More Information
Submitted: August 28, 2022 | Approved: September 01, 2022 | Published: September 02, 2022
How to cite this article: Karoui A, Cherif A, Chaffai O, Saidi W, Sahraoui G, et al. Intravenous leiomyomatosis of the uterus: still discovered on anatomopathological examination. Clin J Obstet Gynecol. 2022; 5: 090-092.
DOI: 10.29328/journal.cjog.1001113
Copyright License: © 2022 Karoui A, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Uterus; Intravenous leiomyomatosis; Surgery; Pathology
Abbreviations: LBU: Leiomyomas Beyond the Uterus; IVL: Intravenous Leiomyomatosis; CT: Computed Tomography; MRI: Magnetic Resonance Imaging; IVC: Inferior Vena Cava
Intravenous leiomyomatosis of the uterus: still discovered on anatomopathological examination
Abir Karoui1*, Ahmed Cherif1, Olfa Chaffai1, Wassim Saidi2, Ghada Sahraoui3, Sana Menjli1, Mohamed Badis Chanoufi1, Nadia Boujelbene2 and Hssine Saber Abouda1
1Department of Gynecology, Maternity and Neonatology Center of Tunis, Tunis, Tunisia
2Department of Histology, Salah AzaiezInstitut, Tunisia
3Department of Surgical Oncology, Salah AzaiezInstitut, Tunis, Tunisia
*Address for Correspondence: Abir Karoui, Department of Gynecology, Maternity and Neonatology Center of Tunis, Tunis, Tunisia, Email: [email protected]; [email protected]
Background: Leiomyomas beyond the uterus are defined by benign smooth muscle cell tumors outside of the uterus. Intravenous leiomyomatosis is a rare type of uterine leiomyoma and is characterized by the formation and growth of benign leiomyoma tissue within the vascular wall. Herein, we present a case of Intravenous leiomyomatosis successfully treated by surgical removal and a review of actual medical recommendations.
Case presentation: A 49 - year-old woman, maghrébin, G3 P2, no family history of uterine myomas mentioned, having systemic arterial hypertension, presented to our department with hypogastric pain and abnormal uterine bleeding in the prior five months resulting in anemia which required iron supplementation. On physical examination the vital signs were normal. A palpable mass in the hypogastrium was noted. The rest of the exam was unremarkable. Pelvic ultrasound showed a huge uterus with multiple heterogeneous leiomyomas, including at least one intracavity. Computed tomography scans and magnetic resonance imaging were not done initially due to the unaffordability of the patient. The initial diagnosis was leiomyoma. The decision to perform a total abdominal hysterectomy and bilateral salpingo-oophorectomy was taken. The abdomen was opened by a midline vertical incision. During surgery, multiple subserosal, intramural and submucosal fibroids ranging from 2 cm × 3 cm to 10 cm × 10 cm were seen. On pathological examination, the uterus measured 19 cm in the largest diameter and weighed 1.3 kg. The cut section showed white nodular myometrial masses. Microscopically, intravascular growth of benign smooth muscle cells is found within venous channels lined by endothelium. The diagnosis of Intravenous leiomyomatosis of the uterus without malignant transformation was retained. The patient was monitored for 14 months and subsequent computed tomography did not reveal any evidence of tumor recurrence. The follow-up will be performed annually till the age of menopause.
Conclusion: Intravenous leiomyomatosis is a benign, rare and potentially lethal pathology. It especially affects premenopausal women with a history of uterine myoma, whether operated on or not. They require close and prolonged follow-up because of the high risk of recurrence.
Leiomyomas beyond the uterus (LBU) are defined by benign smooth muscle cell tumors outside of the uterus. Intravenous leiomyomatosis (IVL) is a rare type of uterine leiomyoma and features the formation and growth of benign leiomyoma tissue in the vascular wall. The tumor can grow along blood vessels, extending to the iliac vein, inferior vena cava, and even the heart [1,2]. The incidence of this tumor is about 0.25% to 0.40% of patients who present uterine fibroma [3]. IVL mainly affects pre-menopausal women between the age of 40 and 50 [3].
