More Information
Submitted: March 24, 2022 | Approved: April 20, 2022 | Published: April 21, 2022
How to cite this article: Mekonnen A, Shewangizaw Z. Timely initiation of breastfeeding and associated factors among mothers with vaginal and cesarean deliveries in public hospitals of Addis Ababa, Ethiopia. Clin J Obstet Gynecol. 2022; 5: 044-050.
DOI: 10.29328/journal.cjog.1001106
Copyright License: © 2022 Mekonnen A, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Timely initiation; Early initiation; Breastfeeding; Cesarean delivery; Vaginal delivery
Timely initiation of breastfeeding and associated factors among mothers with vaginal and cesarean deliveries in public hospitals of Addis Ababa, Ethiopia
Adane Mekonnen1* and Zewdu Shewangizaw2
and Zewdu Shewangizaw2
1Department of Public Health Nutrition, Kotebe Metropolitan University, Menilik II Health, and Medical Science College, Addis Ababa, Ethiopia
2Academic, Research and Training Vice-dean, Kotebe Metropolitan University, Menilik II Health, and Medical Science College, Addis Ababa, Ethiopia
*Address for Correspondence: Adane Mekonnen, Department of Public Health Nutrition, Kotebe Metropolitan University, Menilik II Health, and Medical Science College, Addis Ababa, Ethiopia, Email: [email protected]
Background: WHO and UNICEF recommend breastfeeding to be initiated within an hour of birth. However, timely initiation of breastfeeding remains low in Ethiopia. Therefore, this study aimed to compare the timely initiation of breastfeeding and associated factors with cesarean and vaginal deliveries in public hospitals in Addis Ababa, 2021.
Methods and materials: Comparative cross-sectional study was conducted from January 2021 to February 2021 in public hospitals of Addis Ababa. 322 mothers within three days of delivery at the postnatal ward of the respective public hospitals were selected. A multi-stage sampling method was employed with the final participants being recruited by systematic random sampling. Data was entered to Epi data Version 4.6 and analysis was performed by SPSS Version 26. A Binary and multivariate logistic regression statistical model was used. Adjusted odds ratio with 95% CI was computed to see the strength of association.
Result: Timely breastfeeding initiation was 79 (51.2%) and 123 (80%) for cesarean and vaginal deliveries. With a vaginal delivery, pre-lacteal feeding (AOR = 5.50, 95% CI: 1.83 - 16.57) was significantly associated with timely initiation of breastfeeding. Multiparity (AOR = 2.14, 95% CI: 1.02 - 4.50), support from health care workers (AOR = 2.602, 95% CI: 1.16 - 5.82), and pre-lacteal feeding (AOR = 2.55, 95% CI: 1.13 - 5.75) were significantly associated with timely initiation of breastfeeding with cesarean delivery.
Conclusion: The rate of timely initiation of breastfeeding differs according to the mode of delivery. Cesarean delivery, as compared to vaginal delivery, was associated with a lower rate of timely initiation of breastfeeding.
Breast milk is the ideal food for the infant. It contains all the energy and nutrients in optimal amounts the infant requires [1]. The recent World Health Organization reviews of the short and long-term benefits of breastfeeding concluded that there is strong evidence for many public health benefits of breastfeeding [2]. The benefits for the infant include improved cognitive development, decreased rate of necrotizing enterocolitis, common childhood infections, and decreased risk of sudden infant death syndrome [2-4]. Breastfeeding helps the mother to return to pre-pregnancy weight and improves birth spacing. Additionally, it is important in decreasing rates of chronic illnesses, ovarian and breast cancer [4]. Timely initiation of breastfeeding (TIBF) is defined as breastfeeding within an hour of birth for mothers with vaginal delivery (VD) and Cesarean delivery (CD) with spinal anesthesia; if general anesthesia was used for the procedure, it is defined as the initiation of breastfeeding as soon as the mother regains consciousness [5]. Breastfeeding initiation is a simple intervention that has the potential to significantly improve neonatal outcomes and should be universally recommended [6]. TIBF, by reducing mortality risk, is beneficial for child survival within the first 28 days of birth, including all causes of mortality [7-9]. It also reduces neonatal hypothermia and fosters attachment and bonding through close contact with the mother [10].
