More Information
Submitted: April 11, 2022 | Approved: May 12, 2022 | Published: May 13, 2022
How to cite this article: Merse F, Kelbiso L, Fanta A. Factors associated with utilization of Iron with Folic Acid (IFA) supplement among pregnant women attending antenatal care at government health facilities and family guidance clinic in Hawassa City Administration, Hawassa, Ethiopia. Clin J Obstet Gynecol. 2022; 5: 055-060.
DOI: 10.29328/journal.cjog.1001108
Copyright License: © 2022 Merse F, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Anemia; Iron with folic acid; Compliance; Pregnant; Hawassa city
Abbreviations: ANC: Anti Natal Care; CI: Confidence Interval; CSA: Central Statistical Agency; DHS: Demographic and Health Survey; EDHS: Ethiopian Demographic and Health Survey; FMoH: Federal Ministry of Health; ID: Iron Deficiency; IFA: Iron with Folic Acid; SNNPRS: Southern Nations Nationalities and Peoples Region State; WHO: World Health Organization
Factors associated with utilization of Iron with Folic Acid (IFA) supplement among pregnant women attending antenatal care at government health facilities and family guidance clinic in Hawassa City Administration, Hawassa, Ethiopia
Fekadu Merse1, Lolemo Kelbiso1 and Amanuel Fanta2*
1Nutrition Department, Wolaita Soddo University, Wolaita, Sodo, Ethiopia
2Nursing Department, Hawassa College of Health Sciences, Hawassa, Ethiopia
*Address for Correspondence: Amanuel Fanta, Nursing Department, Hawassa College of Health Sciences, Hawassa, PO Box 84, Hawassa, Ethiopia, Email: [email protected]
Background: Iron deficiency anemia is common during pregnancy since the overall iron requirement is greater than non-pregnant women and is associated with adverse outcomes. Iron deficiency (ID) is a state of insufficient iron to maintain normal physiological functions of tissues and leads to anemia.
Objectives: To assess factors associated with the utilization of Iron with Folic acid supplement Among Pregnant Women Attending Antenatal care at Government Health Facilities and Family Guidance Clinic in Hawassa City, South Ethiopia.
Methods: Institutional-based cross-sectional study design was conducted among 412 health providers who are working at public health institutes in Hawassa city from March to April 2015. Pretested Self-administered questionnaires were used to collect the data. The data was entered into Epi-data and analysed by SPSS version 26.0. Bivariate and multivariate regression analysis was used to see the significant association between the outcome and independent variables. Odds ratios and 95% CI will be computed to measure the strength of the association, p - value of ˂ 0.05 will be considered a statistically significant.
Results: A total of 412 pregnant women who came to attend ANC at least for the second time were interviewed in seven health facilities. Our study showed that 333 (81%, 95% CI: 77.2 - 84.8) pregnant women reported taking IFA supplements and high compliance was 37.7% (95% CI: 32.5 - 42.9). In multivariable analysis, side effects and low acceptance of the supplement were significantly associated with compliance to IFA supplementation (p < 0.05).
Conclusion: There is a relatively better level of compliance towards IFA supplementation compared to other national data. Pregnant women should be counseled regarding how to manage the side effects of IFA supplements during ANC. Further research has to be done on the acceptability of the supplements.
Iron deficiency (ID) is a condition in which there is insufficient iron to support normal physiological activities of tissues, resulting in anemia. Iron and folic acid deficiency anemia is a worldwide public health issue that causes significant maternal morbidity and mortality [1]. Iron deficiency anemia is common during pregnancy because the overall iron requirement is higher than in non-pregnant women and is associated with negative consequences. It is the most common nutritional condition in the world, affecting over 25% of the global population, and it is especially severe in young children and women of reproductive age (Kamau, et al. 2020). It is critical to the socio-economic growth of nations.
Anemia was found in 38.2% of pregnant women worldwide, with Africa accounting for 46.3% (9.2 million). It is the world's most widespread nutritional condition, affecting over 2 billion people. In India, the prevalence of IDA ranges from 38% to 72% depending on age and gender. Because of their cereal-based diet, tribal tribes are thought to have a high prevalence of IDA. The prevalence of anemia in the Indian state of Madhya Pradesh was estimated to be 72.0% among girls aged 12–14 years and 74.8 percent among girls aged 15–17 years (Chakma, et al. 2013). Although IFA supplementation has been a priority program in Nepal since the 1980s, anemia during pregnancy remains a public health issue.