Pelvic ultrasound is used to show the pelvic mass; computed tomography (CT) and magnetic resonance imaging (MRI) are used to better characterize the mass. Both can specify the origin of the tumor and its site of venous invasion.
The management consists to perform a complete removal of the tumor, including total hysterectomy and bilateral adnexectomy to prevent a recurrence.
Herein, we present a case of IVL successfully treated by surgical removal and a review of actual medical recommendations. The patient provided written informed consent.
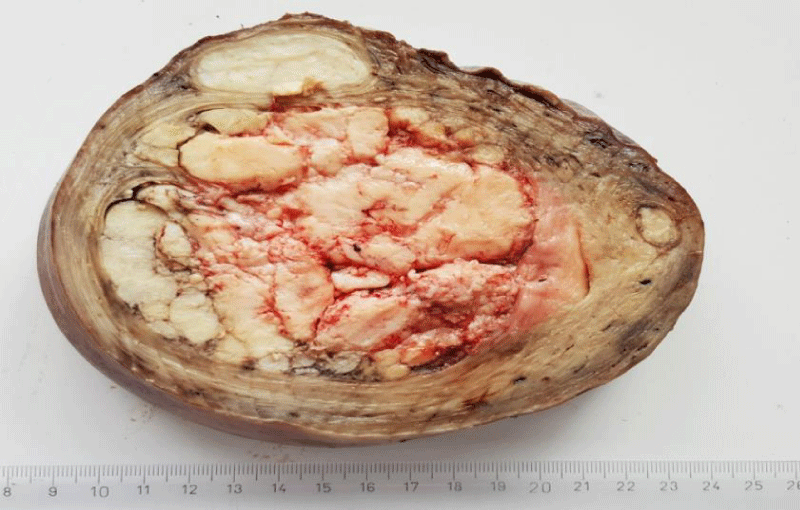
A 49-year-old woman, caucasian, G3 P2, no family history of uterine myomas mentioned, having a history of systemic arterial hypertension presented to our department with hypogastric pain and abnormal uterine bleeding in the prior five months resulting in anemia which required iron supplementation. On physical examination the vital signs were normal. A palpable mass in the hypogastrium was noted. The rest of the exam was unremarkable. Pelvic ultrasound showed a huge uterus with multiple heterogeneous leiomyomas, including at least one intracavity. Computed tomography scan and Magnetic resonance imaging were not done initially due to the unaffordability of the patient. The initial diagnosis was leiomyoma. As the patient was symptomatic and as she had completed their family plan, the decision to perform a total abdominal hysterectomy with bilateral salpingo-oophorectomy was taken. The abdomen was opened by a midline vertical incision. During surgery, multiple subserosal, intramural and submucosal fibroids ranging from 2 cm × 3 cm to 10 cm × 10 cm were seen. On pathological examination, the uterus measured 19 cm in the largest diameter and weighed 1.3 kg. The cut section showed white nodular myometrial masses (Figure 1).
Figure 1: IVL: Multiple white nodular myometrial masses within the myometrium.