Several factors related to the mother and the baby affect the initiation of breastfeeding. Mode of delivery is one of these factors [11-19]. When delivery takes place by cesarean section, the mother becomes a surgical patient with all the inherent risks and problems. Mothers with cesarean section have to cope with having surgery just as they are also trying to care for their newborn children [20]. Cesarean delivery is known to affect the normal physiology of labor and the process that comes after delivery [21-23]. Delayed skin-to-skin contact, fatigue, postoperative pain, and anesthetic drugs may lead to delayed initiation of breastfeeding [21-25]. On the other hand, mothers with a vaginal delivery are devoid of the deleterious effects of surgery and anesthetic drugs on breastfeeding initiation. Other factors identified from a literature review with both delivery modalities include age, educational status, residence, place of birth, employment status, socio-economic status, knowledge of breastfeeding, ANC, infant sex, colostrum, and pre-lacteal feeding status, access to media, parity, counseling on breastfeeding, and singleton births [19,20,27-37].
Globally more than 80% of neonates receive breast milk in nearly all countries, however only about half of them begin breastfeeding within an hour of life [37]. In Africa, TIBF varies regionally. It is 35% in North Africa, 65% in Eastern, and Southern Africa, and 40% in West and Central Africa [38]. In Ethiopia, the national prevalence of timely initiation of breastfeeding is 73% with the lowest prevalence in afar regional state (42%) and the highest prevalence in Diredawa city administration (90.5%) [39]. When the mode of delivery is taken into account, the rate of TIBF varies globally, regionally, and nationally. Globally the TIBF for CD and VD is 33.9% and 64.2% respectively [40]. The prevalence of timely initiation of breastfeeding among cesarean delivered mothers ranged from 16.4% to 85.4% across the 33 sub-Saharan African countries with one-third of these countries having a prevalence of less than 50% [17]. With the vaginal mode of delivery, the rate of timely initiation of breastfeeding is 35.1% in Nigeria [41], 78.8% in Malawi [18], and 84.4% in Namibia [35]. In Ethiopia, the trend from 2000 to 2016 EDHS showed that only 38.8% of mothers with cesarean delivery and 61.5% with vaginal delivery initiated breastfeeding [14].
The Ethiopian Ministry of Health had a plan to increase the proportion of newborns to start breastfeeding within the first hour of life to 92% by 2015 as one strategy to improve child health [42]. Despite the plan data from EDHS 2016 showed that the national rate is 67.5% and which is well below the plan [39]. Studies have indicated that it is possible, successful, and feasible to breastfeed within an hour of birth after a CD [29,43]. A quality improvement approach alone has shown to increase the rate of TIBF from 0% to 93% and interventions to improve breastfeeding initiation rates following CD can improve overall breastfeeding rates [23,43]. Despite this, comparative studies on the TIBF with regards to the mode of delivery in the Ethiopian context are lacking and therefore this study will compare the timely initiation of breastfeeding and associated factors among mothers with cesarean and vaginal deliveries in public hospitals of Addis Ababa, Ethiopia.
Study setting, design and period
A comparative cross-sectional study design was conducted in Addis Ababa from January to February 2021. Addis Ababa is the largest and the capital city of Ethiopia. According to data from the Addis Ababa city administration health bureau 12 public hospitals provide both cesarean and vaginal deliveries.
Inclusion and exclusion criteria
The respondents included in this study were mothers with either cesarean or vaginal delivery who had Antenatal care (ANC) follow up in the same hospital and attended the post-natal ward of selected public hospitals during the study period. Mothers who were critically ill and/or with neonates having gross congenital anomalies that can affect breastfeeding initiation were excluded.