Even though efforts to control and prevent anemia during pregnancy, this public health issue persists in Kenya, with a nationwide prevalence of 55.1%, resulting in an estimated 10% maternal and 20% perinatal mortality. The prevalence is comparable to what has been observed in Asia, where the illness is the second greatest cause of maternal death (Kamau, et al. 2018).
According to the 2019 Ethiopia Demographic and Health Survey report, the national prevalence of anemia during pregnancy is 29.1% [2].
Furthermore, folate is a necessary vitamin in the human body. To avoid anemia, all pregnant women in malnutrition-prone areas should get iron and folic acid (IFA) supplements regularly, along with adequate dietary guidance [3].
Anemia harms women's productivity, immunological function, reproductive failure (miscarriage, stillbirths, prematurity, low birth weight, per-natal mortality), and maternal death during childbirth [4].
Iron supplements are distributed to pregnant women through antenatal care programs. However, the effectiveness of these strategies in lowering maternal anemia has been insufficient [5]. During their most recent pregnancy, 1% of Ethiopian women took iron supplements for the recommended length (90 days or more) [6]. Many nutrition experts feel that one of the main reasons national iron supplementation programs fail is women's refusal to take iron supplements daily due to adverse effects that can arise while taking iron [7].
Recent reviews on the topic suggest that there are several reasons for ineffective programs including sporadic or inadequate supply, poor quality tablets, problems with delivery and distribution systems, poorly trained and uncommitted health providers, ineffective communication materials to promote behavior change, lack of access to or use of prenatal care, and poor monitoring of the problem [8-10].
In Sidama and south regions of Ethiopia, only 27% of women who gave birth in the five years preceding the survey received antenatal care from a skilled provider for their most recent birth and coverage of iron supplementation was 15% [11]. We did not find information on the effective coverage of the IFA women received or purchased in the study. It is also not clear whether women use (ingest) the supplement and the factors associated with compliance in the study area. Thus the purpose of the current study is to assess factors associated with the utilization of Iron with Folic acid supplements among pregnant women attending antenatal care at government health facilities and the Family Guidance clinic in Hawassa city Administration, Ethiopia.
Study setting, design, and period
The study will be conducted at the public health institute in Hawassa city. Hawassa city is surrounded by the shores of Lake Awasa in the Great Rift Valley which is located 273 km (170 mi) far away from Addis Ababa the capital city of Ethiopia. The city serves as the capital of southern nations, nationalities and people region, and the Sidama region. Geographically it is located 130 km from Woliata sodo in the east, 75 km from Dilla in the north, and 22 km from Shashemene in the south, the city is divided into 8 sub-cities and 32 kebeles. Regarding the health infrastructure, there are 6 hospitals, 53 private clinics, and 10 public health centers. There are also government partners owned health facilities of family guidance and Mere stops clinic.
Inclusion and exclusion criteria
Pregnant women who attended antenatal care (ANC) in government hospitals, health centers, and family guidance health facilities at the time of data collection in Hawassa City were included. Pregnant women who were attending antenatal care for the first visit or were very sick were excluded.
Source population
All pregnant women who are permanent residents for the last six months.
Study population
All pregnant women attending antenatal clinics at Hawassa city government hospitals, health centers, and family guidance at the time of data collection.
The sample size was determined by the formula used for the unmatched case-control study using EPI Info 7. Factors like age > 25 years, low socioeconomic status, ANC > 4, and cost of the tablet were used, and a factor giving the largest sample size was used as the final sample size of the study (age > 25 years). Assumptions used to estimate the sample size was the percentage of non-adherents with age > 25 years of 37.3% [12], a minimum detectable odds ratio of 1.836, a level of precision of 5%, a power of 80%, with one-to-one ratio among cases and controls, considering 10% non-response rate and design effect of 1. The final sample size became 412.
