More Information
Submitted: July 07, 2023 | Approved: July 27, 2023 | Published: July 28, 2023
How to cite this article: Kangulu IB, Moyambe JNT, Nzaji MK, Kibibi AA, Kazadi AM, et al. Quality of Antenatal Care and its Determinants in the Urban-Rural Environment of Kamina, Democratic Republic of the Congo. Clin J Obstet Gynecol. 2023; 6: 101-107.
DOI: 10.29328/journal.cjog.1001136
Copyright License: © 2023 Kangulu IB, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Antenatal consultations; Periodicity; Screening activities; Prophylaxis interventions; Kamina
Quality of Antenatal Care and its Determinants in the Urban-Rural Environment of Kamina, Democratic Republic of the Congo
Ignace Bwana Kangulu1*, Jules Ngwe Thaba Moyambe2, Michel Kabamba Nzaji3, Ange Assumani Kibibi4, Alain Mbayo Kazadi1, Elie Kilolo Ngoy Umba1, John Ngoy Lumbule1, Eric Kiwele Zongwe1, Xavier Kinenkinda Kalume2, Albert Mwembo Tambwe A'Nkoy2 and Jean Baptiste Kakoma Sakatolo2
1Department of Gynecology and Obstetrics, Faculty of Medicine, University of Kamina, Kamina, Democratic Republic of the Congo
2Department of Gynecology and Obstetrics, Faculty of Medicine, University of Lubumbashi, Lubumbashi, Democratic Republic of the Congo
3School of Public Health, University of Kamina, Kamina, Democratic Republic of the Congo
4Higher Institute of Medical Techniques of Kamina, Kamina, Democratic Republic of the Congo
*Address for Correspondence: Ignace Bwana Kangulu, University of Kamina, Kamina, Democratic Republic of the Congo, Email: [email protected]
Introduction: Every woman should receive quality antenatal care during pregnancy wherever she lives. We carried out this research with the objective of evaluating the quality of antenatal consultations (ANC) in terms of periodicity, screening, and prophylaxis interventions during antenatal consultations in Kamina and to identify the determinants associated with inadequate ANC.
Material and methods: This was a descriptive and analytical cross-sectional study carried out in 6 health facilities in Kamina over a period of 17 months with 476 women who had given birth having attended antenatal consultations at least once. A scoring grid of periodicity standards, screening, and prophylactic interventions with a score of 40 was used to qualify the ANC as adequate. Logistic regression was performed to identify the determinants of inadequate ANC.
Results: 40.3% of mothers had reached at least 4 antenatal visits (3.4±1.36); 21.2% had started the ANC no later than 16 weeks for an average age of 22.8 weeks ± 6.19. Overall, 72.5% of pregnant women had benefited from ANC qualified as inadequate. After adjustment, the determinants of inadequate ANC were multigestity (aOR=1.86[1.08-3.19]), low level of education of the mother (aOR=3.93; 95% CI=[2, 08-7.42]), and attendance at a first-level health facility (aOR=3.22; 95% CI=[2.06-5.05].
Conclusion: In the majority of cases, the ANC received by pregnant women in Kamina is inadequate. The determinants thus identified should serve the actors to direct the means to improve the quality of antenatal care in Kamina.
Antenatal care is defined as the care provided by trained health professionals to pregnant women and adolescents to ensure the best health conditions for both mother and child during pregnancy. They help identify risk factors, prevent and manage certain pregnancy-related or concomitant diseases, as well as health education and health promotion [1-3].
The World Health Organization (WHO) envisions a world in which “every pregnant woman and child receives quality care throughout pregnancy, childbirth and the postnatal period”. However, nearly 303,000 women and adolescent girls died in 2015 from obstetric complications, of which nearly 99% of maternal deaths occurred in low-resource settings, and were preventable Since 2016, at the beginning of the era of the Development Goals Sustainable (SDGs), WHO had established a new model of antenatal care which the goal was to provide pregnant women with respectful, individualized, person-centered care at every contact, by implementing effective integrated clinical practices, with practitioners with good clinical and relational skills to provide them with relevant and timely information as well as psychological and emotional support, in a well-functioning health system[4].
In the Democratic Republic of Congo (DRC), access to emergency obstetric and neonatal care is still low. Health facilities, both basic and reference, have very limited means of intervention. In addition, qualified health personnel are very insufficient, especially in rural areas where the majority of the Congolese population lives [5]. The quality of prenatal care poses a problem and does not always reduce the long-awaited maternal and perinatal morbidity and mortality. A clinical audit was carried out in Kinshasa, the capital of the country, with the aim of evaluating the standards of the realization of the ANC within the Luyindu Hospital Center to measure the degree of conformity of the practice with the criteria of the reference system of the National Program of the Reproductive Health had shown significant discrepancies with observed practice. Yet the standards require that all activities and interventions be 100% completed [6].
However, in the province of Haut-Lomami, more particularly in Kamina and its surroundings, studies on prenatal consultations are almost non-existent. In view of all the above, we carried out this study with the aim of contributing to the health of the mother-child couple by specifically seeking to assess the quality of the ANCs carried out in Kamina in terms of periodicity standards, screening, and prophylactic interventions compared to the reference system of the National Program for Reproductive Health in force in our country and to identify the determinants of inadequate ANC.
