More Information
Submitted: November 30, 2022 | Approved: December 05, 2022 | Published: December 06, 2022
How to cite this article: Khalid S, Abdulla S. Ovarian lymphoma – A rare presentation. Clin J Obstet Gynecol. 2022; 5: 098-100.
DOI: 10.29328/journal.cjog.1001116
Copyright License: © 2022 Khalid S, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Ovarian lymphoma – A rare presentation
Srwa Khalid* and Saman Abdulla
University Kurdistan Hewler, School of Medicine, Iraq
*Address for Correspondence: Srwa Khalid, MBChB, MRCOG, MRCPI, FRCPI, FRCOG, University Kurdistan Hewler, School of Medicine, Iraq. Email: [email protected]
Non-Hodgkin's lymphoma involving the ovaries is unusual and may cause confusion for the clinician since its presentation could resemble other, more frequent tumors. Malignant lymphoid cells may occur in the ovary either as a primary neoplasm or as a secondary manifestation of a disseminated occult or known disease. The most common presenting symptoms or signs of malignant lymphomas involving the ovaries are abdominopelvic pain or mass.
Involvement of the ovary by malignant lymphoma is well known as a late manifestation of disseminated nodal disease, almost always of the non-Hodgkin's type, however, primary ovarian lymphomas are unusual [1]. Primary ovarian Non-Hodgkin's Lymphoma (NHL) accounts for 0.5% of all non-Hodgkin's lymphomas and 1.5% of all ovarian neoplasms [2].
However, contrary to their traditional presentations, we present a unique case of non-Hodgkin's lymphoma involving the ovary presenting with a Fever of Unknown Origin (FUO). Thus, the objective of this case report is to highlight the variable presentation of primary ovarian lymphoma, as is described later, to alert healthcare providers to avoid delayed or misdiagnosis and, thus, prompt treatment.
A 53-year-old nulliparous female presented to the Accident and Emergency department with three weeks history of general malaise, fever and left renal angle discomfort. She presented to her family doctor eight days ago with the same symptoms, urinary tract infection was suspected and she was treated with broad-spectrum antibiotics.
Examination revealed pyrexia of 38C, tachycardia of 120/min and blood pressure of 110/85, BMI of 52. Abdominal examination revealed a soft non-tender abdomen with no evidence of any swelling, organomegaly, or lymphadenopathy. A system review revealed no other significant abnormality.
Initial investigations revealed raised White Cell Count (WCC) of 11.3 and a C-reactive protein (CRP) of 245. Septic screens were performed including blood cultures, Mid-Stream of Urine (MSU) and chest X-ray. She was then commenced on antibiotics against both gram-positive & gram-negative organisms.
However, on the second day of admission the patient’s temperature remained persistently elevated at up to 39.5 C, therefore, for which a third antibiotic (triple antibiotics), was added to her treatment regime. Intriguingly, her septic screens returned as unremarkable.
On the third day of admission, the patient developed nausea, vomiting, and diarrhea and continued to have a spiking temperature of > 39 C. Repeat C-reactive protein (CRP) was 238 but the White Cell Count (WCC) was falling. She remained on triple antibiotics. However, as the stool culture was positive for Clostridium Difficile, antibiotics were discontinued and the patient was commenced on oral Metronidazole. At that time, the provisional diagnosis was a Fever of Unknown Origin (FUO).
Persistent pyrexia promoted further workup which included an ultrasound scan of the pelvis and abdomen, which revealed a complex-looking pelvic mass of uncertain origin; thus, a CT abdomen and pelvis was carried out on the sixth day of admission. This showed an 8 cm complex left ovarian mass, however, there was no evidence of abscess or fluid collection. The above finding promoted further workup in the shape of tumor markers namely, CEA, CA125, Ca19.9, AFP & HCG as well as an MRI of the pelvis (Figure 1). Rheumatoid factor, ANA, ANCA, ENA, C3, C4 and Immunoglobulin were all normal. The Mantoux test was negative.
Figure 1: MRI pelvis showing large left ovarian mass.
Subsequently, on the 7th day, in view of the patient’s age, imaging evidence of ovarian mass, and continuing symptoms, the patient underwent a diagnostic laparoscopy to assess the abdominal and pelvic cavity as well as the ovarian mass and then consider further intervention depending on operative findings.
Diagnostic laparoscopy was performed under general anesthesia which confirmed the same previous imaging findings, namely, a cystic ovarian mass, which was too friable and bled easily on touch to allow any laparoscopic manipulations, therefore, laparoscopy was abandoned in favor of laparotomy and left salpingo-oophorectomy.
The patient’s temperature settled and vital signs normalized shortly postoperatively; she remained afebrile for the rest of her hospital stay and was discharged home on the fifth postoperative day.