Data from the Hawassa city administration health department showed that approximately 550 pregnant women attend antenatal care per month at selected facilities. This was proportionally allocated based on the number of ANC attendants. Accordingly, 90, 85, 63, 56, 52, 34, and 32 women who had at least one prior visit to an ANC during the current pregnancy were recruited. Study participants were recruited by systematic sampling since there are no patterns in their antenatal care (ANC) appointments and random by itself.
Data collection procedure
Data was collected by using face-to--to-face interviews with pre-tested structured questionnaires initially prepared in English and translated to Amharic, and translated back to English by language experts. The independent study variables included were sociodemographic factors, health-seeking behavior and utilization of supplementation services, environmental factors, and medical information. The dependent variable was the utilization of iron-containing supplements. Seven female research assistants who were unemployed and with training in nursing and two supervisors who had a first degree in health and experience in the research were recruited. The questionnaire was pretested on 10% of the sample other than the study area.
Data processing and analysis
The collected data was data analysis done by using Statistical Package for Social sciences (SPSS) version 21.0 statistical software. Descriptive statistics were carried out to summarize the data. The main dependent variable was the compliance rate. Bivariate analysis was done to elicit factors associated with utilization of iron and folic acid supplementation with odds ratio as the measure of association. Factors having a p - value < 0.25 in bivariate analysis were entered in the binary logistic regression model building process because individual variables that are weakly associated with the outcome can contribute significantly when they are combined. A p - value < 0.05 was considered statistically significant.
Operational definition
Compliance was defined as the use of supplements for more than eleven days from last in the previous 15 days preceding the interview date.
Effective coverage of supplements: The number of pregnant women who had received IFA.
High compliance: Among women who were supplemented iron with folic acid in current pregnancy and ingested the tablet for more than eleven days in the last 15 days preceding the interview.
Low compliance: Among women who were supplemented iron with folic acid in current pregnancy and ingested the tablet for eleven or fewer days in the last 15 days preceding the interview.
Ethical considerations
Ethical clearance was obtained from the school of Public health and medical sciences research and ethics committee of Wolaita Sodo University. A formal letter of permission was obtained from administrative bodies of the Hawassa City administration health desk. Finally, verbal consent was requested from every study participant included in the study during data collection time after explaining the objectives of the study. Data is stored in a password-protected computer. All pregnant women who participated in the study and were not supplemented on current pregnancy were linked with the service providers in the facility where they are attending ANC.
Socio-demographic characteristics of study participants
A total of 412 pregnant women were interviewed in seven health facilities. The median age of the respondents was 25 years and about three-fourths (74.2%) were between 20–29 years. About half of the women (52.1%) were protestant religion followers. Nearly all participants (97.8%) were married. About one-third (34.5%) of the respondents were secondary school complete and 47.8% identified themselves as housewives. The median number of children ever born was two. Three hundred thirteen (87.4%) of the women responded their household average monthly income was greater than one thousand birrs (Table 1).