Sample size determination and sampling procedure
The sample size was calculated using the double population proportion formula. The following assumptions were made to determine the required sample size: desired precision (d) = 5%, Confidence level = 95% (Zα/2 = ± 1.96 value), power (β) = 80% ,the prevalence of TIBF with VD was 75% [44], and the prevalence of TIBF with CD was 56.2% [27]. Hence the final sample size with a 10% non-response rate and a design effect of 1.5 was 322. Accordingly, equal proportions of mothers were employed from both delivery modalities. 12 public hospitals provide both cesarean and vaginal deliveries. A multi-stage sampling procedure was employed to recruit final study participants. To make the samples representative 30% of the public hospitals were selected by simple random sampling technique. As a result, Gandhi Memorial hospital, Zewditu Memorial hospital, Ras Desta Damtew hospital, and Dagmawi Menelik referral hospital were selected. Data from the Addis Ababa city administration health bureau showed that a total of 6623 mothers were expected to give birth in the two-month data collection period. This was proportionally allocated based on the number of deliveries. Study participants were finally recruited by systematic random sampling from the respective post-natal ward of the hospitals.
Data collection tool & assurance
The interviewer-administered face-to-face structured questionnaire was used for data collection which was adapted from previous works of literature. The study tool contained five parts with 40 items for CD and 39 items for VD. The data was collected by midwives and nurses after explaining the purpose of the study. Continuous follow-up and supervision were made by a facilitator and Principal Investigators (PI) throughout the data collection period. The data was checked daily for completeness and consistency throughout the data collection period by the facilitator and PI. A unique code was given to each questionnaire. Before commencing the data collection, a pre-test was conducted on 5% of the total sample size at Tirunesh Bejing hospital. The participants recommended no change be made to the questionnaire. The facilitator and data collectors attended training about the objective of the study and the contents of the questionnaire for a one-day duration.
Study variables
Dependent variable: Timely initiation of breastfeeding. In this study, first, the time elapsed for initial breastfeeding after delivery was asked and then it was categorized as a mother who initiated in less than or equal to an hour after delivery or not.
Independent variables: The independent variables were socio-demographic characteristics (age, marital status, Mothers and spouse/partners' educational level, employment status, Infant sex, and income level), Obstetric and healthcare-related factors (Parity, ANC, health care provider support, previous obstetric history, and labor history), traditional belief factors (colostrum avoidance, pre-lacteal feeding, and family support), and awareness related factors (awareness on TIBF & colostrum).
Operational definitions: Timely initiation of breastfeeding: putting the newborn on the mother’s breast to suckle within one hour of birth with VD and CD (if spinal anesthesia is used) or putting the newborn on the mother’s breast to suckle as soon as consciousness is regained with CD (if general anesthesia used) as reported by the mother.
Health care provider support: health care professionals, who counsel and assist the mother for proper attachment and positioning to initiate breastfeeding within one hour of birth.
Pre-lacteal feeding: feeding an infant with something other than breast milk after birth to three days.
Good awareness about the timely initiation of breastfeeding: If the mother can answer five or more questions asked to measure awareness of the timely initiation of breastfeeding.
Poor awareness about the timely initiation of breastfeeding: If the mother answers less than five questions asked to measure awareness of the timely initiation of breastfeeding.
Data processing and analysis
All the questionnaires were checked for completeness, coded, and entered into EpiData version 4.6 and then exported to SPSS version 26 for data analysis. The descriptive statistics were presented in the form of a figure, tables, and text using frequencies and numerical summary statistics such as mean and median. Variables in the bivariate analysis with a p - value ≤ 0.25 were further considered in the final logistic regression analysis. The degree of association between independent and dependent variables was assessed by using an adjusted odds ratio at a 95% confidence interval.