Study setting
The study was carried out in six health facilities in the urban-rural health zone of Kamina in the DRC selected by a reasoned choice: University Clinics, the General Reference Hospital, SNCC Clinic, Shungu Memorial Health center, Bumi Health Center, and the Monseigneur Malunga polyclinic.
Type and period of study
This was a cross-sectional descriptive and analytical study carried out in the year 2022.
Study population and sample
The study involved all mothers who gave birth at term in the health facilities concerned by the survey and were eligible for the inclusion criteria. The size of our exhaustive sample was 476.
Inclusion criteria
− Have attended prenatal consultations in a health facility in Kamina (at least one visit),
− Full-term birth (at least 38 WA) and
− Have access to the prenatal consultation book.
Collection of data: Data collection was done by teams of investigators briefed beforehand. The information collected by interviewing the mother and reviewing the ANC notebook was recorded on a pre-established data collection sheet.
Criteria for evaluating the quality of antenatal consultations
There is no universally accepted or recognized tool to assess the quality of services at the ANC. The existing tools found in the literature are different according to the authors and the countries [7-12]. Taking into account the standards in force in the DRC [13], the information on the elements of the pregnancy follow-up book used as well as certain scores developed in the literature [7-12], we selected 3 groups of criteria to assess the quality of prenatal consultations. These criteria relate to the standards of periodicity, screening, and prophylaxis for a total score of 40 (Table 1).
| Table 1: Evaluation grid for prenatal consultations in Kamina. | |||||
| NO | Standards | Citation | Total | ||
| 0 | 1 | 2 | |||
| 1 | Number of ANC | 0 | < 4 | ≥ 4 | 02 |
| 2 | First ANC | - | > 14WA | ≤ 14WA | 02 |
| 3 | Number ANC in the third trimester of pregnancy | 0 | < 2 | ≥ 2 | 02 |
| 4 | Blood pressure monitoring | No | Sometimes | Every time | 02 |
| 5 | Maternal weight monitoring | No | Sometimes | Every time | 02 |
| 6 | Fundal Height and Fetal heart rate socked | No | Sometimes | Every time | 02 |
| 7 | Hemoglobin essay | No | 1 time | 2 or more times | 02 |
| 8 | Malaria RDT | No | 1 time | 2 or more times | 02 |
| 9 | Urine examination | No | 1 time | 2 or more times | 02 |
| 10 | Blood glucose test | No | 1 time | 2 or more times | 02 |
| 11 | HIV serology | No | - | Yes | 02 |
| 12 | Syphilis serology | No | - | Yes | 02 |
| 13 | Ultrasound | No | 1 time | 2 or more times | 02 |
| 14 | Health education | No | Sometimes | Every time | 02 |
| 15 | Tetanus vaccination | No | Irregularly | Regularly | 02 |
| 16 | Iron and folic acid supplementation | No | Irregularly | Regularly | 02 |
| 17 | Sulfadoxine Pyriméthamine | No | 1-2 doses | 3 doses or more | 02 |
| 18 | Mebendazol | No | - | Yes | 02 |
| 19 | Use of LLIN | No | Irregularly | Regularly | 02 |
| 20 | Treatment of screening or diagnosed illnesses | - | No | Yes | 02 |
| Total score | 40 | ||||
The classification of ANCs was made as follows:
− Excellent ANC: score ≥ 35 out of 40 i.e. > 85%,
− Very good ANC: score ranging from 28 to 34, i.e. from 70% to 85%,
− Intermediate ANC: score ranging from 20 to 27 out of 40, i.e. from 50% to 69%,
− Poor ANC: score ranging from 16 to 19, i.e. from 40% to 49% and
− Bad ANC with a score of less than 16 out of 40 or < 40%.
To identify the determinants of ANC quality, respondents with a score ≥ 70% (adequate ANC) were compared with those with a score < 70% (inadequate ANC).
Data analysis
Our data have been processed and descriptive statistical analyzes (%, means and standard deviations) realized thanks to the software IBM SPSS Statistics 23. In the bivariate analysis, the OR and its 95% CI, as well as the chi-square test, were used to test the association between the dependent variable (quality of the ANCs) and the independent variables (socio-demographic characteristics and obstetric history of the mother and the level of the health unit that organized the ANCs). Measures of association were considered statistically significant when the p-value was less than 0.05 and or when the lower bound of the 95% CI was ≥ 1. A logistic regression was performed to retain the determinants of inadequate prenatal consultations.
Ethical considerations
Mothers had received sufficient information on study objectives and on the interest of their participation. Mothers' Participation in this Study was free, voluntary without constraint. All information collected from participants was confidential. Only the restricted research team had access to it. A free and informed consent form was presented and read by each respondent. To ensure confidentiality, data were collected anonymously. This study caused no respondents morbidity and a favorable opinion from the Ethics Committee of the University of Lubumbashi was required and obtained at the start of the study (approval letter No UNILU/CEM/021/2020).
Frequency of antenatal consultations
40.3% of mothers had reached at least 4 antenatal visits (3.4 ± 1.36); 21.2% had started the ANC no later than 16 weeks for an average age of 22.8 weeks ± 6.19. However, considering the number of ANCs in the third trimester of pregnancy, 67.0% had reached at least 2 visits. Only a minority of women delivered, i.e. 13.0%, had reached at least 2 visits in the third trimester of pregnancy with ANC1 before the end of 16 weeks.