| Table 1: Socio-demographic characteristics of pregnant women attending ANC at government hospitals, health centers, and family guidance health clinic in Hawassa City, South Ethiopia, March 2015. | |||
| Variables | Category | Frequency | percentage |
|
Age (N=411) |
15-19 years | 52 | 12.6 |
| 20-24 years | 138 | 33.5 | |
| 25-29 years | 167 | 40.5 | |
| 30-34 years | 42 | 10.2 | |
| 35-39 years | 12 | 2.9 | |
| 40-44 years | 1 | 0.3 | |
| Children ever born (N=404) |
0 | 198 | 49 |
| 1-2 | 172 | 42.6 | |
| 3-4 | 32 | 7.9 | |
| 5+ | 2 | 0.5 | |
| Marital status (N=412) | Married | 403 | 97.8 |
| Others* | 9 | 2.2 | |
|
Educational level (N=412) |
No formal education | 31 | 7.5 |
| primary | 138 | 33.5 | |
| Secondary completed | 142 | 34.5 | |
| Technical and vocational | 64 | 15.5 | |
| College and above | 37 | 9 | |
| Monthly income in Et. Birr (N=358) | ≤500 Birr(24.55USD) | 5 | 1.4 |
| 500-1000 | 40 | 11.2 | |
| ≥1000 Birr(49.1USD) | 313 | 87.4 | |
| Current occupation (N=412) |
Housewife | 197 | 47.8 |
| Self-employed | 104 | 25.2 | |
| Government employee | 80 | 19.4 | |
| Student | 21 | 5.1 | |
| Others** | 10 | 2.5 | |
| * Single and divorced ** Privet firm employee, Work in other's house, run the family business, work in NGO, Daily laborer |
|||
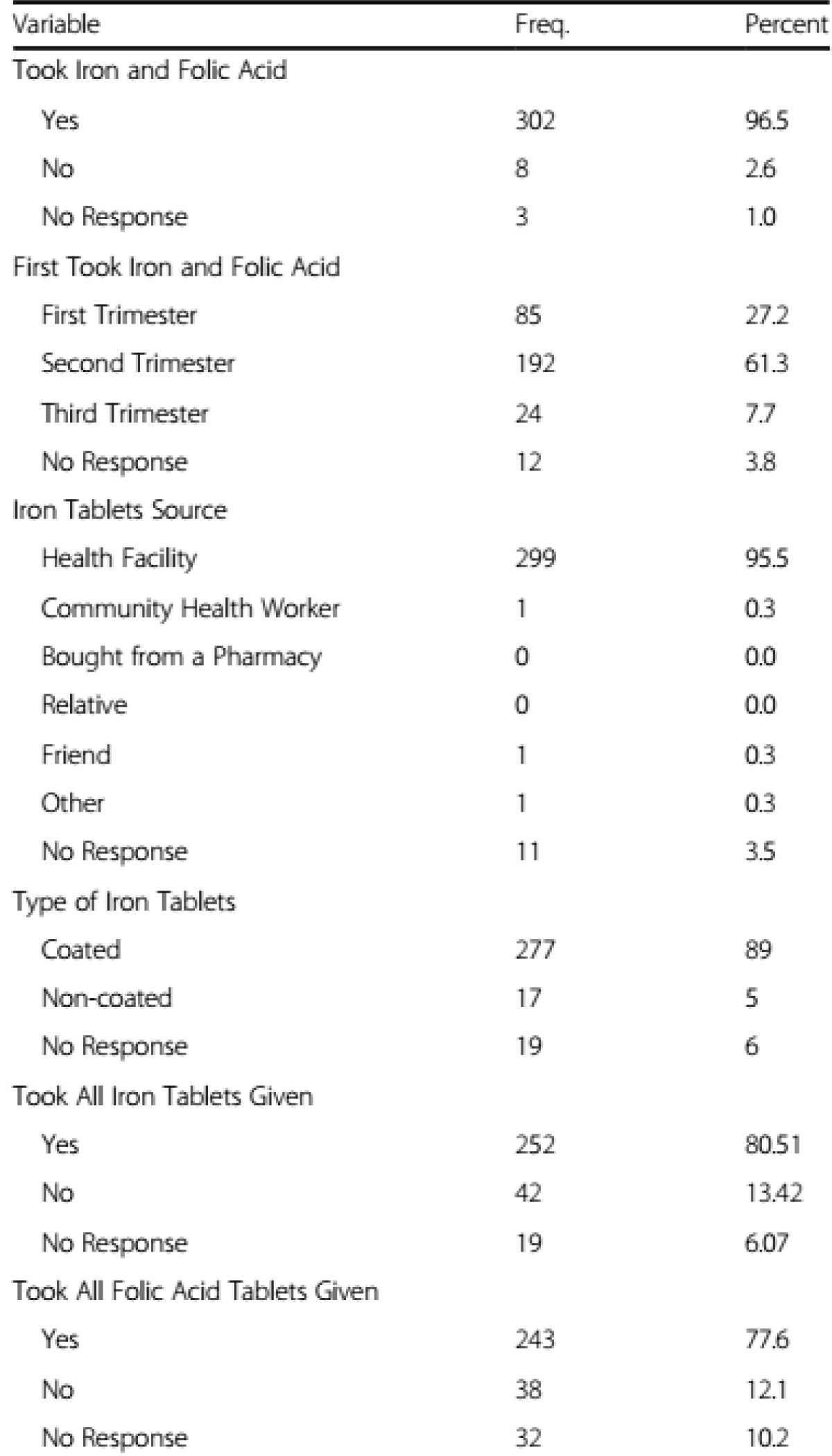
Iron and folic acid effective coverage and compliance (n = 412) (Figure 1)
Factors associated with compliance to iron with folic acid supplementation pregnancy.