Ethical consideration
Ethical clearance was obtained from Addis Ababa public health research and emergency management directorate and the Ethical Committee of Kotebe Metropolitan University Menelik II Medical and Health Science College. A formal letter was submitted to the public health hospitals. Data collection was conducted after receiving written consent from the participants following an adequate explanation of the purpose of the study.
Socio-demographic characteristics
A total of 322 mothers with vaginal or cesarean delivery at the postnatal ward of selected public hospitals in Addis Ababa, Ethiopia were interviewed with a response rate of 307 (95.3%). The mean age of respondents with cesarean delivery was 31.2 years (95% CI = 30.6 - 31.8) and 30.4 years (95% CI = 30.0 - 30.8) with vaginal delivery. Other results of the socio-demographic characteristics are shown in Table 1.
| Table 1: Socio-demographic characteristics of study participants. | ||||
| Variables | Category | CD (n = 154) |
VD (n = 153) |
Total (n = 307) |
| Maternal age | 15-19 | 5 (3.2%) | 8 (5.2%) | 13 (4.2%) |
| 20-24 | 36 (23.4%) | 25 (16.9%) | 61(19.8%) | |
| 25-29 | 62 (40.3%) | 63 (40.9%) | 125 (40.7%) | |
| 30-34 | 35 (22.7%) | 33 (21.4%) | 68 (22.1%) | |
| ≥ 35 | 16 (10.4%) | 24 (15.6%) | 40 (13%) | |
| Educational level | Primary education | 49 (31.8%) | 55 (36.4%) | 104 (33.8%) |
| Secondary education | 49 (31.8%) | 53 (34.4%) | 102 (33.2%) | |
| Higher/Technical education | 35 (22.7%) | 29 (18.8%) | 64 (20.8%) | |
| No education | 21 (13.6%) | 16 (10.4%) | 37 (12%) | |
| Marital status | In union | 145 (94.2%) | 138 (90.3%) | 283 (92.1%) |
| Not in uniona | 9 (5.8%) | 15 (9.7%) | 24 (7.8%) | |
| Spouse/partner educational level | Primary education | 51 (35.2%) | 42 (27.3%) | 93 (32.8%) |
| Secondary education | 35 (22.7%) | 55 (36.4%) | 90 (31.8%) | |
| Higher/Technical education | 49 (31.8%) | 36 (23.4%) | 85 (30%) | |
| No education | 10 (6.5%) | 5 (3.2%) | 15 (5.3%) | |
| Newborns sex | Male | 86 (55.8%) | 77 (50.6%) | 168 (53%) |
| Female | 68 (44.2%) | 76 (49.4%) | 144 (46.9%) | |
| Occupation | Currently employed | 79 (51.3%) | 50 (32.5%) | 129 (42%) |
| Currently unemployed | 75 (48.7%) | 103 (67.5%) | 178 (57.9%) | |
| Monthly income | <5000 | 59 (38.3%) | 53 (34.9%) | 112 (36.5%) |
| 5000-10000 | 55 (35.7%) | 53 (34.9%) | 108 (35.2%) | |
| >10000 | 40 (26%) | 47 (30.3%) | 87 (28.3%) | |
| asingle, divorced, widowed, cohabited or separated. | ||||
Timely initiation of breastfeeding
Timely initiation of breastfeeding regardless of the method of delivery was 204 (66.5%). With CD, 79 (51.2%) initiated breastfeeding within an hour of birth whereas 123 (80%) with VD initiated timely. The reasons stated for delayed initiation of breastfeeding by mothers with CD were the effect of anesthesia 25 (33.3%), lack of assistance 20 (26.6%), baby sickness 15 (20%), inadequate breast milk 8 (10.6%), and maternal sickness 7 (9.3%). Respondents with VD identified baby sickness 14 (46.6%), maternal sickness 6 (20%), inadequate breast milk 6 (20%), and lack of assistance 4 (13.3%) as a cause for delaying breastfeeding initiation. The mean and median time for vaginal delivery was 90.3 minutes (95% CI = 26.56 - 154.03) and 30 min respectively. For cesarean delivery, the meantime was 414.57 minutes (95% CI 261.13 - 568.00) whereas the median time was 60 minutes.