Screening activities and prophylactic interventions at antenatal consultations
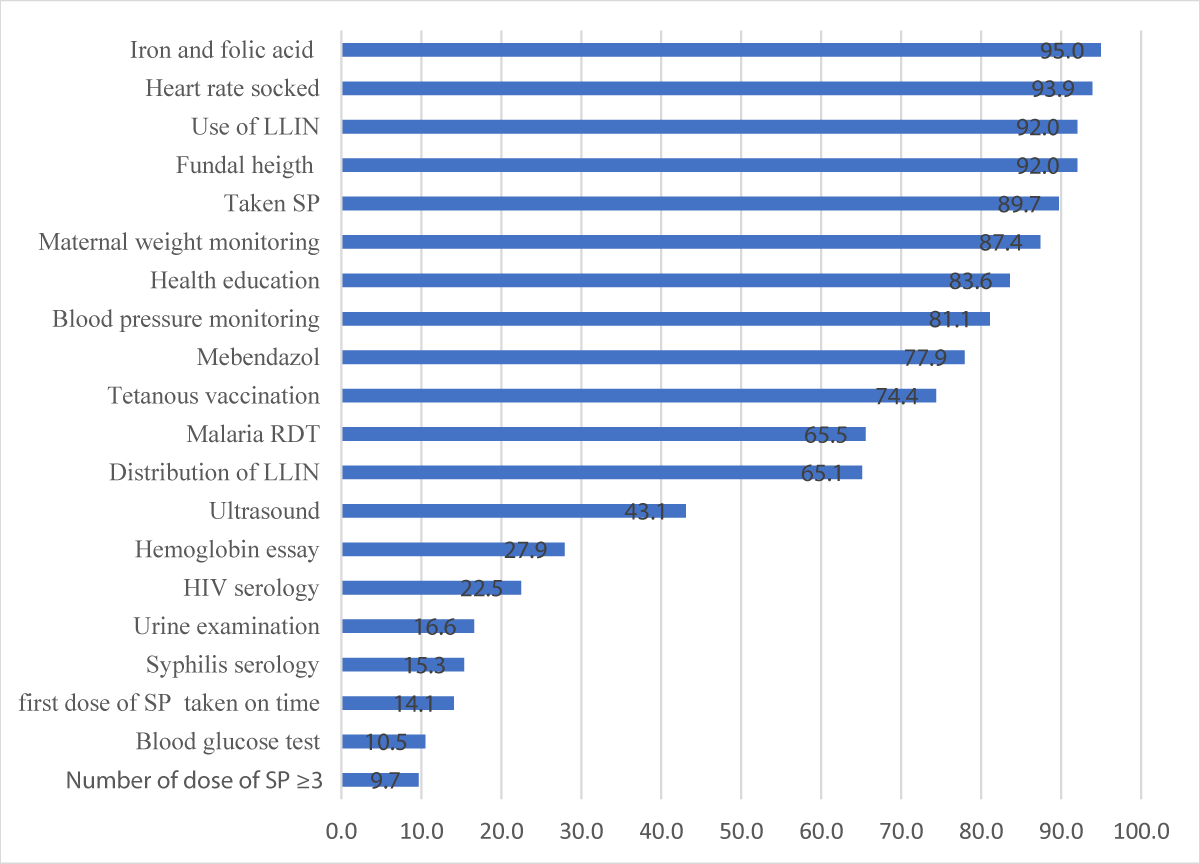
The most performed routine screening activities were taking Fetal heart rate (93.1%), taking Fundal Height (92.0%), taking weight (87.4%), taking blood pressure (81.1%), and malaria Rapid Diagnostic Test (RDT) (65.6%). Regarding malaria prevention during pregnancy, the majority of women giving birth, i.e. 83.6%, had received Sulfadoxine Pyrimethamine; however, only 9.6% had reached the required number of doses (minimum 3 doses) and 14.1% had received the first dose on time. 92.0% reported sleeping during their pregnancy in LLINs. As for nutritional supplementation and deworming, 94.7% of mothers had benefited from iron and folic acid supplementation, and 77.9% were dewormed with Mebendazol. The tetanus vaccine was administered in 74.4% (Figure 1).
Figure 1: Screening activities and prophylactic interventions at ANC.