Figure 1: Iron and folic acid effective coverage and Compliance (n = 412).
More than one-third (38.43%) of the study population took all the supplements before the survey. Among those who did not take the entire dispensed supplement Side effects (14.11%) are the main reason for not taking the supplement followed by forgetfulness (3.3%) (Table 2).
| Table 2: Reason for missing one or more doses of iron-containing tablets/capsule supplementation among pregnant women attending ANC at government hospitals, health centers, and family guidance clinic in Hawassa City, Ethiopia, March 2015. | ||
| Variable | Frequency | percentage |
| Took Iron and Folic Acid Supplementation (n=412) | ||
| Yes | 333 | 80.8 |
| No | 79 | 18.2 |
| No Response | 4 | 1 |
| Took for Eleven Days or More N=305 | ||
| Yes | 115 | 37.7 |
| No | 190 | 62.3 |
| No Response | 0 | 0 |
| Reason for Not Taking the Supplement (Multiple Response) N=208 | ||
| Took All of the Supplements Dispensed Before the survey | 128 | 38.43 |
| Side Effects | 47 | 14.11 |
| Forgetfulness | 11 | 3.3 |
| I Dislike Taking Drugs | 5 | 1.5 |
| Not knowing the Importance | 5 | 1.5 |
| Others | 12 | 3.6 |
| *Others: Travel lost the supplement, caught other illnesses, get well from anemia, and assumed to have many drugs harm the fetus. | ||
Iron and folic acid effective coverage, compliance, and reason for not taking the supplement
Out of the candidate variables on bivariate analysis having p - value < 0.25, only explaining the poor quality of supplement and side effects showed statistical significance in multivariate analysis (Table 3).
| Table 3: Factors associated with utilization of IFA supplementation among pregnant women attending ANC at government hospitals, health centers, and family guidance clinics in Hawassa City, South Ethiopia, and March 2015. | ||||
| Variables | Low compliance (N=115) | High compliance (N=115) | Crude OR (95%CI) | Adjusted OR (95% CI) |
| Number of ANC visit | ||||
| Second | 56(47.5%) | 54(27.7%) | 2.95(1.63-5.31) | − |
| Third | 37(31.4%) | 70(35.9%) | 1.50(0.82-2.75) | − |
| Fourth and above | 25(21.2%) | 71(36.4%) | 1 | |
| Trimester | ||||
| First | 1(0.9%) | 3(1.6%) | 0.71(0.07-6.90) | − |
| Second | 44(38.3%) | 40(20.9%) | 2.33(1.39-3.89) | − |
| Third | 70(60.9%) | 148(77.5%) | 1 | |
| Ever heard of anemia | ||||
| Yes | 96(81.4%) | 181(92.8%) | 0.34(0.17-0.69) | − |
| No | 22(18.6%) | 14(7.2%) | 1 | |
| Comprehensive Knowledge | ||||
| Yes | 38(32.8%) | 99(52.1%) | 0.45(0.28-0.72) | − |
| No | 78(67.2%) | 91(47.9%) | 1 | |
| Source | ||||
| Government facility (free) | 102(86.4%) | 154(80.6%) | 1.53(0.81-2.90 ) | − |
| Other source | 16(13.6%) | 37(19.4%) | 1 | |
| Side effect | ||||
| Yes | 20(16.9%) | 63(32.6%) | 0.42(0.24 -0.74) | 0.35(0.18-0.68)** |
| No | 98(83.1%) | 130(67.4%) | ||
| Run out of the supplement | ||||
| Yes | 50(42.7%) | 107(55.2%) | 0.61(0.38-0.96) | |
| No | 67(57.3%) | 87(44.8%) | 1 | |
| Stop due to poor quality | 0.42(0.24-0.72) | |||
| Yes | 13(11.4%) | 34(18.7%) | 0.56(0.28-1.11) | |
| No | 101(88.6%) | 148(81.3%) | ||
WHO recommends all pregnant women in areas of anemia prevalence < 40% should routinely receive iron and folic acid supplements, which means ideally taking 180 tablets before delivery [6]. However, our study showed that more than four-fifths (81%) of pregnant women took Iron-containing supplements during the current pregnancy and the compliance was 37.7% (95% CI: 32.5-42.9). Socio-demographic characteristics were not good predictors of compliance, and our findings confirmed this statement [12]. Age of the woman, current marital status, birth order, and income variables did not have a significant effect on high compliance with IFA supplementation. Side effects and low acceptance of the supplement were important predictors of compliance with IFA supplementation (Table 3).
