More Information
Submitted: May 26, 2023 | Approved: June 27, 2023 | Published: June 28, 2023
How to cite this article: Hantoushzadeh S, Mirnia K, Sadeghi HS, Sadeghimoghadam P, Aghaali M, et al. Neonatal Mortality Rate among Twin and Singleton Births with the Gestational Age of 34-37 Weeks: A Population-Based Study. Clin J Obstet Gynecol. 2023; 6: 088-094.
DOI: 10.29328/journal.cjog.1001134
Copyright License: © 2023 Hantoushzadeh S, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Twins; Perinatal mortality; Risk factors; Cesarean section; Premature birth
Neonatal Mortality Rate among Twin and Singleton Births with the Gestational Age of 34-37 Weeks: A Population-Based Study
Sedigheh Hantoushzadeh1, Kayvan Mirnia2, Hananeh Sadat Sadeghi3, Parvaneh Sadeghimoghadam4*, Mohammad Aghaali5, Mohammad Heidarzadeh6, Abbas Habibelahi7, Shima Rafiee8, Mohammad Haddadi1 and Amir Naddaf9
1Vali-E-Asr Reproductive Health Research Center, Family Health Research Institute, Tehran University of Medical Sciences, Tehran, Iran
2Children Medical Center, Pediatric Center of Excellence. Tehran University of Medical Sciences, Tehran, Iran
3Department of Demography, Tehran University, Tehran, Iran
4Department of Pediatrics, Vali-E-Asr Reproductive Health Research Center, Family Health Research Institute, Tehran University of Medical Sciences, Tehran, Iran
5Department of Family and Community Medicine, Qom, Iran
6Department of Pediatrics, Zahedan University of Medical Sciences, Zahedan, Iran
7Neonatal Health Office. MOME.IR IRAN, Tehran, Iran
8School of Medicine, Tehran University of Medical Sciences, Tehran, Iran
9Department of Pediatrics, School of Medicine, Maternal, Fetal, and Neonatal Research Center, Family Health Institute, Vali-E-Asr Hospital, Imam Khomeini Hospital Complex, Tehran University of Medical Sciences, Tehran, Iran
*Address for Correspondence: Parvaneh Sadeghimoghadam, Department of Pediatrics, Vali-E-Asr Reproductive Health Research Center, Family Health Research Institute, Tehran University of Medical Sciences, Tehran, Iran, Email: [email protected]
Introduction: Twin pregnancy, compared to a singleton pregnancy, is associated with a higher risk of preterm birth and other neonatal complications. This study aimed to compare neonatal mortality rates and risk factors among births with the gestational age of 34 weeks - 37 weeks in twin and singleton pregnancies.
Methods: The study design was cross-sectional and population-based. We extracted the data from the birth information registry in Iran. Mothers' and neonates' information was removed from the registry systems between 2018 and 2020. We used Statistical R software to compare neonatal mortality rate, demographic variables, and risk factors between two groups of twin and singleton neonates.
Results: Out of 579,873 live births with a gestational age of 34 weeks - 37 weeks, 729 (1.4/1000) singleton and 54(0.77/1000) twins (one out of two) neonates died in the delivery room in the first hour of life. Of the neonates who left the delivery room alive, 3129 (4.9 per 1000) neonates had died (5.7/1000 singleton and 3.04/1000 twin). The neonatal mortality rate in hospitalized singleton neonates (1.85%) was higher than twin group (1.06%). After adjustment of other variables, the mortality rate in twin pregnancy was significantly lower than in singletons (p value < 1/1000), with an odds ratio of 0.47 (CI: 0.39 - 0.55). Antenatal corticosteroid treatment in the twin group was significantly higher than in singletons.
Conclusion: Twin neonatal mortality rate was lower than singletons in the neonates with gestational age 34 weeks - 37 weeks. Clinicians could consider these results for delivery timing in uncomplicated twin pregnancies. Antenatal corticosteroid therapy can be considered to reduce the mortality rate of late preterm neonates in resource-limited countries.
Over the last 40 years, twin pregnancies have become more frequent, especially in high-income countries [1]. Between 1980 and 2009, the USA experienced an increase in twinning rates from 18.9 to 33.3 per 1000 births. The increased use of Assisted Reproductive Techniques (ARTs) is responsible for this upward trend [2]. Iran is witnessing a similar trend due to the use of ARTs [3]. It is crucial to determine the delivery time in uncomplicated twin pregnancies. The risks of late-preterm birth's adverse outcomes should be taken into account. Compared to a singleton pregnancy, a twin pregnancy is associated with a higher risk of preterm birth and other neonatal complications [4]. Prematurity complications are the leading cause of mortalities and morbidities in multiple pregnancies [5]. Extremely premature twins don't have a higher death rate than singletons [5,6]. However, some studies have found that twins have a higher mortality rate than singletons [7]. The results of previous studies in this field, particularly in late preterm infants, are conflicting and insufficient. This study aimed to compare stillbirths and neonatal mortality in twin and singleton births with gestational age between 34 weeks - 37 weeks. Additionally, we examined the differences in mother and infant characteristics and underlying factors between twin and singleton births concerning mortality.
Study design
Between Mar 21, 2018, and Mar 21, 2020 (the first day of the Persian calendar), a cross-sectional and population-based study was carried out on all singleton and twin births with a gestational age of 34weeks+0 days to 37weeks+6day who needed NICU admission in the neonatal period. The data was extracted from 1. Birth Information Registry (Iranian Maternal and Neonatal Network (IMAN) registry, www.iman.health.gov.ir) and 2. the Specialized Newborn Care Registry (contains basic information about newborns hospitalized in the Neonatal Intensive Care Unit (NICU) and specialized neonatal department in all public and private hospitals regardless of the neonatal outcomes (death, transfer, or discharge) in Iran after merging the two datasets based on the national maternal code [8]. Iran's accreditation program for hospitals showed a data registration validity rate of around 85% [9]. Additionally, the investigator determined the gestational age from the first-trimester ultrasonography report.
