More Information
Submitted: October 25, 2022 | Approved: October 31, 2022 | Published: November 01, 2022
How to cite this article: Tate J, McGrath N, Lalchandani S. Idiopathic ascites following caesarean section: A case report. Clin J Obstet Gynecol. 2022; 5: 093-095.
DOI: 10.29328/journal.cjog.1001114
Copyright License: © 2022 Tate J, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Ascites; Idiopathic; Post-caesarean
Idiopathic ascites following caesarean section: A case report
Jessica Tate*, Niamh McGrath and Savita Lalchandani
Department of Obstetrics & Gynaecology, University Hospital Kerry, V92NX94, Ireland
*Address for Correspondence: Dr. Jessica Tate, Department of Obstetrics & Gynaecology, University Hospital Kerry, V92NX94, Ireland, Email: [email protected]
Ms X is a 40-year-old gravida 12, para 2 + 9 woman, who was admitted for an elective caesarean section at 38 weeks gestation following the previous two caesarean sections. Ms X had abdominal distension and generalised abdominal tenderness in the postoperative period. On investigation, she was found to have an elevated white cell count (WCC), C - Reactive Protein (CRP) and creatinine with free fluid in the abdomen on imaging but there was no evidence of perforation of any visceral organ. Ms X was treated conservatively for sepsis, an Acute Kidney Injury (AKI) and post-operative ileus and her symptoms gradually resolved. This is a case of idiopathic ascites post caesarean delivery with no clear cause.
Ascites are the accumulation of fluid in the peritoneal cavity. There are both benign and malignant aetiologies including liver failure, malignancy, pancreatitis, tuberculous & chylous ascites [1]. It is well reported that rates of the caesarean section have been continuously increasing in recent decades [2]. Caesarean section delivery is known to be associated with complications such as blood loss and damage to adjacent organs intraoperatively such as the bladder, ureters & bowel. Pain, infection and venous thromboembolism can complicate the postoperative period [3]. The objective of this case report is to highlight a rare occurrence of idiopathic ascites following caesarean section as there are very few cases of this reported in the current literature [1].
We present the case of Ms X, a 40-year-old gravida 12 para 2 + 9 woman, who was admitted for an elective caesarean section at 38 weeks gestation. Ms X had two previous caesarean deliveries and would be considered a high-risk obstetric patient due to multiple risk factors highlighted at her booking visit including raised body mass index (BMI) of 32, 9 previous first trimester miscarriages and a history of Intrauterine Growth Restriction (IUGR). Ms X has no other significant past medical or surgical history.
Ms X attended the high-risk antenatal clinic and had an uneventful pregnancy. Of note, there was no history of pre-eclampsia in this pregnancy. She delivered a healthy male infant via elective caesarean section. The surgery was performed without any evident intraoperative complications. The total estimated blood loss was 300 ml.
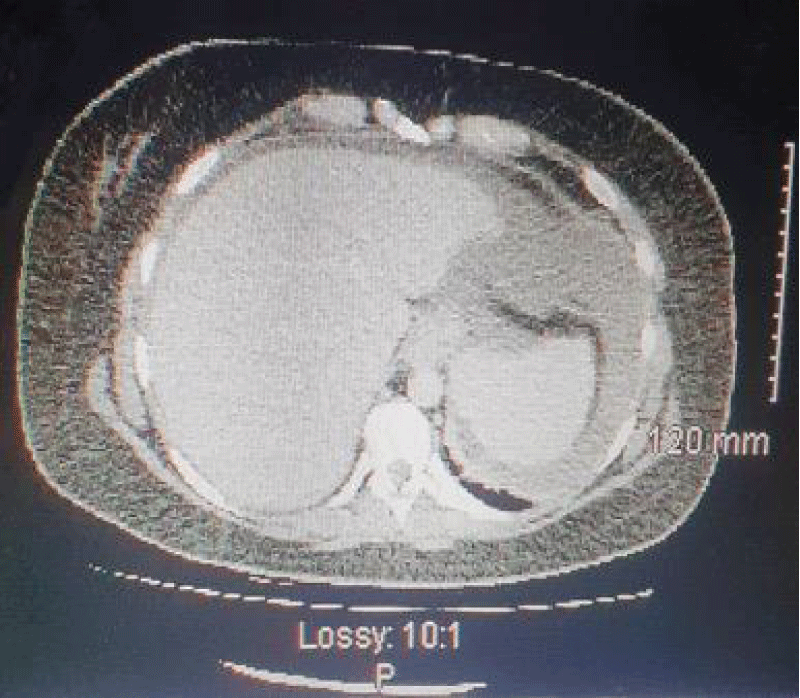
The initial postoperative course was uncomplicated and Ms X was transferred to the postnatal ward where she received routine postoperative analgesia. Within hours of arriving on the ward, Ms X began to complain of lower abdominal pain and mild scar tenderness in keeping with caesarean section delivery. Her urinary output was satisfactory (960 ml over 24 hours). The urinary catheter was removed 24 hours post-procedure. Over the next 24 hours, Ms X developed urinary retention (750 ml seen on bedside bladder ultrasound) requiring re-catheterisation Figure 1.