Overall assessment of the quality of ANC in Kamina
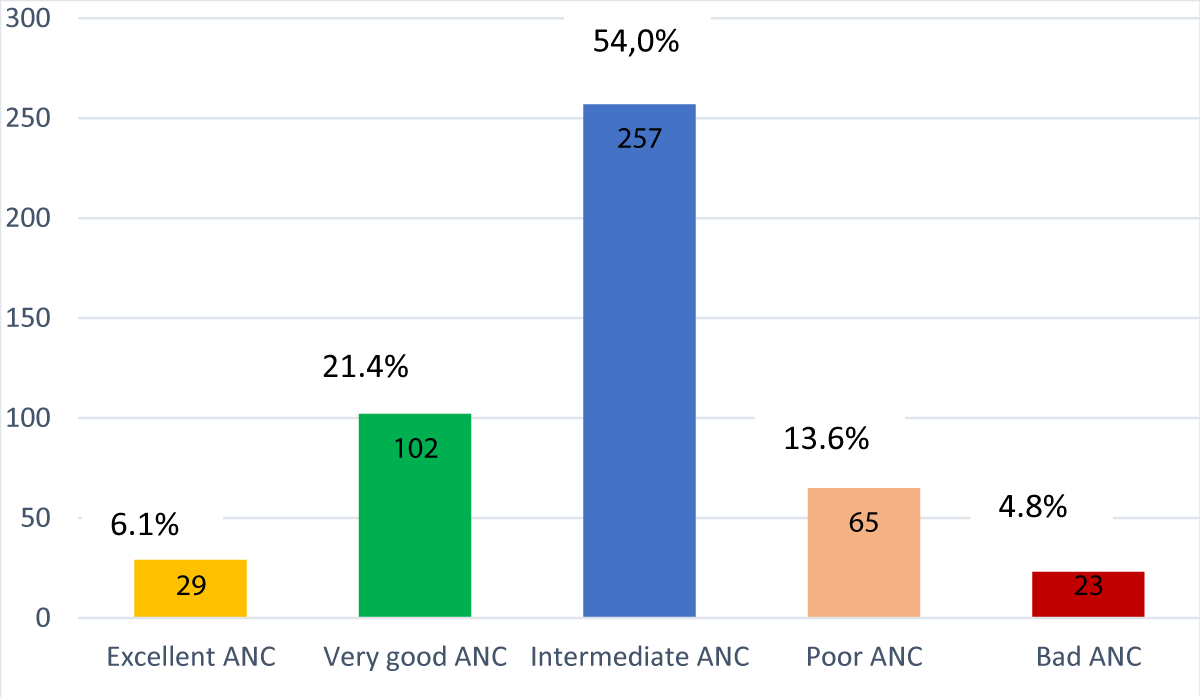
Out of a total of 476 mothers having concerns with this evaluation; 6.1% had had ANC considered Excellent; 21.4% with Very Good ANCs, and 54.0% with Good ANCs. However, ANCs were rated as mediocre and bad respectively 13.6% and 4.8% (Figure 2).
Figure 2: Quality of Antenatal Consultations in Kamina.
Determinants of the adequacy of ANC
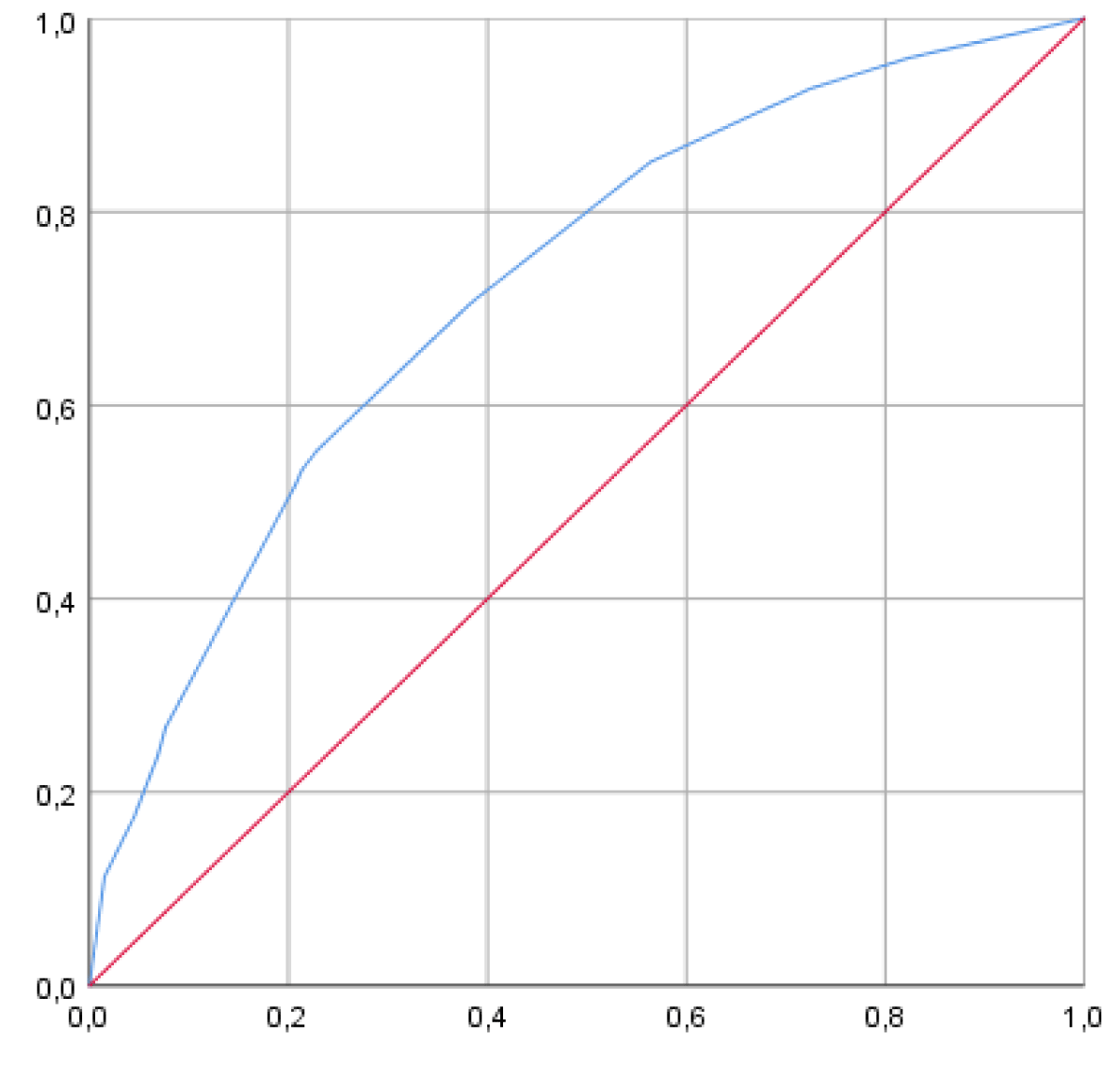
Of all the variables significantly associated with inadequate prenatal consultations in the bivariate analysis (Tables 2-4), only prenatal follow-up in a first-level health facility (OR=3.93; 95% CI=[2.08-7.43]), the low level of education of the mother (OR=3.22; 95% CI=[2.06-5.05]) and multi-gestation (OR=1.22; 95% CI=[1.08-3.19] were selected after multivariate analysis (Table 5). The area under the ROC curve (AUC) values in the figure below indicate a good model performance of 72.2% (67.1-77.3%) (Figure 3).