Excluding criteria
Neonates who were not assigned a national code (born to mothers who were not Iranian) were omitted from both systems. The study did not include live births of triplets or higher-order multiples. Furthermore, infants with birth defects were not included.
Primary outcome
Neonatal mortality was the main outcome of interest. The mortality rate was determined by the number of deaths per 1000 infants, including stillbirths. The mortality rate was divided based on time of occurrence: antepartum (stillbirth), early neonatal death in the delivery room, and late neonatal death after NICU admission. Neonatal death is characterized as a demise from birth to 28 days of age.
Data collection
The information such as the mothers’ demographic characteristics, infant’s birth characteristics, mode of delivery, birth date, number of parity and gravidity, parental consanguinity, abortion history, gestational weeks, mother’s medical history, and risk factors for pregnancy and childbirth, were reported and evaluated among hospitalized neonates.
Statistics
Data analysis was performed with the statistical R software. Chi-square, t-test, univariate logistic regression, and backward stepwise multivariate logistic regression were used to compare the two groups’ demographic variables and risk factors. Multivariable logistic regression was performed to adjust for confounding factors, such as maternal age, delivery type, birth weight, and corticosteroid administration. The level of significance was established at α = 0.05.
Ethics: The Research Ethics Committees of Imam Hospital Complex at Tehran University of Medical Sciences approved the study (IR.TUMS.IKHC.REC.1400.256).
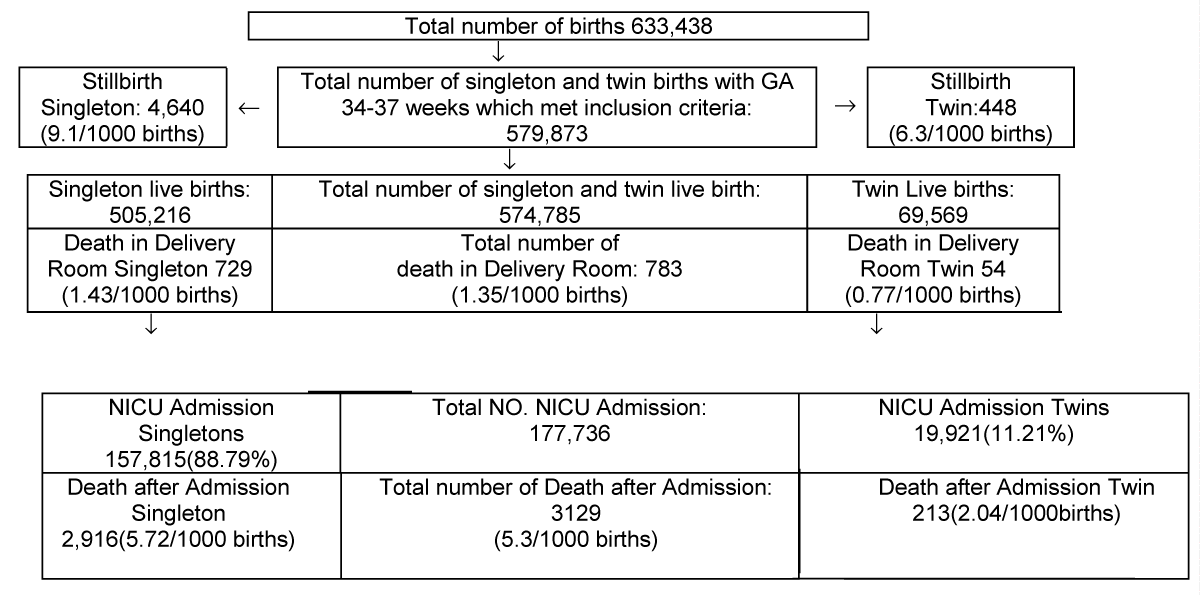
The total number of neonates from 2018 to 2020 was 633,438 after the datasets were merged. A total of 579,873 neonates met the inclusion criteria. This survey recorded 4640 stillbirths (91/1000 births) and 177,736 neonates hospitalized. Of the total, 88.79% (157,815) were singletons, and 11.21% (19,921) were twins. The association between mortality and each candidate predictor is summarized in Table 1. C-sections accounted for 67.92% (120,730) of all deliveries. The rate of cesarean deliveries was higher for twin births than for singletons. Among the singleton group, C-sections were used to deliver 64% of neonates, while in the twin group, the percentage was 95%. The mean birth weight among twins was 2284.84 ± 1945.6 grams, and the mean birth weight of singletons was 2753.85 ± 2427.44 grams. The median birth weight of singletons was 2760 grams. In the twin group, 28.4% were given antenatal corticosteroid treatment, compared to 16.8% in singletons (Figure 1).