This effective coverage (81%) of the IFA supplementation is high compared to the coverage of mini EDHS 2016 of urban consumption of iron tablets [13] but it is far different than developed countries (Europe and America) which are around 99% [14] This difference may be due to the respondents were from health facility only and the study was carried out in the capital of south nations and the nationality of people region. In addition to that, the longer reference period used in the EDHS might have made it less sensitive to the very recent national level. However, WHO recommends that every pregnant woman has to receive standard doses of iron and folic acid supplements.
Ideally, women should receive iron-containing supple-ments no later than the first trimester of pregnancy as recommended by World Health Organization [15,16]. However, we found that the supplementation initiation was late (4.2 ± 1.3 months) on average during the fourth month of pregnancy but it is earlier than the study done in eight rural districts of Ethiopia 5.6 (± 1.7) and this might be due to early first ANC visit [17]. Early initiation and the total number of supplements consumed during pregnancy have a significant impact on child mortality [1].
According to our study, 37.7% of women have high compliance. This finding is lower than the compliance of 74.9% reported in Ethiopia, 69% in Senegal, and 58.1% in South India [4,5,18]. This might be due to the low compliance of prescribers with the national micronutrient guideline. In addition, various studies use different definitions of compliance with IFA supplementation; hence, a comparison among them is not worthy.
Forget fullness is mentioned by 3.3% of women as a reason for missing one or more doses of iron-containing tablets/capsules. It was found to be 78.8% in another study of compliance with IFA in the Philippines [8] and 48.8% in South India [3], which is lower in this study might better self-care. Further, it can be prevented by the supportive attitude of family members and compliance can be improved by developing an appropriate message and improving communication [9].
Among the enabling factors, side effects and acceptability of iron and folic acid supplement was found to be significantly associated. The side-effect is frequently considered a major obstacle to compliance [5,7,15]. In our study, it was observed that 80.9% of women with low compliance reported side effects as the reason for low compliance. However, in Burma, only 3% of women stated that side effects were the reason they stopped taking iron supplements, while 30% of women in Thailand complained of side effects while taking iron tablets [19]. Studies conducted in the Philippines [4] and Vietnam also concluded likewise. This might be due to the majority of women were not informed about the potential side effects of iron and folic acid supplements and how to minimize them in advance. The study also showed that 14.41% of women not took the supplement due to the poor quality of iron and folic acid tablets. This finding is supported by a study done in India [5].
The limitation of this study is the self-reporting method of measuring compliance over or underestimating compliance. In addition, the cross-sectional nature of the study does not extend to establishing a true cause and effect relationship between complete IFA supplements and associated factors. There were also chances of recall bias among the study subjects regarding the taking of the supplement.
Effective coverage and compliance with IFA supplemen-tation among pregnant women attending ANC at government hospitals, health centers, and family guidance clinics in Hawassa City were relatively high. Compliance is significantly associated with side effects and low acceptance of the supplement due to poor quality.
Declarations
Ethics approval and consent to participate: Ethical clearance was obtained from the School of Public Health and Medical Sciences Research and Ethics committee of Wolaita Sodo University. A formal letter of permission was obtained from the Hawassa City administration health desk for each health facility. Respective health centers officially allowed carrying out the interviews. Finally, verbal consent was secured from each participant before the interview explaining the objectives of the study. Confidentiality was assured by indicating that they are not requested to write their name on the questionnaire and by assuring that their responses will not in any way be linked to them. In addition, they were told that they have the right not to participate and withdraw from the study in between.