| Table 2: Association between maternal age, gestality, parity, marital status, occupation, educational level of mother and husband, and quality of ANC. | ||||
| Settings | ANC quality | OR [95%CI] | p | |
| Inadequate (n = 345) | Adequate (n = 131) | |||
| Maternal age | ||||
| < 20 years | 44 (78.6) | 12(21.4) | 0.67[0.34-1.31] | 0.24 |
| 20-35 years old | 252(71.0) | 103(29.0) | 1 | |
| > 35 years old | 49(75.5) | 16(24.6) | 0.80[0.43-1.47] | 0.47 |
| Gestality | ||||
| 1 | 91(70.5) | 38(29.5) | 1.34[0.80-2.23] | 0.26 |
| 2-3 | 93(64.1) | 52(35.9) | 1 | |
| ≥ 4 | 161(79.7) | 41(20.3) | 2.19[1.36-3.56] | 0.001 |
| Parity | ||||
| 1 | 138(70.1) | 59(29.9) | 1.1[0.13-1.76] | 0.71 |
| 2-3 | 90 (68.2) | 42(31.8) | 1 | |
| ≥ 4 | 117(79.6) | 30(20.4) | 1.82[1.15-3.13] | |
| Residence | ||||
| Village | 33(84.6) | 06(15.4) | 2.20[0.90-5.39] | 0.08 |
| Kamina | 312(28.6) | 125(71.4) | ||
| Daily activity | ||||
| No revenue generating | 251(71.1) | 102(28.9) | 0.76[0.47-1.22] | 0.56 |
| recipe generator | 94(76.4) | 29(23.6) | ||
| Marital status | ||||
| Bachelor | 35(76.1) | 11(23.9) | 1.23[0.61-2.50] | 0.56 |
| Married | 310(72.1) | 120(27.9) | ||
| Mother's instruction | ||||
| < secondary | 105(11.0) | 13(89.0) | 3.97[2.14-7.39] | < 0.001 |
| ≥ Secondary | 240(67.0) | 118(33.0) | ||
| Husband's instruction | ||||
| < secondary | 42(91.3) | 04(8.7) | 4.40[1.55-12.53] | 0.003 |
| ≥ secondary | 303(70.5) | 127(29.5) | ||
| Table 3: History of abortion, premature delivery and stillbirth and quality of ANC. | ||||
| Variable | ANC quality | OR [95%CI] | p | |
| Inadequate | Adequate | |||
| History of abortion | ||||
| Yes | 283(70.9) | 116(29.1) | 0.59[0.32-1.08] | 0.08 |
| No | 62(80.5) | 15(19.5) | ||
| History of premature birth | ||||
| Yes | 327(71.7) | 128(28.3) | 0.36[0.11-1.23] | 0.10 |
| No | 21(87.5) | 03(12.5) | ||
| History of stillbirth | ||||
| Yes | 319(71.7) | 126(28.3) | 0.49[0.18-1.30] | 0.14 |
| No | 26(83.9) | 05(16.1) | ||
| Table 4: Association between health facility category and ANC quality. | ||||
| Variable | ANC quality | OR [95%CI] | p | |
| Inadequate | Adequate | |||
| 1st level | 317(80.1) | 79(19.9) | 7.45[4.42-12.55] | < 0.001 |
| 2nd level | 28(35.0) | 52(65.0) | ||
| Table 5: Multivariate analysis of the different variables associated with inadequate ANC in Kamina. | ||
| Variable | aOR[IC95] | p |
| Mother's instruction | 3.93[2.08-7.43] | < 0.001 |
| Health facility level | 3.22[2.06-5.05] | < 0.001 |
| Gesture ≥4 | 1.82[1.08-3.19] | 0.025 |
Figure 3: ROC curve of determinants of inadequate antenatal care in Kamina.