| Table 1: Comparison of clinical and demographic characteristics in late preterm birth between singleton and twin pregnancies (survived and died). | ||||||
| Variables | Single | p - value | Twin | p - value | ||
| survived | died | survived | died | |||
| Delivery type | 0.000 | 0.007 | ||||
| vaginal birth | 55080(98.4%) | 875(1.6%) | 1043(99.2%) | 8(0.8%) | ||
| C-section | 99819(98%) | 2041(2%) | 18665(98.9%) | 205(1.1%) | ||
| Gestational age, week | Median (36.00), IQR (2) | Median (35.0), IQR (2) | ||||
| 34 | 19573(96.7%) | 662(3.3%) | 0.000 | 5289(98.6%) | 76(1.4%) | 0.001 |
| 35 | 26171(97.7%) | 618(2.3%) | 5265(98.8%) | 66(1.2%) | ||
| 36 | 39284(98.2%) | 704(1.8%) | 5020(99.3%) | 37(0.7%) | ||
| 37 | 69872(98.7%) | 932(1.3%) | 4134(99.2%) | 34(1.1%) | ||
| Weight (gram) | Mean (2753.854) Median 2760 |
Mean (2427.438) Median 2470 |
0.000 | Mean (2284.841) |
Mean (1945.601) |
0.000 |
| very low birth weight (<1500) | 1284(87.1%) | 190(12.9%) | 0.000 | 449(91.8%) | 40(8.2%) | 0.000 |
| low birth weight (<2500) | 42326(97.1%) | 1277(2.9%) | 13260(99%) | 140(1%) | ||
| normal birth weight (<=4000) | 108895(98.7%) | 1414(1.3%) | 5994(99.5%) | 213(0.5%) | ||
| Corticosteroid administration | ||||||
| has not taken | 92580(98.3%) | 1610(1.7%) | 0.000 |
9649(99%) | 97(1%) | 0.304 |
| full | 16485(98.2%) | 296(1.8%) | 4002(98.9%) | 43(1.1%) | ||
| imperfect | 9552(97.7%) | 225(2.3%) | 1598(98.6%) | 23(1.4%) | ||
| Maternal age (years) | 30.48±6.24 | 30.28±5.93 | ||||
| <20 | 6654(97.7%) | 155(2.3%) | 0.001 | 486(98.2%) | 9(1.8%) | 0.307 |
| 20–29 | 59858(98%) | 1197(2%) | 8456(99%) | 86(1%) | ||
| 30–39 | 77314(98.3%) | 1359(1.7%) | 9605(98.9%) | 108(1.1%) | ||
| ≥40 | 11074(98.2%) | 205(1.8%) | 1158(99.1%) | 10(0.9%) | ||
| Prior pregnancies | Median(0.9981), IQR (2) | Median(0.7342), IQR (1) | ||||
| None | 59249(98.5%) | 914(1.5%) | 0.000 | 10021(99%) | 101(1%) | 0.000 |
| 1 | 55498(98.4%) | 931(1.6%) | 6291(99.1%) | 59(0.9%) | ||
| 2 | 27735(97.8%) | 625(2.2%) | 2452(99%) | 26(1%) | ||
| ≥3 | 12418(96.5%) | 446(3.5%) | 944(97.2%) | 27(2.8%) | ||
| Consanguinity of parents | ||||||
| No | 129460(98.4%) | 2078(1.6%) | 0.000 | 16574(99.1%) | 152(0.9%) | 0.000 |
| Yes | 25440(96.8%) | 838 (3.2%) | 3134(98.1%) | 61(1.9%) | ||
| Childbirth Preparation Classes | ||||||
| No | 141867(98.1%) | 2730(1.9%) | 0.000 | 18477(99%) | 194(1%) | 0.145 |
| Yes | 13033(98.6%) | 186(1.4%) | 1231(98.5%) | 19(1.5%) | ||
| Year | ||||||
| 2018 | 55264 (98.1%) | 1078(1.9%) | 0.012 | 6602(99%) | 70(1%) | 0.421 |
| 2019 | 53495 (98.3%) | 930(1.7%) | 6944(99%) | 68(1%) | ||
| 2020 | 46141 (98.1%) | 908(1.9%) | 6162(99%) | 75(1.2%) | ||
| Artificial Insemination | ||||||
| No | 153023(98.1%) | 2893(1.9%) | 0.047 | 18040(98.9%) | 198(1.1%) | 0.537 |
| Yes | 1877(98.8%) | 23(1.2%) | 1668(99.1%) | 15(0.9%) | ||
| Apgar score | Median (9.00), IQR (1) | Median (9.00), IQR (1) | ||||
| 0-3 | 1382 (71.6%) | 547(28.4%) | 0.000 | 176(88.4%) | 23(11.6%) | 0.000 |
| 4-6 | 5516 (90.4%) | 584(9.6%) | 878(96%) | 37(4%) | ||
| 7-10 | 147998(98.8%) | 1785(1.2%) | 18654(99.2%) | 153(0.8%) | ||
Figure 1: Study flowchart.
Table 1 compares variables related to the mother and neonates and delivery conditions separately for singletons and twins in both the surviving and dead groups. Table 2 shows the outcomes of univariate logistic regression analyses for factors associated with mortality for singletons and twins separately. Gestational age, weight, prior pregnancy, consanguinity of parents, and Apgar score were significant mortality risk factors in hospitalized babies common to singletons and twins (p values < 0.05). Delivery type, corticosteroid administration, and participation in childbirth Preparation Classes were considerable risk factors of mortality in hospitalized babies for singletons (p < 0.001) but not twins (p > 0.05). Table 3 shows the outcomes of multivariate logistic regression analyses for singletons and twins separately and for all neonates with gestational age 34 weeks - 37 weeks (twins as a reference group). Starting with the most comprehensive model, including all risk factors (full model), we used a backward stepwise selection process.