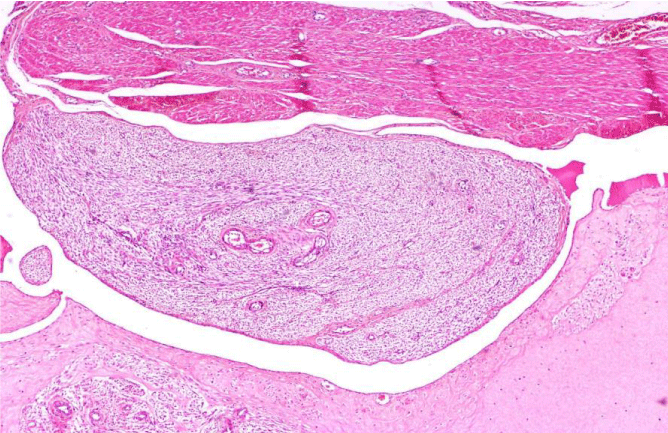
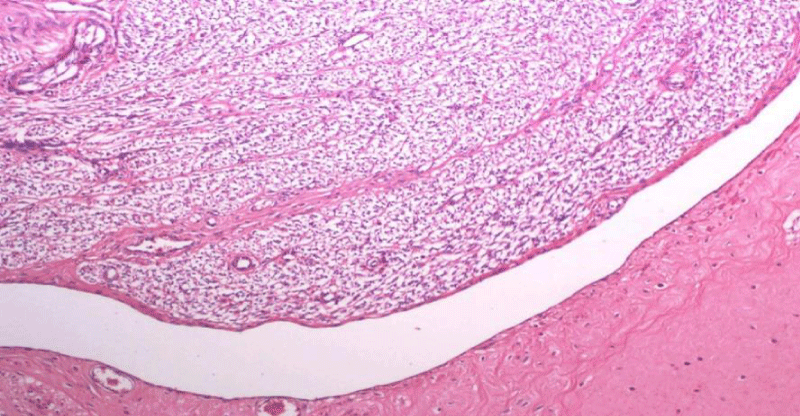
Microscopically, intravascular growth of benign smooth muscle cells is found within venous channels (Figure 2) lined by endothelium (Figure 3).
Figure 2: IVL: Intravenous proliferation of a histologically benign smooth muscle cell tumor mass (HEx20).
Figure 3: IVL: Intravenous leiomyomatosis is found within venous channels lined by endothelium (HEx100).
The diagnosis of IVL of the uterus without malignant transformation was retained. The patient tolerated the treatment with a satisfactory evolution. She was monitored for 14 months and subsequent CT did not reveal any evidence of tumor recurrence. The follow-up will be performed annually till the age of menopause.
Uterine leiomyomas are the most common benign uterine tumors, and the prevalence is about 70% - 80% at the age of 50 [4]. IVL was first described by Hirschfield in 1896 [5]. The precise etiology of IVL is still unclear, although there are 2 hypotheses for the origin of intravenous leiomyomatosis. The first is that the uterine leiomyoma invades the uterine vein and then grows in the venous system. The other hypothesis suggests that the smooth muscle cells of the vein abnormally proliferate in the venous system [6]. However, the latter hypothesis was recently refuted and studies found no endothelial tissue markers (CD10, CD31 and CD34) in IVL tumors [7]. IVL through the uterine vein grows into the internal iliac veins, common iliac veins and inferior vena cava (IVC), and rarely goes to the right atrium, ventricle and pulmonary artery [8]. Sometimes, the ovarian vein provides another way to the subphrenic portion of the IVC [9]. The early diagnosis of IVL is usually difficult. At the early stage of IVL, most of the patients are asymptomatic despite the intravenous extension and the tumor extension remains inside the small vessels of the myometrium and cannot be detected by computed tomography scan or magnetic resonance imaging [10]. The cases of IVL are underestimated because the diagnosis can be missed particularly in the early stage. The preoperative diagnosis of IVL is also difficult because it is usually confirmed by intraoperative findings or postoperative pathologic examination [11]. Clinical manifestations are nonspecific depending on the location and size of the tumor. For example, in the case of a pelvic mass or uterine leiomyoma, patients may either be asymptomatic or complain of abnormal uterine bleeding, pelvic pain and abdominal distension. Regarding the IVC and heart, patients may have symptoms such as chest pain, dyspnea, lower extremity edema and even sudden death [9]. The diagnosis of certainty is based on anatomopathological analysis. The tumor is composed of smooth muscle cells normally present in the uterus. Microscopically, the tumor is positive for desmin and actin. There is also the presence of hormonal receptors for progestins and estrogens. The mitotic analysis reveals a low activity of the cells [12,13]. IVL needs surgical treatment for diagnosis and therapeutic purposes. Complete resection is necessary to prevent a recurrence. Resection should include the uterus, fallopian tubes, ovaries and intravascular tumors. If an extrauterine invasion is present, a multidisciplinary team is needed to ensure a successful surgery. A one or two-stage operation can be considered depending on the general condition of the patient and tumor invasion [14]. The recurrence rate of IVL varies from 16% to 30%. The difference in recurrence rate is due to the difference in surgical methods. Women who have had myomectomy or hysterectomy alone are more likely to recur compared to women who have undergone hysterectomy with bilateral salpingo-oophorectomy [15].