Figure 1: Free fluid surrounding liver & spleen demonstrated on CT Abdomen-Pelvis.
By day 3 post-delivery, the pain had migrated upwards to the right & left flanks and right upper quadrant (RUQ). The pain was intermittent and crampy and exacerbated by lying flat and mobilising. Urinary output remained > 1 litre/day. At this point, she had not yet passed a bowel movement since the surgery but reported passing flatus. Oral laxatives and a phosphate enema were administered with no effect.
On examination, the abdomen was distended, and soft on palpation with no guarding or rigidity but there was generali-sed abdominal tenderness and it was tympanic on percussion. Vitals were as follows: Blood pressure 134/84 mmHg, Sp02 98% on room air, temperature 37.1 oC, heart rate 92. Her vital signs remained stable throughout her hospitalisation with a maximum recorded temperature of 37.1 oC.
Laboratory investigations revealed a leukocytosis (WCC 16.47 × 109/L) with raised inflammatory markers (CRP 589.6 mg/L), a raised Creatinine (292 mg/dL) and raised urea (11.7 mmol/L) consistent with an acute kidney injury (AKI). Lactate was 0.6 on venous blood gas and liver function tests and electrolytes were within normal ranges. A procalcitonin level was not taken. Haemoglobin pre-operatively was 12.5 g/dL as compared to 11.7 g/dL on day 2 post-operatively. The Hb was stable for the remainder of the admission.
To treat the AKI, Ms X was given intravenous (IV) fluids and the Consultant Microbiologist was contacted who advised her to treat her for sepsis. Initially, Ms X was commenced on IV Co-Amoxiclav. This was later changed to IV Tazocin and IV Gentamicin when her creatinine returned to baseline (88) on the advice of the Consultant Microbiologist as the WCC & CRP remained persistently high (CRP 584.1 mg/L, WCC 15.61 × 109/L) despite receiving 48 hours of Co-Amoxiclav.
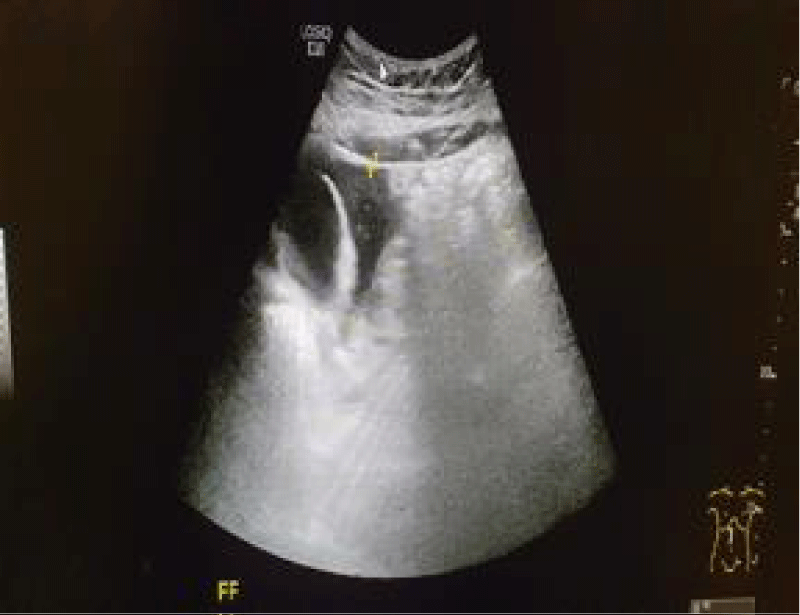
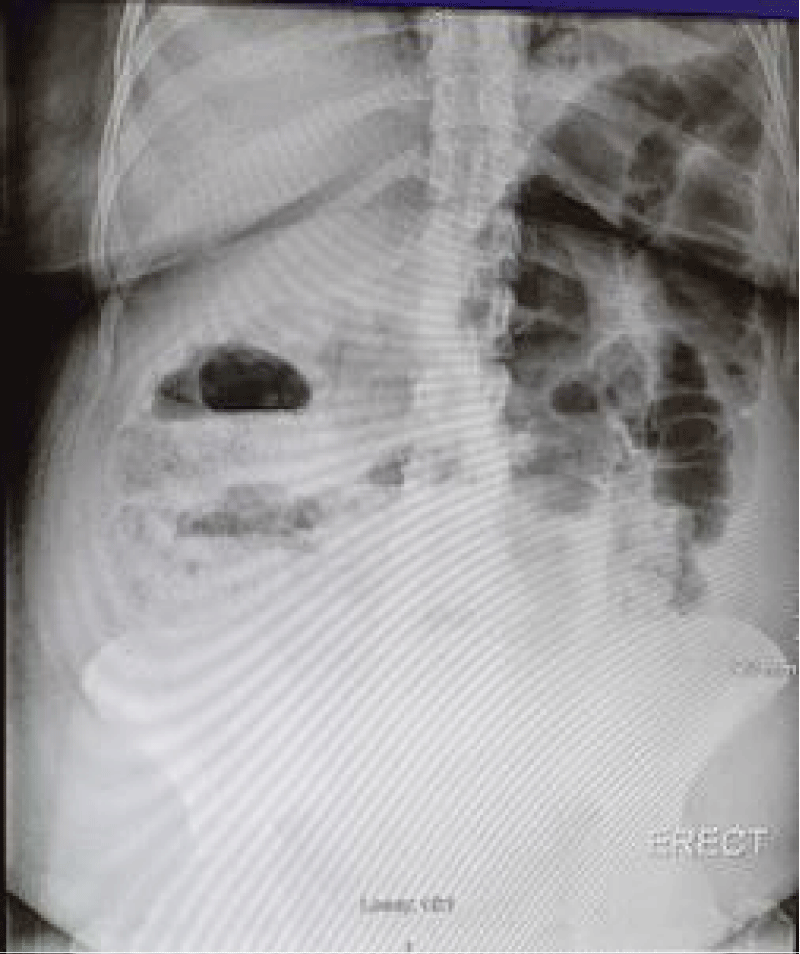
An x-ray of the abdomen was performed to out rule visceral organ perforation. This demonstrated faecal loading in the ascending colon with no evidence of perforation. An ultrasound (US) of the abdomen found a large amount of free fluid surrounding the liver, spleen, right iliac fossa (RIF), left iliac fossa (LIF), right flank & left flank Figure 2. Computed Tomography (CT) of the Abdomen & Pelvis (CT AP) confirmed marked ascites with no signs of hollow organ perforation. An enlarged gallbladder was noted with no evidence of inflammation. The bladder walls appeared intact and there was no sign of mechanical intestinal obstruction.