| Table 2: Univariate analysis of associated factors related to neonatal mortality rate by separate logistic regression models for singletons and twins born with gestational age 34 - 37 weeks in Iran, 2018–2020. | |||
| Variables | Singletons | Twins | |
| Odds ratio (95% CI) | Odds ratio (95% CI) | ||
| Gestational Age | 34 (ref) | ||
| 35 | 0.69 (0.62, 0.78)*** | 0.87 (0.62, 1.21) | |
| 36 | 0.52 (0.47, 0.59) *** | 0.51 (0.34, 0.75) *** | |
| 37 | 0.39 (0.35, 0.43) *** | 0.57 (0.37, 0.85) ** | |
| Weight | normal weight(ref) | ||
| very low birth weight | 11.39(9.67,13.35) *** | 16.18 (10.11,26.04) *** | |
| low birth weight | 2.32 (2.15, 2.50) *** | 1.91 (1.32,2.85) *** | |
| Delivery type | vaginal birth (ref) | ||
| C-section | 1.28 (1.18,1.39) *** | 1.43 (0.75,3.17) | |
| Corticosteroid administration | has not taken(ref) | ||
| full | 1.03 (0.90, 1.16) | 1.06 (0.73,1.52) | |
| imperfect | 1.35 (1.17, 1.55) *** | 1.43 (0.88,2.22) | |
| Maternal age (years) | <20 (ref) | ||
| 20–29 | 0.85 (0.72,1.02) | 0.54 (0.29,1.17) | |
| 30–39 | 0.75 (0.64,0.89) ** | 0.60 (0.32,1.29) | |
| ≥40 | 0.79 (0.64,0.98) * | 0.46 (0.18,1.18) | |
| Prior pregnancies | None (ref) | ||
| 1 | 1.08 (0.99,1.19) | 0.93 (0.67,1.28) | |
| 2 | 1.46 (1.31,1.61) *** | 1.05 (0.66,1.56) | |
| ≥3 | 2.32 (2.07,2.60) *** | 2.83 (1.81,4.29) *** | |
| Consanguinity of parents | No(ref) | ||
| Yes | 2.05 (1.89,2.22) *** | 2.12 (1.56,2.84) *** | |
| Childbirth Preparation Classes | No(ref) | ||
| Yes | 0.74 (0.63,0.85) *** | 1.47 (0.88,2.22) | |
| Year | 2018(ref) | ||
| 2019 | 0.89 (0.81,0.97) * | 0.92 (0.65,1.129) | |
| 2020 | 1.00 (0.92,1.10) | 1.14 (0.82,1.59) | |
| Apgar score | 0-3(ref) | ||
| 6-Apr | 0.26 (0.23,0.30) *** | 0.32 (0.18,0.56) *** | |
| 10-Jul | 0.03 (0.02,0.03) *** | 0.06 (0.04,0.10) *** | |
| Artificial Insemination | No(ref) | ||
| Yes | 0.64 (0.41,0.95) * | 0.81 (0.46,1.33) | |
| Signif. codes: 0 '***' 0.001 '**' 0.01 '*' 0.05 '.' 0.1 ' ' | |||
| Table3: Multivariate analysis of associated factors related to late preterm mortalityby separate logistic regression models for singletons and twins born in Iran,2018–2020 (Stepwise Logistic Regression: backward). | |||||
| stage | Variables | Singletons | Twins | Total | |
| Oddsratio(95% CI) | Oddsratio(95% CI) | Oddsratio(95% CI) | |||
| Full model | Singletons(ref) | Fetal number | - | - | |
| Twins | 0.46(0.39,0.55)*** | ||||
| 34 (ref) | Gestational Age | ||||
| 35 | 0.95 (0.82, 1.09) | 0.98 (0.67, 1.44) | 0.95(0.83,1.08) | ||
| 36 | 0.96(0.83, 1.10) | 0.64 (0.39, 1.04) | 0.93(0.82,1.07) | ||
| 37 | 0.86(0.75, 1.00)* | 0.82 (0.48, 1.36) | 0.86(0.75,0.98)* | ||
| normalweight (ref) | Weight | ||||
| verylow weight | 6.01(4.81,7.48)*** | 8.44 (4.75,15.0)*** | 6.59(5.37,8.04)*** | ||
| lowweight | 1.82(1.65, 2.02)*** | 1.36 (0.89,2.14) | 1.79(1.62,1.97)*** | ||
| vaginalbirth (ref) | Delivery type | ||||
| C-section | 1.02(0.93,1.13) | 1.38 (0.68,3.29) | 1.03(0.94,1.14) | ||
| hasnot taken (ref) | Corticosteroid administration | ||||
| full | 0.93(0.81, 1.06) | 1.05 (0.71,1.52) | 0.95(0.83,1.07) | ||
| imperfect | 0.91(0.78, 1.06) | 1.05 (0.63,1.66) | 0.92(0.79,1.07) | ||
| <20(ref) | Maternal age (years) | ||||
| 20–29 | 0.91(0.73,1.13) | 0.64 (0.30,1.58) | 0.88(0.72,1.10) | ||
| 30–39 | 0.65(0.52,0.82)*** | 0.61 (0.28,1.53) | 0.65(0.52,0.81)*** | ||
| ≥40 | 0.53(0.40,0.71)*** | 0.42 (0.15,1.28) | 0.53(0.40,0.69)*** | ||
| None (ref) | Prior pregnancies | ||||
| 1 | 1.27(1.13,1.43)*** | 1.11 (0.75,1.63) | 1.25(1.12,1.40)*** | ||
| 2 | 1.80(1.57,2.06)*** | 1.18 (0.68,1.99) | 1.74(1.53,1.98)*** | ||
| ≥3 | 2.43(2.07,2.85)*** | 2.30 (1.25,4.04)** | 2.42(2.07,2.83)*** | ||
| No(ref) | Consanguinity of parents | ||||
| Yes | 1.73(1.56,1.91)*** | 1.97 (1.38,2.79)*** | 1.75(1.59,1.93)*** | ||
| No(ref) | Childbirth Preparation Classes | ||||
| Yes | 0.78(0.65,0.94)* | 1.56 (0.86,2.62) | 0.82(0.69,0.98)* | ||
| 2018(ref) | Year | ||||
| 2019 | 0.85(0.76,0.95)** | 0.95 (0.64,1.40) | 0.86(0.77,0.95) | ||
| 2020 | 0.95(0.85,1.06 | 0.95 (0.64,1.41) | 0.95(0.85,1.05)** | ||
| 0-3 (ref) | Apgar score | ||||
| 6-Apr | 0.28(0.24,0.33)*** | 0.30 (0.16,0.59)*** | 0.28(0.24,0.32)*** | ||
| 10-Jul | 0.04(0.03,0.04)*** | 0.08 (0.05,0.14)*** | 0.04(0.04,0.05)*** | ||
| No(ref) | Artificial Insemination | ||||
| Yes | 0.91(0.54,1.43) | 1.00 (0.53,1.75) | 0.96(0.65,1.37) | ||
| R2 | 0.14 | 0.1 | 0.14 | ||
| Final model | Singletons(ref) | Fetal number | - | - | |
| Twins | 0.47(0.39,0.55)*** | ||||
| normalweight (ref) | Weight | ||||
| verylow weight | 6.25(5.03,7.72)*** | 9.60 (5.55,16.6)*** | 6.91(5.67,8.37)*** | ||
| lowweight | 1.88(1.72,2.07)*** | 1.48 (0.99,2.29) | 1.86(1.69,2.03)*** | ||
| No(ref) | Childbirth Preparation Classes | ||||
| Yes | 0.78(0.65,0.94)* | 1.58 (0.87,2.65) | 0.83(0.69,0.98)* | ||
| <20(ref) | Maternal age (years) | 0.90(0.73,1.13) | - | ||
| 20–29 | 0.65(0.52,0.82)*** | 0.88(0.72,1.10) | |||
| 30–39 | 0.53(0.40,0.71)*** | 0.65(0.52,0.81)*** | |||