Female steroids have been incriminated in the pathogenesis of this disease. For this reason, several authors have evaluated the efficacy of hormonal therapy in the treatment of the IV as a neoadjuvant for patients with incomplete resection or who do not have surgery. The commonly used agents are gonadotropin-releasing hormone agonists, tamoxifen and medroxyprogesterone [16]. The results of treatment effects vary. Some papers report meaningful responses [2]. In other cases, efficacy has not been demonstrated [2,8]. Since postoperative recurrence of IVL may occur after many years of surgery, long-term follow-up is mandatory and an annual CT examination is recommended [17].
IVL is a benign, rare but potentially lethal pathology. It usually affects premenopausal women with a history of uterine myoma, whether operated on or not. Once the disease is diagnosed, radical resection should be performed. They require close and prolonged follow-up because of the high risk of recurrence.
Declarations
Consent for publication: Written consent was provided by the patient.
- Fasih N, Prasad Shanbhogue AK, Macdonald DB, Fraser-Hill MA, Papadatos D, Kielar AZ, Doherty GP, Walsh C, McInnes M, Atri M. Leiomyomas beyond the uterus: unusual locations, rare manifestations. Radiographics. 2008 Nov-Dec;28(7):1931-48. doi: 10.1148/rg.287085095. PMID: 19001649.
- Clay TD, Dimitriou J, McNally OM, Russell PA, Newcomb AE, Wilson AM. Intravenous leiomyomatosis with intracardiac extension - a review of diagnosis and management with an illustrative case. Surg Oncol. 2013 Sep;22(3):e44-52. doi: 10.1016/j.suronc.2013.03.004. Epub 2013 Apr 30. PMID: 23642379.
- Ma G, Miao Q, Liu X, Zhang C, Liu J, Zheng Y, Shao J, Cheng N, Du S, Hu Z, Ren Z, Sun L. Different surgical strategies of patients with intravenous leiomyomatosis. Medicine (Baltimore). 2016 Sep;95(37):e4902. doi: 10.1097/MD.0000000000004902. PMID: 27631266; PMCID: PMC5402609.
- Baird DD, Dunson DB, Hill MC, Cousins D, Schectman JM. High cumulative incidence of uterine leiomyoma in black and white women: ultrasound evidence. Am J Obstet Gynecol. 2003 Jan;188(1):100-7. doi: 10.1067/mob.2003.99. PMID: 12548202.
- Birch-Hirschfeld FV, Felix V, Johne A, Royal College of Physicians of Edinburgh. Lehrbuch der pathologischenAnatomie. Leipzig: F.C.W. Vogel; 1887; http://archive.org/details/b21925501_0002].
- Diakomanolis E, Elsheikh A, Sotiropoulou M, Voulgaris Z, Vlachos G, Loutradis D, Michalas S. Intravenous leiomyomatosis. Arch Gynecol Obstet. 2003 Feb;267(4):256-7. doi: 10.1007/s00404-002-0443-z. Epub 2002 Nov 13. PMID: 12592433.