Periodicity of ANC
A minority of mothers (40.3%) had reached at least 4 (3.4 ± 1.36) ANCs as recommended by the country standard [13]. The insufficient number of visits is justified by the late start of ANC by the majority of pregnant women. This situation remains worrying and does not allow providers to correctly offer all the recommended interventions during ANC and prelude to challenges faced by our healthcare system in the feasibility of the 2016 WHO model which recommends a minimum of eight contacts [2]. Several studies carried out in developing countries, in both urban and rural areas, have highlighted this observation. By way of illustration, only 12% of pregnant women had reached at least 4 antenatal visits in a study conducted in Kinshasa [6]; this rate was 12.3% in a study conducted in Ethiopia [14] and 23.3% in that of Yirimadio in a health district of commune VI of Bamako [15].
The onset of ANC was late at approximately 80%. The average age of pregnancy at the start of the prenatal consultations was 22.8 weeks ± 6.19 (4-38 weeks). Several studies carried out in developing countries observed the late start of ANC in the majority of cases [15-18]. For Mafuta and Kayembe in the DRC, the ANC attendance was late in 59.8% [18]. A study conducted in Douala, Cameroon in 2014 found that the average gestational age at ANC1 was 16SA+3 days ± 6SA+3, and 62% of ANC1 were late [16].
Dereje, et al. [19] in their study conducted in Arba Minch Zuria in Ethiopia also found that the majority of the mothers (78.7%) visited their first ANC lately, and 25.2% of mothers attended ≥ 4 ANC visits
A recent study in Ethiopia on factors associated with timely initiation of antenatal care at Wachemo University Nigist Eleni Mohammed Memorial Comprehensive Specialized Hospital indicated that y indicated that only 34.3% of the women initiated ANC timely. The factors associated with the timely initiation of ANC were women aged 25–34 years, tertiary maternal education, zero parity, planned pregnancy, good knowledge about ANC services, and good knowledge about danger signs in pregnancy [20].
Indeed, the late start of ANC does not allow the pregnant woman to reach the required number of visits and to benefit from all recommended interventions in real-time. In our environment, several reasons can justify this situation, in particular the ignorance of the age to begin antenatal consultations and the interest even to begin them precociously. The experience of previous pregnancies can also positively or negatively influence the late start of antenatal consultations. In a study conducted in the Republic of South Africa, pregnant women said they wanted to hide their pregnancy at first for fear of miscarriage. Barriers to early initiation of antenatal care also included women's need to balance income-generating activities and travel costs to clinical [21].
Considering the number of ANCs in the third trimester of pregnancy, 67.0% had reached at least 2 visits (1.87 ± 0.77). Only a minority of pregnant women i.e. 13.0% had reached at least 2 visits in the third trimester of pregnancy with ANC1 before the end of the 16 weeks. In an effort to improve the quality of antenatal care and maternal, fetal, and neonatal outcomes related to antenatal care, the WHO recommends 5 scheduled contacts in the third trimester of pregnancy [2].
Screening activities at prenatal consultations
None of the recommended screening activities has been carried out 100%, while some may, if omitted, miss a maternal or fetal pathology that could complicate the pregnancy. These findings relate to those of a study carried out in Guinea Conakry on the evaluation of the quality of prenatal consultations. In the latter, no routine examination recommended during pregnancy was carried out 100% [22]. The reasons are multiple and can be related to providers who do not recommend them, material resources and the availability of inputs in the health establishments as well as the financial cost of the examinations, the costs being borne generally by the pregnant women themselves. In our community, some screening tests such as the RDT for malaria, HIV and syphilis serologies are offered free of charge, yet only 22.5% of mothers were screened for HIV and 15.3% for syphilis. This contradiction is justified by stock shortages common in screening tests.
Prophylactic interventions during pregnancy
The majority, 83.6%, had received Sulfadoxine Pyrimethamine (SP). However, only 9.6% had reached the required number of doses (minimum 3 doses) and 14.1% had received the first dose on time. 92.0% of mothers said they slept during their pregnancy under an insecticide-treated mosquito net (the LLIN). Only 17.1% of mothers received all the eight selected elements of ANC services in Haile’s study and al in Ethiopia [19].
According to the WHO, malaria in pregnancy is a major public health problem that poses significant risks to mothers and their babies. The low proportion (9.6%) of pregnant women who received at least 3 doses as recommended is linked to the late start of ANC, SP being given free from 14 weeks at each prenatal visit.
As for supplementation and deworming, 94.7% of the mothers had benefited from iron and folic acid supplementation, and 77.9% were dewormed with Mebendazol. Td against tetanus and diphtheria was administered in 74.4% of cases. These interventions are generally offered free of charge at prenatal consultations. The delivery of prescriptions for iron, folic acid, and Mebendazol in the event of a stock shortage could explain the fact that some pregnant women did not benefit from them.
The overall quality of antenatal consultations in Kamina
Overall, the antenatal consultations carried out in Kamina were adequate in only 27.5% and inadequate in 72.5%. In other developing countries like ours, studies had also found a low rate of pregnant women who had benefited from adequate prenatal consultations during their pregnancy, the norms and scoring criteria of the ANC used have several points in common[7,9,11,14].
However, only 30% of women received care with all recommended components in Blackstone’s study conducted in Liberia [23].On the contrary, a study conducted in Mexico with 9052044 women found that 98.4% of women received antenatal care during their last pregnancy, but only 71.5% received maternal health care classified as adequate. Significant geographic differences in coverage of care were identified among states [24].