| ≥40 | 0.53(0.40,0.69)*** | ||||
| 2018(ref) | Year | - | |||
| 2019 | 0.85(0.76,0.95)** | 0.86(0.77,0.95)** | |||
| 2020 | 0.95(0.85,1.06) | 0.95(0.85,1.05) | |||
| 0-3(ref) | Apgar score | ||||
| 6-Apr | 0.28(0.24,0.33)*** | 0.31(0.16,0.60)*** | 0.28(0.24,0.32)*** | ||
| 10-Jul | 0.04(0.03,0.04)*** | 0.08(0.05,0.14)*** | 0.04(0.03,0.05)*** | ||
| None(ref) | Prior pregnancies | ||||
| 1 | 1.28(1.14,1.44)*** | 1.06(0.72,1.52) | 1.26(1.13,1.41)*** | ||
| 2 | 1.82(1.59,2.08)*** | 1.11(0.65,1.80) | 1.76(1.55,2,00)*** | ||
| ≥3 | 2.46(2.10,2.88)*** | 2.06(1.17,3.44)** | 2.45(2.10,2.85)*** | ||
| No(ref) | Consanguinity of parents | ||||
| Yes | 1.72(1.56,1.91)*** | 2.04(1.43,2.87)*** | 1.75(1.58,1.93)*** | ||
| R2 | 0.14 | 0.1 | 0.14 | ||
| Signif.codes: 0 '***' 0.001 '**' 0.01 '*' 0.05 '.' 0.1 ' ' 1 | |||||
The rate of stillbirth and death in the delivery room was significantly higher in the singletons group. In hospitalized neonates, the neonatal mortality rate was higher in the singletons (1.85%) than in twins (1.06%). The mortality rate was higher in the singleton group (12.9%) than in the twin group (8.2%) for very low birth weight neonates. The odds ratio of mortality in very low birth weight neonates in the twin group was higher than in the singleton group (16.18 vs. 11.39), but for low birth weight neonates, the odds ratio in the singleton group was higher (2.32 vs. 1.91). The mortality rate was lower in the artificial insemination group than in the others. After adjusting for other variables, the multivariate regression analysis showed that hospitalized neonates in twin pregnancies had a lower mortality rate than singletons, with an odds ratio of 0.47 (CI: 0.39, 0.55). In neonates with gestational age 34 weeks - 37 weeks, twins have a significantly different mortality rate than singletons. The stillbirth, delivery room death, and neonatal mortality rates were lower in twins than in singletons. Mortality rates decline as gestational age increases in both groups. There are numerous explanations for our findings. Our study had a larger sample size compared to earlier ones. A slight difference between the groups can be detected. Antenatal corticosteroids may have been administered more to twins due to their increased risk of preterm birth [10]. In this study, the use of antenatal corticosteroids was more frequent in the twin group. Previous studies have yielded conflicting results. Research shows late preterm singleton infants have a greater mortality risk than term infants. Morbidity risk decreases as gestational age increases [11-15]. Studies have revealed that premature neonates in multiple gestations have a higher risk of morbidity and mortality than full-term neonates [15-17]. No contrast in mortality rates between twins and singletons was found in previous studies [18-20]. Studies reporting equivalent outcomes among singletons and twins in the late preterm often had small sample sizes [21,22]. In a study of 165,894 neonates, Clara Ward et al. found no difference in mortality rates between twins and singletons. A study discovered that twins in the late preterm are at a higher risk of neonatal morbidity. They failed to consider crucial factors like indication for delivery, mode of delivery, or antenatal corticosteroid administration [15]. In a study of 1015 late preterm neonates by Vachharajani, et al. singletons had a higher need for ventilation, but there was no difference in respiratory morbidity between singletons and twins [18]. Our study is consistent with Garite et al.'s findings that neonatal outcomes of multiple gestations are comparable to singletons in a survey of 14,457 twin and triplet births with gestational age between 23 to 35 weeks. According to the study, gestational age and growth restriction are the primary factors leading to mortality in multiple births [23]. According to other studies, twin and triplet neonates have comparable outcomes to singleton [21,24,25]. In a retrospective study conducted by Blank Vask, et al. on 152,120 singleton and 51,658 twin babies whose gestational age was 28 - 43 weeks, results revealed that the rate of stillbirth and neonatal mortality up to the gestational age 37 weeks was higher in twins compared to singletons [26]. Twin fetuses have a clinical impression of accelerated pulmonary maturation, resulting in earlier delivery terms for twins than singleton fetuses. This hypothesis was not supported by some studies [27]. The rate of cesarean sections is higher in neonates born as twins. Respiratory disorder is a crucial problem for twin neonates [28]. Amniotic fluid samples from 454 singletons and 398 twin pregnancies were analyzed by Tsuda et al. According to a study, twin fetuses experience more rapid lung fluid absorption and maturation than singletons [29]. According to their findings, neonatal respiratory distress syndrome and transient tachypnea in newborns at 38 weeks gestation in singleton pregnancies are comparable to