We would like to thank Wolaita Sodo University for facilitating the whole project work and the NORHED-SENUPH project for financial support to conduct the study. We are also grateful to the Hawassa city health department, health facilities included in the study, data collectors, and the study participants for delivering information regarding the study.
Authors' contributions
FM carried out IFA utilization and factors associated with IFA utilization among pregnant women attending ANC at government health facilities and family guidance clinic in Hawassa city study by the acquisition of funding, collection of data, general supervision of the research, and made substantial contributions to conception and design, acquisition of data, analysis and interpretation of data, involved in drafting the manuscript and revising it critically for important intellectual content, and gave final approval of the version to be published. LK made substantial contributions to conception and design, acquisition of data involved in drafting the manuscript, and revising it critically for important intellectual content. AF made substantial contributions to the conception and design, analysis, and interpretation of data involved in drafting the manuscript or revising it critically for important intellectual content, and gave final approval of the version to be published.
Availability of data and materials: the spreadsheet data supporting the findings of this is available at the hands of the corresponding author which can be delivered to the journal based on request at any time.
Consent for publication: We agree to the terms and policies of the editorial office of the journal.
- Simuyemba MC, Bwembya PA, Chola M, Michelo C. A root cause analysis of sub-optimal uptake and compliance to iron and folic acid supplementation in pregnancy in 7 districts of Zambia. BMC Pregnancy Childbirth. 2020 Jan 6;20(1):20. doi: 10.1186/s12884-019-2700-1. PMID: 31906880; PMCID: PMC6945660.
- Ethiopian Public Health Institute Addis Ababa. Ethiopia Mini Demographic And Health Survey. Federal Democratic Republic Of Ethiopia Ethiopia, 2019 July.
- Fite MB, Roba KT, Oljira L, Tura AK, Yadeta TA. Compliance with Iron and Folic Acid Supplementation (IFAS) and associated factors among pregnant women in Sub-Saharan Africa: A systematic review and meta-analysis. PLoS One. 2021 Apr 14;16(4):e0249789. doi: 10.1371/journal.pone.0249789. PMID: 33852614; PMCID: PMC8046188.
- Felipe-Dimog EB, Yu CH, Ho CH, Liang FW. Factors Influencing the Compliance of Pregnant Women with Iron and Folic Acid Supplementation in the Philippines: 2017 Philippine Demographic and Health Survey Analysis. Nutrients. 2021 Aug 31;13(9):3060. doi: 10.3390/nu13093060. PMID: 34578937; PMCID: PMC8468511.
- Pathirathna ML, Wimalasiri KMS, Sekijima K, Sadakata M. Maternal Compliance to Recommended Iron and Folic Acid Supplementation in Pregnancy, Sri Lanka: A Hospital-Based Cross-Sectional Study. Nutrients. 2020 Oct 25;12(11):3266. doi: 10.3390/nu12113266. PMID: 33113819; PMCID: PMC7694027.
- Desta M, Kassie B, Chanie H, Mulugeta H, Yirga T, Temesgen H, Leshargie CT, Merkeb Y. Adherence of iron and folic acid supplementation and determinants among pregnant women in Ethiopia: a systematic review and meta-analysis. Reprod Health. 2019 Dec 21;16(1):182. doi: 10.1186/s12978-019-0848-9. PMID: 31864397; PMCID: PMC6925441.
- Ba DM, Ssentongo P, Kjerulff KH, Na M, Liu G, Gao X, Du P. Adherence to Iron Supplementation in 22 Sub-Saharan African Countries and Associated Factors among Pregnant Women: A Large Population-Based Study. Curr Dev Nutr. 2019 Oct 21;3(12):nzz120. doi: 10.1093/cdn/nzz120. PMID: 31777771; PMCID: PMC6867960.
- Means RT. Iron Deficiency and Iron Deficiency Anemia: Implications and Impact in Pregnancy, Fetal Development, and Early Childhood Parameters. Nutrients. 2020 Feb 11;12(2):447. doi: 10.3390/nu12020447. PMID: 32053933; PMCID: PMC7071168.