This situation will not make it possible to achieve the objectives so much sought after by antenatal consultations because inadequate ANCs are associated, according to several studies, with an increase in maternal and perinatal morbidity and mortality [7,8,21-25].
Determinants of inadequate ANC in Kamina
The present study found in a multivariate analysis that inadequate ANC in Kamina was significantly associated with attendance at a first-level health facility (OR=3.93; 95% CI= [2.08-7.43]).
The proportion of inadequate and late antenatal care was 34% and 25% in Saudi. Inadequate antenatal care was independently associated with employed mothers and high parity (three or more) [26-30].
In the DRC, the ANC is an activity of the minimum package of activities of a health center. Higher-level health facilities, such as the General Reference Hospital and University Clinics organize reference prenatal consultations. The poor technical platform of first-level health facilities as well as the level of training of service providers compared to higher-level health facilities are the main reasons.
Similarly, the mother's low level of education (OR=3.22; 95% CI=[2.06-5.05]) remained significantly associated with inadequate ANC. There is a positive link between a woman's level of education and the use of health services. It allows women to acquire a certain autonomy; they then have more latitude to make decisions relating to their health and that of the child. The education of women, their occupation, and their exposure to the media remain a privileged framework for women to break with cultural and traditional practices which are often impermeable to the use of prenatal care considered as a modern practice [31]. In addition, education also increases the standard of living due to the possibility of accessing better-paid jobs, which increases the financial capacity to pay for health care [32].
Finally, it was found that gestation ≥ 4 was associated with inadequate prenatal consultation (OR=1.22; 95% CI=[1.08-3.19]. It is likely that primigravida is more worried while multi gestures would be confident thanks to the experience accumulated in the past. Indeed, women perceive risks associated with the first pregnancy and tend to use more maternal health care services and respect the recommendations of providers in terms of frequency of screening activities and prophylactic interventions, which improves the quality of their ANC.
The ANC carried out in the Kamina health facilities is inadequate in the majority of cases. Efforts should be made at all levels, in particular on the side of the political and administrative authorities, the providers, the pregnant woman, and her entourage, each as far as they are concerned, to improve the quality of the ANC in its periodicity, the screening activities and prophylactic interventions.
- WHO. To make every child count. 2017;156.
- WHO. Who recommendations on antenatal care for a positive pregnancy experience. 2016;10. http://apps.who.int/bookorders.%0Ahttp://apps.who.int/iris/bitstream/10665/250801/1/WHO-RHR-16.12-fre.pdf?ua=1
- WHO. Who recommendations on antenatal care for a positive pregnancy experience: abstract. 2018;10(1):1–13.
- WHO. Who recommendations on antenatal care for a positive pregnancy experience. Geneva; 2017;158.
- ESP and ICF. DRC: Evaluation of health service delivery(EPSS RDC) 2017-2018. RDC and Rockville, Maryland, USA: ESPK and ICF. 2019;15.
- Matondo BA. Normative evaluation of the prenatal consultation with pregnant women who attend the Luyindu Hospital Center in Kinshasa in the Democratic Republic of Congo. 2016.
- Amponsah-Tabi S, Dassah ET, Asubonteng GO, Ankobea F, Annan JJK, Senu E, Opoku S, Opoku E, Opare-Addo HS. An assessment of the quality of antenatal care and pregnancy outcomes in a tertiary hospital in Ghana. PLoS One. 2022 Oct 12;17(10):e0275933. doi: 10.1371/journal.pone.0275933. PMID: 36223426; PMCID: PMC9555636.
- Arroyave L, Saad GE, Victora CG, Barros AJD. A new content-qualified antenatal care coverage indicator: Development and validation of a score using national health surveys in low- and middle-income countries. J Glob Health. 2021 Jan 30;11:04008. doi: 10.7189/jogh.11.04008. PMID: 33692892; PMCID: PMC7916319.
- Kyei NN, Chansa C, Gabrysch S. Quality of antenatal care in Zambia: a national assessment. BMC Pregnancy Childbirth. 2012 Dec 13;12:151. doi: 10.1186/1471-2393-12-151. PMID: 23237601; PMCID: PMC3536568.
- Yeoh PL, Hornetz K, Shauki NIA, Dahlui M. Evaluating the quality of antenatal care and pregnancy outcomes using content and utilization assessment. Int J Qual Health Care. 2018 Jul 1;30(6):466-471. doi: 10.1093/intqhc/mzy041. PMID: 29590356.
- Tadele A, Teka B. Adequacy of prenatal care services and associated factors in Southern Ethiopia. Arch Public Health. 2021 Jun 7;79(1):94. doi: 10.1186/s13690-021-00614-3. PMID: 34099020; PMCID: PMC8183068.
- Watson A, Hernandez L, Thompson D. Adequacy of Prenatal Care Utilization Index and Adverse Birth Outcomes, Florida 2016. Florida Haelth. 2018;0-4.
- RDC-MINISANTE. Health Zone Standards for Integrated Maternal, Newborn and Child Health Interventions in the Democratic Republic of Congo. SONU. 2012;1:99.
- Kassaw A, Debie A, Geberu DM. Quality of Prenatal Care and Associated Factors among Pregnant Women at Public Health Facilities of Wogera District, Northwest Ethiopia. J Pregnancy. 2020 Jan 29;2020:9592124. doi: 10.1155/2020/9592124. PMID: 32411469; PMCID: PMC7204156.