that at 36 weeks gestation in twin pregnancies [28]. It is recommended to deliver uncomplicated twin pregnancies earlier to prevent intrauterine death in the last weeks of gestation due to their higher risk than singleton pregnancies [30] and lower neonatal mortality rate during the late preterm period [30]. Antepartum corticosteroids reduce morbidity and mortality of preterm babies under 34 weeks gestation. Recent studies suggest that the beneficial effects of giving antenatal corticosteroids may also extend to late preterm and early-term infants. In most studies conducted in late preterm infants, antenatal corticosteroids reduce the chance of short-term respiratory complications but do not affect the mortality rate [31]. Antenatal corticosteroid benefits in twin pregnancies have been studied less than in singleton pregnancies. Guidelines for administering antenatal corticosteroids in twin pregnancies are based on evidence from singleton pregnancies [31-32]. While studies show varying perinatal mortality rates for twins compared to singletons, recent years have seen a greater reduction in stillbirth and neonatal death rates for twins than for singletons. This achievement owes to the critical role of fetal monitoring in twin pregnancies. The presence of specific guidelines for managing high-risk and twin pregnancies and the ability to treat complications like twin-twin transfusion syndrome during the fetal period are crucial factors [33-35]. Most studies like ours have examined twin mortality overall without considering the impact of chronicity, and the mortality rate of twins has not been explored by zygosity [33].
Study limitations
The study excluded non-Iranian mothers and out-of-hospital deaths and births. Therefore, the results did not reflect the immigrant population in Iran. We accounted for critical factors in this setting (delivery method, antenatal corticosteroid use, and assisted reproductive technology) and applied multivariable logistic regression to account for possible variables.
Our study shows that twins have a lower mortality rate than singletons who delivered between 34 to 37 weeks of gestational age. Delivery timing in uncomplicated twin pregnancies could be affected by these results. Moreover, the roles of antepartum corticosteroids and better prenatal care were considered to improve the outcomes of singleton, such as twin pregnancies which caused a decrease in stillbirth and neonatal death between them. Healthcare providers and policymakers could use these results and demonstrations to make appropriate decisions in the healthcare system to develop and improve maternal-fetal health among developing countries like Iran, and it could be guided to further studies in this field.
We thank Iran's Neonatal Health Office of Health and Medical Education Ministry.
Funding: Tehran University of Medical Sciences
Availability of data and materials: In this study, we used Iranian Maternal and neonatal records (IMAN registry) data; administrative permissions are required to access the dataset.
- Esposito G, Dalmartello M, Franchi M, Mauri PA, Cipriani S, Corrao G, Parazzini F. Trends in Dizygotic and Monozygotic Spontaneous Twin Births During the Period 2007-2017 in Lombardy, Northern Italy: A Population-Based Study. Twin Res Hum Genet. 2022 Jun;25(3):149-155. doi: 10.1017/thg.2022.19. Epub 2022 Jun 29. PMID: 35765814.
- Dawson AL, Tinker SC, Jamieson DJ, Hobbs CA, Rasmussen SA, Reefhuis J; National Birth Defects Prevention Study. Epidemiology of twinning in the National Birth Defects Prevention Study, 1997 to 2007. Birth Defects Res A Clin Mol Teratol. 2015 Feb;103(2):85-99. doi: 10.1002/bdra.23325. Epub 2014 Oct 31. PMID: 25359509; PMCID: PMC4382674.
- Yazdekhasti A, Firouzfar A, Hajheidari P, Havaei A, Tavakol G, Karbasian F. Prevalence of multiple birth in Isfahan, Iran. J Res Med Sci. 2018 Mar 27;23:25. doi: 10.4103/jrms.JRMS_892_16. PMID: 29692822; PMCID: PMC5894274.
- Cho GJ, Cho KD, Kim HY, Ha S, Oh MJ, Won HS, Chung JH. Short-term neonatal and long-term infant outcome of late-preterm twins: nationwide population-based study. Ultrasound Obstet Gynecol. 2022 Jun;59(6):763-770. doi: 10.1002/uog.24838. PMID: 34931725.
- Ray B, Platt MP. Mortality of twin and singleton livebirths under 30 weeks' gestation: a population-based study. Arch Dis Child Fetal Neonatal Ed. 2009 Mar;94(2):F140-3. doi: 10.1136/adc.2008.143016. Epub 2008 Oct 6. PMID: 18838469.
- Asztalos E, Barrett JF, Lacy M, Luther M. Evaluating 2 year outcome in twins < or = 30 weeks gestation at birth: a regional perinatal unit's experience. Twin Res. 2001 Dec;4(6):431-8. doi: 10.1375/1369052012759. PMID: 11780934.
- Synnes AR, Ling EW, Whitfield MF, Mackinnon M, Lopes L, Wong G, Effer SB. Perinatal outcomes of a large cohort of extremely low gestational age infants (twenty-three to twenty-eight completed weeks of gestation). J Pediatr. 1994 Dec;125(6 Pt 1):952-60. doi: 10.1016/s0022-3476(05)82015-3. PMID: 7996370.