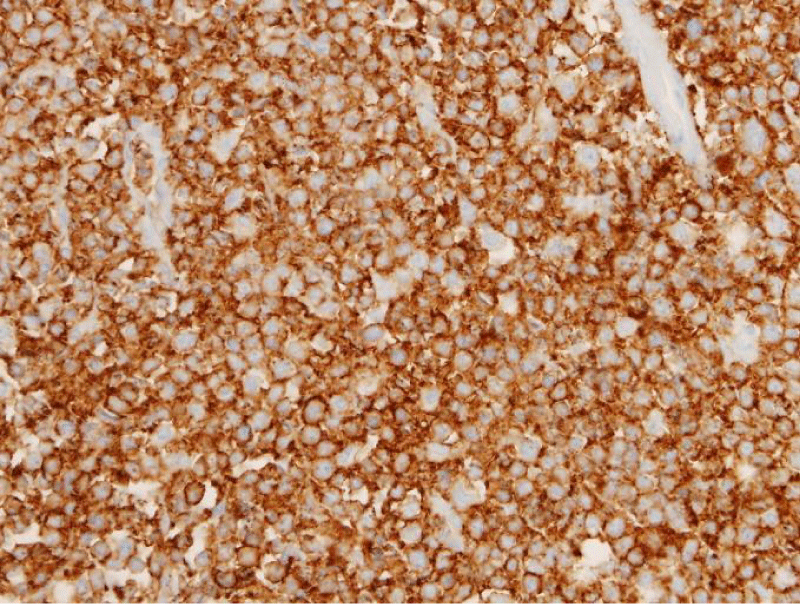
Pathological assessment of the ovary revealed ovarian B cell lymphoma, but no other abnormalities were detected. Further workup with a gynecologist and oncologist team in the shape of bone marrow aspirate, PET scan and CT scan of the chest revealed no further abnormality.
Most Non-Hodgkin’s Lymphomas (NHL) are nodal. Extranodal NHL is frequently encountered in gastrointestinal and other mucosa-associated lymphoid tissues. Although NHL of the ovary is rare, it has been well-reported in the literature. The latter revealed two large case series: one of 42 cases, 1983 (1) and the second of 39 cases including one case of leukemia, 1993 (2). The vast majority of the cases in these series presented with an ovarian mass and most of them were referred with a suspicion of primary or secondary neoplasm [1,2].
Numerous published case reports emphasized that pelvic-related complaints, e.g., pain and/or mass were the commonest clinical presentation [3]. However, some unusual presentation was also reported, for example, some case series reported NHL cases with features suggestive of ovarian cancer, e.g., pelvic mass, pleural effusion and even marked elevation of CA-125 [4,5]. Other cases presented with rare features, e.g., thickened omentum and ascites [6], autoimmune hemolytic anemia which occurs in 3% of NHL [7], abnormal genital bleeding [8], twisted ovarian cyst [9] and menstrual abnormalities [10] have been reported.
In general, true primary ovarian lymphoma usually carries a favorable prognosis [7,11,12], however, other favorable prognostic features should also be considered, e.g.:
1. FIGO stage IA.
2. Unilateral ovarian involvement.
3. Focal involvement of one ovary; and,
4. Follicular (nodular) lymphoma [1].
The main steps in the management are surgery and chemotherapy. The primary disease has better survival than secondary ovarian involvement.
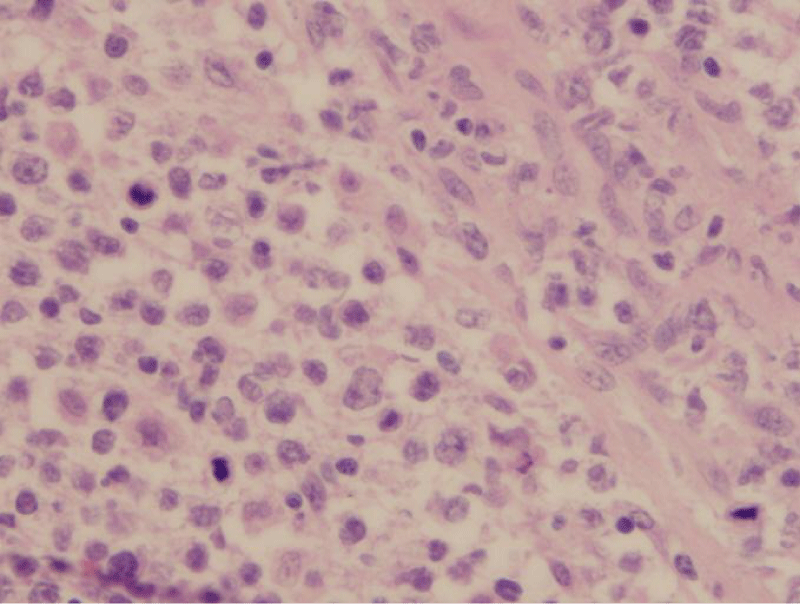
Our case has had a unique presentation and clinical features that have not been previously reported/published. Although lymphomas represent an important cause of FUO, we are not aware of previously published cases of primary ovarian lymphoma presenting with FUO as the primary presentation (Figures 2,3).