- Ma G, Miao Q, Liu X, Zhang C, Liu J, Zheng Y, Shao J, Cheng N, Du S, Hu Z, Ren Z, Sun L. Different surgical strategies of patients with intravenous leiomyomatosis. Medicine (Baltimore). 2016 Sep;95(37):e4902. doi: 10.1097/MD.0000000000004902. PMID: 27631266; PMCID: PMC5402609.
- Wang J, Yang J, Huang H, Li Y, Miao Q, Lu X, Li Y, Yang N, Huang Y, Chen J, Cao D, Wu M, Pan L, Lang J, Shen K. Management of intravenous leiomyomatosis with intracaval and intracardiac extension. Obstet Gynecol. 2012 Dec;120(6):1400-6. doi: 10.1097/aog.0b013e31826ebb90. PMID: 23168766.
- Gunderson CC, Parsons B, Penaroza S, Peyton MD, Landrum LM. Intravenous leiomyomatosis disguised as a large deep vein thrombosis. J Radiol Case Rep. 2016 May 31;10(5):29-35. doi: 10.3941/jrcr.v10i5.2221. PMID: 27761178; PMCID: PMC5065288.
- Douik F, Hsayaoui N, Bettaieb H, Mbarki W, Oueslati H, et al. (2017) Intravenous Leiomyomatosis of the Uterus: A Case Report. ObstetGynecol Cases Rev 4:108. doi.org/10.23937/2377-9004/1410108. https://pdfs.semanticscholar.org/079d/797b9d46d37b5093bb300501e79ca6343087.pdf
- Barksdale J, Abolhoda A, Saremi F. Intravenous leiomyomatosis presenting as acute Budd-Chiari syndrome. J Vasc Surg. 2011 Sep;54(3):860-3. doi: 10.1016/j.jvs.2011.03.261. Epub 2011 May 28. PMID: 21620629.
- Kim YN, Eoh KJ, Lee JY, Nam EJ, Kim S, Kim SW, Kim YT. Aberrant uterine leiomyomas with extrauterine manifestation: intravenous leiomyomatosis and benign metastasizing leiomyomas. Obstet Gynecol Sci. 2018 Jul;61(4):509-519. doi: 10.5468/ogs.2018.61.4.509. Epub 2018 Jun 18. PMID: 30018906; PMCID: PMC6046354.
- Vaquero ME, Magrina JF, Leslie KO. Uterine smooth-muscle tumors with unusual growth patterns. J Minim Invasive Gynecol. 2009 May-Jun;16(3):263-8. doi: 10.1016/j.jmig.2009.01.013. PMID: 19423058.
- He J, Chen ZB, Wang SM, Liu MB, Li ZG, Li HY, Zhao G. Intravenous leiomyomatosis with different surgical approaches: Three case reports. World J Clin Cases. 2019 Feb 6;7(3):347-356. doi: 10.12998/wjcc.v7.i3.347. PMID: 30746376; PMCID: PMC6369390.
- Correia P, Castro A, Rocha A, Freitas D, Carnide C, Moutinho O. Pelvic Intravenous Leiomyomatosis - Case Report. Rev Bras Ginecol Obstet. 2016 Aug;38(8):412-5. doi: 10.1055/s-0036-1588002. Epub 2016 Aug 16. PMID: 27529764.
- He J, Chen ZB, Wang SM, Liu MB, Li ZG, Li HY, Zhao G. Intravenous leiomyomatosis with different surgical approaches: Three case reports. World J Clin Cases. 2019 Feb 6;7(3):347-356. doi: 10.12998/wjcc.v7.i3.347. PMID: 30746376; PMCID: PMC6369390.
- Su Q, Zhang X, Zhang H, Liu Y, Dong Z, Li G, Ding X, Liu Y, Jiang J. Intravenous Leiomyomatosis of the Uterus: A Retrospective Single-Center Study in 14 Cases. Biomed Res Int. 2020 Feb 14;2020:9758302. doi: 10.1155/2020/9758302. PMID: 32337287; PMCID: PMC7155762.