes in Grand Multiparas Women. Mater Sociomed. 2018 Jun;30(2):118-120. doi: 10.5455/msm.2018.30.118-120. PMID: 30061801; PMCID: PMC6029909.
- Glodean DM, Miclea D, Popa AR. Macrosomia. A systematic review of recent literature Rom J Diabetes Nutr Metab Dis. 2018; 25(2):187-195.
- Alshammari RF, Khan FH, Alkwai HM, Alenazi F, Alshammari KF, Sogeir EKA, Batool A, Khalid AA. Role of Parity and Age in Cesarean Section Rate among Women: A Retrospective Cohort Study in Hail, Saudi Arabia. Int J Environ Res Public Health. 2023 Jan 13;20(2):1486. doi: 10.3390/ijerph20021486. PMID: 36674239; PMCID: PMC9865448.
- Antoine C, Young BK. Cesarean section one hundred years 1920-2020: the Good, the Bad and the Ugly. J Perinat Med. 2020 Sep 4;49(1):5-16. doi: 10.1515/jpm-2020-0305. PMID: 32887190.
- Betran AP, Ye J, Moller AB, Souza JP, Zhang J. Trends and projections of caesarean section rates: global and regional estimates. BMJ Glob Health. 2021 Jun;6(6):e005671. doi: 10.1136/bmjgh-2021-005671. PMID: 34130991; PMCID: PMC8208001.
- Ahmed AE, Mohammad RS. Cesarean sections. Associated factors and frequency at King Abdulaziz Medical City in the Central Region of the Kingdom of Saudi Arabia. Saudi Med J. 2018 Nov;39(11):1154-1157. doi: 10.15537/smj.2018.11.22499. PMID: 30397716; PMCID: PMC6274665.
- Martinelli KG, Gama SGND, Neto S, ETD. The role of parity in the mode of delivery in advanced maternal age women. Revista Brasileira de Saúde Materno Infantil. 2021; 21:65–75.
- Deng R, Tang X, Liu J, Gao Y, Zhong X. Cesarean delivery on maternal request and its influencing factors in Chongqing, China. BMC Pregnancy Childbirth. 2021 May 19;21(1):384. doi: 10.1186/s12884-021-03866-7. PMID: 34011289; PMCID: PMC8132350.