Figure 2: Diffuse large cell lymphoma (40x H&E) showing sheets of atypical cells with numerous mitoses.
Figure 3: CD 20 immunostaining showing monoclonal diffuse membranous staining.
Although uncommon, it is advisable to consider ovarian lymphomas in the differential diagnosis of FUO. Moreover, to our knowledge, this is the first case report of primary ovarian lymphoma presenting as FUO. Therefore, we suggest considering primary ovarian lymphoma in the differential diagnosis of FUO in women presenting with a pelvic mass. This would help with prompt diagnosis and is likely to save the patient further intervention, e.g., antibiotic treatment, as well as health care resources by avoiding numerous other diagnostic and treatment modalities.
- Osborne BM, Robboy SJ. Lymphomas or leukemia presenting as ovarian tumors. An analysis of 42 cases. Cancer. 1983 Nov 15;52(10):1933-43. doi: 10.1002/1097-0142(19831115)52:10<1933::aid-cncr2820521026>3.0.co;2-8. PMID: 6627208.
- Monterroso V, Jaffe ES, Merino MJ, Medeiros LJ. Malignant lymphomas involving the ovary. A clinicopathologic analysis of 39 cases. Am J Surg Pathol. 1993 Feb;17(2):154-70. doi: 10.1097/00000478-199302000-00007. PMID: 8422111.
- Vang R, Medeiros LJ, Warnke RA, Higgins JP, Deavers MT. Ovarian non-Hodgkin's lymphoma: a clinicopathologic study of eight primary cases. Mod Pathol. 2001 Nov;14(11):1093-9. doi: 10.1038/modpathol.3880442. PMID: 11706069.
- Perlman S, Ben-Arie A, Feldberg E, Hagay Z. Non-Hodgkin's lymphoma presenting as advanced ovarian cancer-a case report and review of literature. Int J Gynecol Cancer. 2005 May-Jun;15(3):554-7. doi: 10.1111/j.1525-1438.2005.15324.x. PMID: 15882185.
- Weingertner AS, Hamid D, Roedlich MN, Baldauf JJ. Non-Hodgkin malignant lymphoma revealed by an ovarian tumor case report and review of the literature. Gynecol Oncol. 2004 Dec;95(3):750-4. doi: 10.1016/j.ygyno.2004.08.020. PMID: 15581998.
- Yamada T, Iwao N, Kasamatsu H, Mori H. A case of malignant lymphoma of the ovary manifesting like an advanced ovarian cancer. Gynecol Oncol. 2003 Jul;90(1):215-9. doi: 10.1016/s0090-8258(03)00229-4. PMID: 12821369.
- Jung CK, Park JS, Lee EJ, Kim SH, Kwon HC, Kim JS, Roh MS, Yoon SK, Kim KH, Han JY, Kim HJ. Autoimmune hemolytic anemia in a patient with primary ovarian non-Hodgkin's lymphoma. J Korean Med Sci. 2004 Apr;19(2):294-6. doi: 10.3346/jkms.2004.19.2.294. PMID: 15082907; PMCID: PMC2822315.
- Yamane T, Kirimoto K, Fujita M, Naka T, Tsubakio T, Ishikawa K, Nobunaga T, Tanaka F, Yamasaki M. Ovarian involvement as an initial manifestation of malignant lymphoma. Jpn J Clin Oncol. 1989 Jun;19(2):163-6. PMID: 2733170.
- Ng SP, Leong CF, Nurismah MI, Shahila T, Jamil MA. Primary Burkitt lymphoma of the ovary. Med J Malaysia. 2006 Aug;61(3):363-5. PMID: 17240592.
- Konje JC, Otolorin EO, Odukoya OA, Ladipo OA, Ogunniyi J. Burkitts lymphoma of the ovary in Nigerian adults-a 27-year review. Afr J Med Med Sci. 1989 Dec;18(4):301-5. PMID: 2558562.
- Dao AH. Malignant lymphoma of the ovary: report of a case successfully managed with surgery and chemotherapy. Gynecol Oncol. 1998 Jul;70(1):137-40. doi: 10.1006/gyno.1998.5033. PMID: 9698492.
- Scully RE Young RH, Clement PB. Atlas of Tumour Pathology Tumours of the Ovary, Maldeveloped Gonads, Fallopian Tube and Broad Ligament. 3rd ed. AFIP: Washimgton, DC. 1998.