- Traore BM, Diarra AS, Diallo H, El Fakir S, Nejjari C. Antenatal consultations at the Yirimadio community health center. Rev Marocaine Santé Publique. 2018;5:2-8.
- Nguefack TC, Dourwe TG, Njamen TN, Kenfack B, Priso Belley E. Determinants of gestational age at first prenatal consultation in Douala (Cameroun). J SAGO. 2018;19:1-6.
- Botawaosenge Ted L, Natuhoyila Aliocha N, Ngwala Philippe L, Batumanitu Joel M, Mwimba Roger M. Determinants of Delay in First Prenatal Consultation at Hospital Environment in Kimpese Health Zone in Democratic Republic of Congo: Cross-sectional Study. J Heal Environ Res. 2020;6(3):98-103.
- Mafuta E, Kayembe P. Late antenatal care attendance, main determinants, in health zones of Katanga and Equateur, DR Congo. Ann Africaines Médecine. 2011;4(4):845-54.
- Haile D, Habte A, Bogale B. Determinants of Frequency and Content of Antenatal Care in Postnatal Mothers in Arba Minch Zuria District, SNNPR, Ethiopia, 2019. Int J Womens Health. 2020 Nov 3;12:953-964. doi: 10.2147/IJWH.S261705. PMID: 33177886; PMCID: PMC7650005.
- Tessema D, Kassu A, Teshome A, Abdo R. Timely Initiation of Antenatal Care and Associated Factors among Pregnant Women Attending at Wachemo University Nigist Eleni Mohammed Memorial Comprehensive Specialized Hospital, Hossana, Ethiopia: A Cross-Sectional Study. J Pregnancy. 2023 Mar 16;2023:7054381. doi: 10.1155/2023/7054381. PMID: 36970108; PMCID: PMC10036173.
- Jinga N, Mongwenyana C, Moolla A, Malete G, Onoya D. Reasons for late presentation for antenatal care, healthcare providers' perspective. BMC Health Serv Res. 2019 Dec 30;19(1):1016. doi: 10.1186/s12913-019-4855-x. PMID: 31888616; PMCID: PMC6937646.
- Baldé IS, Diallo FB, Diallo MH, Sylla I, Bah EM, Mamy MN. Quality Assessment of the Last Prenatal Consultation at a Peripheral Maternity Center in Guinea, Conakry. Rev Médecine Périnatale. 2016;8(1):39–45.
- Blackstone SR. Evaluating antenatal care in Liberia: evidence from the demographic and health survey. Women Health. 2019 Nov-Dec;59(10):1141-1154. doi: 10.1080/03630242.2019.1590496. Epub 2019 Mar 27. PMID: 30917774.
- Heredia-Pi I, Servan-Mori E, Darney BG, Reyes-Morales H, Lozano R. Measuring the adequacy of antenatal health care: a national cross-sectional study in Mexico. Bull World Health Organ. 2016 Jun 1;94(6):452-61. doi: 10.2471/BLT.15.168302. PMID: 27274597; PMCID: PMC4890208.
- Linard M, Blondel B, Estellat C, Deneux-Tharaux C, Luton D, Oury JF, Schmitz T, Mandelbrot L, Azria E; PreCARE study group. Association between inadequate antenatal care utilisation and severe perinatal and maternal morbidity: an analysis in the PreCARE cohort. BJOG. 2018 Apr;125(5):587-595. doi: 10.1111/1471-0528.14794. Epub 2017 Aug 2. PMID: 28631308.
- Oyerinde K. Can Antenatal Care Result in Significant Maternal Mortality Reduction in Developing Countries ? J Community Med Heal Educ. 2013;3(January 2013):1–3.
- Mundhra R, Singh A, Agarwal M, Kumar R. Utilization of antenatal care and its influence on fetal-maternal outcome: a tertiary care experience. Int J Reprod Contraception, Obstet Gynecol. 2013;2(4):600.
- Manjavidze T, Rylander C, Skjeldestad FE, Kazakhashvili N, Anda EE. The impact of antenatal care utilization on admissions to neonatal intensive care units and perinatal mortality in Georgia. PLoS One. 2020 Dec 2;15(12):e0242991. doi: 10.1371/journal.pone.0242991. PMID: 33264324; PMCID: PMC7710101.
- McDiehl RP, Boatin AA, Mugyenyi GR, Siedner MJ, Riley LE, Ngonzi J, Bebell LM. Antenatal Care Visit Attendance Frequency and Birth Outcomes in Rural Uganda: A Prospective Cohort Study. Matern Child Health J. 2021 Feb;25(2):311-320. doi: 10.1007/s10995-020-03023-0. Epub 2020 Nov 17. PMID: 33201450; PMCID: PMC7878332.
- Al-Wutayd O. Inadequate and Late Antenatal Contacts Among Saudi Mothers: A Hospital-Based Cross-Sectional Study. Int J Womens Health. 2020 Sep 14;12:731-738. doi: 10.2147/IJWH.S265941. PMID: 32982477; PMCID: PMC7500838.
- Guindo MMA. Use of Prenatal Care in Mali : An Analysis of the Quality of Care. ESI Prepr. 2023;301–32.
- Nkurunziza M. Analysis of the use of obstetric care in Burundi: Determinants and motivations: Leuven University Press; 2015.