Figure 2: Free fluid surrounding liver & spleen demonstrated on US Pelvis.
A Consultant General Surgeon examined Ms X and reviewed the above images. A CT Urogram was then performed to further investigate the presence of bladder or ureteric injury as the possible cause of the ascites. The results of the CT urogram further supported the prior imaging and showed no evidence of bladder injury.
Ms X was again reviewed by the surgical team and advised she receive peripheral Total Parenteral Nutrition (TPN) for 48 hours as management of postoperative ileus. After two days she was switched to a light diet and continued on oral laxatives under the advice of hospital Dieticians and General Surgeons (Figure 3).
Figure 3: X-ray Abdomen showing dilated loops of bowel with faecal loading.
Ms X responded well to conservative management with input from obstetricians, general surgeons, radiologists, microbiologists and dieticians. A week after caesarean section delivery she had a bowel movement and the day following this her catheter was taken out. She was discharged 9 days post-delivery with normalised blood test results and a normal US scan of the abdomen. Ms X was followed up closely as an outpatient. At a 6 - week follow-up appointment Ms X reported a complete resolution of her symptoms.
Ascites are the accumulation of fluid in the peritoneal cavity. In this case, there was no evident source of the ascites as the more common causes like vascular, bladder & bowel injuries were ruled out. Radiology showed no evidence of malignancy or pancreatitis. This woman had no history of liver disease and liver function tests were normal. Ms X did not have pre-eclampsia, a condition that has been linked with the finding of ascites during caesarean sections [4]. In addition, there was no history suggestive of underlying tuberculosis.
Bladder injury is an uncommon yet well-known complication of caesarean delivery affecting 1 in every 1000 women [5] and has been linked with the development of urinary ascites. Symptoms of urinary ascites are often non-specific such as abdominal pain or lower back pain with or without evidence of peritonism [6]. Ms X reported RUQ & right flank pain with some lower back pain however both a CT AP and a CT urogram failed to show any evidence of a bladder or ureteric injury to support this as a cause of the visualised ascites.