- Khatibi T, Kheyrikoochaksarayee N, Sepehri MM. Analysis of big data for prediction of provider-initiated preterm birth and spontaneous premature deliveries and ranking the predictive features. Arch Gynecol Obstet. 2019 Dec;300(6):1565-1582. doi: 10.1007/s00404-019-05325-3. Epub 2019 Oct 24. PMID: 31650230.
- Pourshirazi M, Heidarzadeh M, Taheri M, Esmaily H, Babaey F, Talkhi N, Gholizadeh L. Cesarean delivery in Iran: a population-based analysis using the Robson classification system. BMC Pregnancy Childbirth. 2022 Mar 8;22(1):185. doi: 10.1186/s12884-022-04517-1. PMID: 35260106; PMCID: PMC8903666.
- Esposito G, Dalmartello M, Franchi M, Mauri PA, Cipriani S, Corrao G, Parazzini F. Trends in Dizygotic and Monozygotic Spontaneous Twin Births During the Period 2007-2017 in Lombardy, Northern Italy: A Population-Based Study. Twin Res Hum Genet. 2022 Jun;25(3):149-155. doi: 10.1017/thg.2022.19. Epub 2022 Jun 29. PMID: 35765814.
- Ananth CV, Friedman AM, Gyamfi-Bannerman C. Epidemiology of moderate preterm, late preterm and early term delivery. Clin Perinatol. 2013 Dec;40(4):601-10. doi: 10.1016/j.clp.2013.07.001. Epub 2013 Sep 20. PMID: 24182950.
- Nagasaka M, Morioka I, Yokota T, Fujita K, Kurokawa D, Koda T, Shibata A, Yamada H, Ito Y, Uchino E, Shirai C, Iijima K. Incidence of short stature at 3 years of age in late preterm infants: a population-based study. Arch Dis Child. 2015 Mar;100(3):250-4. doi: 10.1136/archdischild-2014-307045. Epub 2014 Sep 26. PMID: 25260516.
- Dimitriou G, Fouzas S, Georgakis V, Vervenioti A, Papadopoulos VG, Decavalas G, Mantagos S. Determinants of morbidity in late preterm infants. Early Hum Dev. 2010 Sep;86(9):587-91. doi: 10.1016/j.earlhumdev.2010.07.011. Epub 2010 Aug 21. PMID: 20729014.
- King JP, Gazmararian JA, Shapiro-Mendoza CK. Disparities in mortality rates among US infants born late preterm or early term, 2003-2005. Matern Child Health J. 2014 Jan;18(1):233-241. doi: 10.1007/s10995-013-1259-0. PMID: 23519825; PMCID: PMC4407273.
- Ward C, Caughey AB. Late preterm births: neonatal mortality and morbidity in twins vs. singletons. J Matern Fetal Neonatal Med. 2022 Dec;35(25):7962-7967. doi: 10.1080/14767058.2021.1939303. Epub 2021 Jun 21. PMID: 34154507.
- Martinka D, Barrett J, Mei-Dan E, Zaltz A, Melamed N. Respiratory morbidity in late preterm twin infants. Arch Gynecol Obstet. 2019 Aug;300(2):337-345. doi: 10.1007/s00404-019-05191-z. Epub 2019 May 15. PMID: 31093740.
- Refuerzo JS, Momirova V, Peaceman AM, Sciscione A, Rouse DJ, Caritis SN, Spong CY, Varner MW, Malone FD, Iams JD, Mercer BM, Thorp JM Jr, Sorokin Y, Carpenter MW, Lo J, Harper M; Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. Neonatal outcomes in twin pregnancies delivered moderately preterm, late preterm, and term. Am J Perinatol. 2010 Aug;27(7):537-42. doi: 10.1055/s-0030-1248940. Epub 2010 Feb 19. PMID: 20175042; PMCID: PMC2990398.
- Vachharajani AJ, Vachharajani NA, Dawson JG. Comparison of short-term outcomes of late preterm singletons and multiple births: an institutional experience. Clin Pediatr (Phila). 2009 Nov;48(9):922-5. doi: 10.1177/0009922809336359. Epub 2009 May 29. PMID: 19483134.
- Suzuki S, Inde Y, Miyake H. Comparison of short-term outcomes of late pre-term singletons and dichorionic twins and optimal timing of delivery. J Obstet Gynaecol. 2010;30(6):574-7. doi: 10.3109/01443615.2010.494207. PMID: 20701505.
- Zdanowicz JA, Sommer E, Raio L, Nelle M, Gerull R. Do late preterm twins face an increased neonatal morbidity compared with singletons? Swiss Med Wkly. 2018 Jan 4;148:w14581. doi: 10.4414/smw.2018.14581. PMID: 29376553.
- Ribicic R, Kranjcec I, Borosak J, Tumbri J, Mihovilovic Prajz L, Ribicic T. Perinatal outcome of singleton versus twin late preterm infants: do twins mature faster than singletons? J Matern Fetal Neonatal Med. 2016;29(9):1520-4. doi: 10.3109/14767058.2015.1053449. Epub 2015 Jun 24. PMID: 26103779.
- Yoo EH, Chun D, Kim MJ, Cha HH, Seong WJ. Comparison of perinatal outcomes in late preterm birth between singleton and twin pregnancies. Obstet Gynecol Sci. 2017 Sep;60(5):421-426. doi: 10.5468/ogs.2017.60.5.421. Epub 2017 Sep 18. PMID: 28989917; PMCID: PMC5621070.