- Deori TJ, Ramaswamy G, Jaiswal A, Loganathan V, Kumar R, Mahey R, Yadav K, Kant S. Compliance with iron folic acid (IFA) tablets and associated factors among pregnant women attending ante-natal care clinic at Sub District Hospital, Ballabgarh. J Family Med Prim Care. 2021 May;10(5):2006-2011. doi: 10.4103/jfmpc.jfmpc_1742_20. Epub 2021 May 31. PMID: 34195139; PMCID: PMC8208205.
- Debi S, Basu G, Mondal R, Chakrabarti S, Roy SK, Ghosh S. Compliance to iron-folic-acid supplementation and associated factors among pregnant women: A cross-sectional survey in a district of West Bengal, India. J Family Med Prim Care. 2020 Jul 30;9(7):3613-3618. doi: 10.4103/jfmpc.jfmpc_392_20. Erratum in: J Family Med Prim Care. 2020 Aug 25;9(8):4504. PMID: 33102338; PMCID: PMC7567271.
- Kassa ZY, Awraris T, Daba AK, Tenaw Z. Compliance with iron folic acid and associated factors among pregnant women through pill count in Hawassa city, South Ethiopia: A community based cross-sectional study. Reproductive Health. 2019;16(1). https://doi.org/10.1186/s12978-019-0679-8
- Tesfaye TS, Tessema F, Jarso H. Prevalence of Anemia and Associated Factors Among "Apparently Healthy" Urban and Rural Residents in Ethiopia: A Comparative Cross-Sectional Study. J Blood Med. 2020 Mar 11;11:89-96. doi: 10.2147/JBM.S239988. PMID: 32210654; PMCID: PMC7073428.
- DHS. Federal Democratic Republic Of Ethiopia Demographic And Health Survey. 2016.
- Marx JJ. Iron deficiency in developed countries: prevalence, influence of lifestyle factors and hazards of prevention. Eur J Clin Nutr. 1997 Aug;51(8):491-4. doi: 10.1038/sj.ejcn.1600440. PMID: 11248872.
- Moshi FV, Millanzi WC, Mwampagatwa I. Factors Associated With Uptake of Iron Supplement During Pregnancy Among Women of Reproductive Age in Tanzania: an Analysis of Data From the 2015 to 2016 Tanzania Demographic and Health Survey and Malaria Indicators Survey. Front Public Health. 2021 Jul 14;9:604058. doi: 10.3389/fpubh.2021.604058. PMID: 34336749; PMCID: PMC8316680.
- Fouelifack FY, Sama JD, Sone CE. Assessment of adherence to iron supplementation among pregnant women in the Yaounde gynaeco-obstetric and paediatric hospital. Pan Afr Med J. 2019 Dec 26;34:211. doi: 10.11604/pamj.2019.34.211.16446. PMID: 32201546; PMCID: PMC7065651.
- Mithra P, Unnikrishnan B, Rekha T, Nithin K, Mohan K, Kulkarni V, Holla R, Agarwal D. Compliance with iron-folic acid (IFA) therapy among pregnant women in an urban area of south India. Afr Health Sci. 2014 Mar;14(1):255-60. doi: 10.4314/ahs.v14i1.39. PMID: 26060488; PMCID: PMC4449048.
- Srivastava R, Kant S, Singh A, Saxena R, Yadav K, Pandav C. Effect of iron and folic acid tablet versus capsule formulation on treatment compliance and iron status among pregnant women: A randomized controlled trial. J Family Med Primary Care. 2019;8(2):378. https://doi.org/10.4103/jfmpc.jfmpc_339_18
- Charoenlarp P, Dhanamitta S, Kaewvichit R, Silprasert A, Suwanaradd C, Na-Nakorn S, Prawatmuang P, Vatanavicharn S, Nutcharas U, Pootrakul P, et al. A WHO collaborative study on iron supplementation in Burma and in Thailand. Am J Clin Nutr. 1988 Feb;47(2):280-97. doi: 10.1093/ajcn/47.2.280. PMID: 2963533.