Chylous ascites are defined as the leakage of lipid-rich lymph into the abdominal cavity [7]. Chylous ascites have occasionally been reported as a post-operative complication and have rarely been associated with pregnancy due to the compression of lymphatics by the gravid uterus or secondary to trauma to the lymphatics sustained during abdominal surgery. In this woman, no ascitic fluid was noted by the surgeons intraoperatively which suggests that Ms X developed ascites post-operatively as uterine involution occurred. Other case reports found that chylous ascites in pregnancy typically resolved with uterine involution and oftentimes there was a clear cause found such as pancreatitis or malignancy. Therefore this is an unlikely mechanism for the development of ascites in our case. One such similar case was in a 27-year-old woman with a BMI of 38.9 where no specific cause could be found yet the ascites resolved with involution of the uterus [8]. According to Thompson, et al. only 6 other cases of chylous ascites post caesarean section delivery have been reported in addition to their case report when they performed a literature review in 2015.
The global incidence rate of Caesarean Sections is rising. In 1990 the global LSCS rate was 7%, this has reached 21% by June 2021 with rates predicted to reach as high as 28.5% globally by 2030 [9]. This is evident across high-income, middle-income & low-income countries. With this, is the need to reallocate resources & ensure adequate counselling of women regarding the risks & potential complications of this operation and its’ potential impact on the future health of both mother & baby.
Post-operative ascites following caesarean section are rarely reported in pregnancy. Ascites has multiple aetiologies including malignancy, liver cirrhosis, intraperitoneal infections and trauma. When ascites post caesarean section is suspected, you must out rule the possibility of iatrogenic injury to the urinary bladder, bowel or blood vessels. In this case, multiple imaging modalities were performed. They failed to demonstrate any of the common causes of ascites. Therefore it is also important to consider less common causes. Paracentesis is a procedure performed to obtain a sample of ascitic fluid for diagnostic or therapeutic purposes [10]. As the ascites were resolving satisfactorily in this case, paracentesis was not performed which meant that no analysis of the ascitic fluid was carried out and therefore no definite cause could be identified.
This case also highlights the importance of involving a Multi-Disciplinary Team (MDT) early in the care of women who develop complex or rare post-operative complications. MDT teams can vary greatly from one maternity hospital to another, however, they often consist of obstetricians, general surgeons, radiologists, microbiologists, midwives, dieticians and internal medicine specialists. MDT management has been shown to maximise patient safety, increase patient satisfaction, improve patient outcomes and positively impact the healthcare team involved in their care [11].
- Sandhu N, Singh S. An unusual case of postoperative ascites after cesarean section. International Journal of Reproduction, Contraception, Obstetrics and Gynecology. 2020 Jun 1;9(6):2635-8.
- Roberts CL, Nippita TA. International caesarean section rates: the rising tide. Lancet Glob Health. 2015 May;3(5):e241-2. doi: 10.1016/S2214-109X(15)70111-7. Epub 2015 Apr 9. PMID: 25866356..
- Dempsey A, Diamond KA, Bonney EA, Myers JE. Caesarean section: techniques and complications. Obstetrics, Gynaecology & Reproductive Medicine. 2017; 1:27(2);37-43.
- Alabrah PW, Agbo J, Agoro ES. Preeclampsia complicated by antenatal & postnatal ascites. European Journal of Medicine & Health Sciences. 2019;1:5.
- Caesarean Section. Consent Advice No. 7, Royal College of Obstetricians & Gynaecologists. Greentop Guidelines. 2009.
- Ko PC, Lo TS, Ashok K. Urinary ascites with elevated blood creatinine following cesarean section indicating bladder injury. Taiwan J Obstet Gynecol. 2011 Dec;50(4):537-9. doi: 10.1016/j.tjog.2011.10.027. PMID: 22212334.
- Al-Busafi SA, Ghali P, Deschênes M, Wong P. Chylous Ascites: Evaluation and Management. ISRN Hepatol. 2014 Feb 3;2014:240473. doi: 10.1155/2014/240473. PMID: 27335837; PMCID: PMC4890871.
- Thompson KA, Al Khabbaz A. Incidental Chylous Ascites at the Time of Cesarean Section. Case Rep Obstet Gynecol. 2015;2015:530210. doi: 10.1155/2015/530210. Epub 2015 Jun 15. PMID: 26171264; PMCID: PMC4485536.
- Betran AP, Ye J, Moller AB, Souza JP, Zhang J. Trends and projections of caesarean section rates: global and regional estimates. BMJ Glob Health. 2021 Jun;6(6):e005671. doi: 10.1136/bmjgh-2021-005671. PMID: 34130991; PMCID: PMC8208001.
- Aponte EM, Katta S, O'Rourke MC. Paracentesis. In: StatPearls. Treasure Island (FL). 2022. https://www.ncbi.nlm.nih.gov/books/NBK435998/
- Epstein NE. Multidisciplinary in-hospital teams improve patient outcomes: A review. Surg Neurol Int. 2014 Aug 28;5(Suppl 7):S295-303. doi: 10.4103/2152-7806.139612. PMID: 25289149; PMCID: PMC4173201.