- Garite TJ, Clark RH, Elliott JP, Thorp JA. Twins and triplets: the effect of plurality and growth on neonatal outcome compared with singleton infants. Am J Obstet Gynecol. 2004 Sep;191(3):700-7. doi: 10.1016/j.ajog.2004.03.040. Erratum in: Am J Obstet Gynecol. 2004 Dec;191(6):2184. PMID: 15467528.
- Kaufman GE, Malone FD, Harvey-Wilkes KB, Chelmow D, Penzias AS, D'Alton ME. Neonatal morbidity and mortality associated with triplet pregnancy. Obstet Gynecol. 1998 Mar;91(3):342-8. doi: 10.1016/s0029-7844(97)00686-8. PMID: 9491857.
- Hedriana HL, Eby-Wilkens EM, Gilbert WM. Perinatal mortality and morbidity rates among singleton, twin, and triplet gestations. Prim Care Update Ob Gyns. 1998 Jul 1;5(4):184. doi: 10.1016/s1068-607x(98)00099-7. PMID: 10838344.
- Vasak B, Verhagen JJ, Koenen SV, Koster MP, de Reu PA, Franx A, Nijhuis JG, Bonsel GJ, Visser GH. Lower perinatal mortality in preterm born twins than in singletons: a nationwide study from The Netherlands. Am J Obstet Gynecol. 2017 Feb;216(2):161.e1-161.e9. doi: 10.1016/j.ajog.2016.10.005. Epub 2016 Oct 8. PMID: 27729252.
- Gyamfi-Bannerman C, Gilbert S, Landon MB, Spong CY, Rouse DJ, Varner MW, Meis PJ, Wapner RJ, Sorokin Y, Carpenter M, Peaceman AM, O'Sullivan MJ, Sibai BM, Thorp JM, Ramin SM, Mercer BM; Eunice Kennedy Shriver National Institute of Child Health; Human Development (NICHD) Maternal-Fetal Medicine Units Network (MFMU). Effect of antenatal corticosteroids on respiratory morbidity in singletons after late-preterm birth. Obstet Gynecol. 2012 Mar;119(3):555-9. doi: 10.1097/AOG.0b013e31824758f6. PMID: 22353953; PMCID: PMC3338333.
- Tsuda H, Hirakawa A, Kotani T, Sumigama S, Mano Y, Nakano T, Imai K, Kawabata I, Takahashi Y, Iwagaki S, Kikkawa F. Risk assessment for neonatal RDS/TTN using gestational age and the amniotic lamellar body count in twin pregnancies. Clin Chim Acta. 2015 Dec 7;451(Pt B):301-4. doi: 10.1016/j.cca.2015.10.013. Epub 2015 Oct 20. PMID: 26477481.
- Tsuda H, Kotani T, Nakano T, Imai K, Ushida T, Hirakawa A, Kinoshita F, Takahashi Y, Iwagaki S, Kikkawa F. The rate of neonatal respiratory distress syndrome/transient tachypnea in the newborn and the amniotic lamellar body count in twin pregnancies compared with singleton pregnancies. Clin Chim Acta. 2018 Sep;484:293-297. doi: 10.1016/j.cca.2018.06.015. Epub 2018 Jun 9. PMID: 29894780.
- Cheong-See F, Schuit E, Arroyo-Manzano D, Khalil A, Barrett J, Joseph KS, Asztalos E, Hack K, Lewi L, Lim A, Liem S, Norman JE, Morrison J, Combs CA, Garite TJ, Maurel K, Serra V, Perales A, Rode L, Worda K, Nassar A, Aboulghar M, Rouse D, Thom E, Breathnach F, Nakayama S, Russo FM, Robinson JN, Dodd JM, Newman RB, Bhattacharya S, Tang S, Mol BW, Zamora J, Thilaganathan B, Thangaratinam S; Global Obstetrics Network (GONet) Collaboration. Prospective risk of stillbirth and neonatal complications in twin pregnancies: systematic review and meta-analysis. BMJ. 2016 Sep 6;354:i4353. doi: 10.1136/bmj.i4353. PMID: 27599496; PMCID: PMC5013231.
- Htun ZT, Hairston JC, Gyamfi-Bannerman C, Marasch J, Duarte Ribeiro AP. Antenatal Corticosteroids: Extending the Practice for Late-Preterm and Scheduled Early-Term Deliveries? Children (Basel). 2021 Apr 1;8(4):272. doi: 10.3390/children8040272. PMID: 33916116; PMCID: PMC8066880.
- Vieira LA, Kao YH, Tsevdos DS, Lau YK, Wang Z, Li S, Zheutlin AB, Gross SJ, Stone JL, Dolan SM, Schadt EE, Li L. Late preterm antenatal corticosteroids in singleton and twin gestations: a retrospective cohort study. BMC Pregnancy Childbirth. 2022 Dec 5;22(1):904. doi: 10.1186/s12884-022-05262-1. PMID: 36471280; PMCID: PMC9721054.
- Hong S, Lee SM, Kwak DW, Lee J, Kim SY, Oh JW, Jun JK. Effects of antenatal corticosteroids in twin neonates with late preterm birth (ACTWIN [Antenatal Corticosteroids in TWIN late preterm neonates] trial): study protocol for a randomized controlled trial. BMC pregnancy and childbirth. 2019; 19:1-6h.
- Murray S, MacKay D, Stock S, Pell J, Norman J. Association of Gestational Age at Birth With Risk of Perinatal Mortality and Special Educational Need Among Twins. JAMA Pediatr. 2020 May 1;174(5):437-445. doi: 10.1001/jamapediatrics.2019.6317. PMID: 32150231; PMCID: PMC7063542.
- Khalil A. Unprecedented fall in stillbirth and neonatal death in twins: lessons from the UK. Ultrasound Obstet Gynecol. 2019 Feb;53(2):153-157. doi: 10.1002/uog.20107. PMID: 30152183.