Obstetric and healthcare-related factors
With both delivery methods, ANC coverage was high. Other obstetric and healthcare-related characteristics of the respondents are displayed in Table 2.
| Table 2: Obstetric and health care related factors of study participants. | |||
| Variable | Category | CD | VD |
| Parity | Primi parous | 80 (51.9%) | 73 (47.3%) |
| Multi parous | 74 (48.1%) | 80 (53.3%) | |
| ANC follow up | Yes | 153 (99.4%) | 147 (96.1%) |
| No | 1 (0.6%) | 6 (3.9%) | |
| Multiple gestations | Yes | 6 (3.9%) | 4 (2.6%) |
| No | 148 (96.1%) | 149 (97.4%) | |
| Reason for CD | Medical indication | 152 (98.8%) | - |
| Self-request | 1 (0.6%) | - | |
| I do not know | 1 (0.6%) | - | |
| Type of CD | Emergency | 103 (66.9%) | - |
| Elective | 51 (33.1%) | - | |
| Primary/ repeat CD | Primary | 114 (74.5%) | - |
| Repeat | 39 (25.5%) | - | |
| Anesthesia used | General | 5 (3.3%) | - |
| Spinal | 149 (96.7%) | - | |
| Pain after delivery | Yes | 45 (29.3%) | 29 (19%) |
| No | 109 (70.7%) | 124 (81%) | |
| Fatigue after delivery | Yes | 55 (35.7%) | 65 (42.5%) |
| No | 99 (64.3%) | 88 (57.5%) | |
| Skin to skin contact | Yes | 21 (13.8%) | 86 (56.2%) |
| No | 127 (82.8%) | 67 (43.8%) | |
| I do not know | 5 (3.4%) | - | |
| Developed complications | Yes | 23 (14.9%) | 25 (16.3%) |
| No | 131 (85.1%) | 128 (83.7%) | |
| Support from HCW | Yes | 100 (64.9%) | 85 (55.6%) |
| No | 54 (35.1%) | 68 (44.4%) | |
| Labor onset | Spontaneous | - | 123 (80.4%) |
| Induced | - | 30 (19.6%) | |
| Augmentation | Yes | - | 38 (24.8%) |
| No | - | 115 (75.2%) | |
| Type of VD | Spontaneous | - | 128 (83.6%) |
| Assisted | - | 25 (16.4%) | |
Traditional belief related factors
The majority of the mothers with CD 113 (73.4%) and VD 125 (81.7%) fed colostrum to the neonate. Giving pre-lacteal feeding was avoided by the majority of the mothers with CD 96 (62.4%) and VD 133 (86.9%) Table 3.
| Table 3: Traditional belief related characteristics of the respondents. | |||
| Variable | Category | CD | VD |
| Fed colostrum | Yes | 113 (73.4%) | 125 (81.7%) |
| No | 41 (26.6%) | 28 (18.3%) | |
| Pre-lacteal feeding | Yes | 58 (37.6%) | 20 (13.1%) |
| No | 96 (62.4%) | 133 (86.9%) | |
| Partner/spouse support | Yes | 76 (52.4%) | 85 (58.2%) |
| No | 63 (43.4%) | 42 (28.8%) | |
| Absent during delivery | 6 (4.2%) | 19 (13%) | |
| Mother/in-law support | Yes | 55 (35.9%) | 51 (33.3%) |
| No | 26 (17%) | 19 (12.4%) | |
| Absent during delivery | 72 (47.1%) | 83 (54.2%) | |
Awareness of timely initiation of breastfeeding
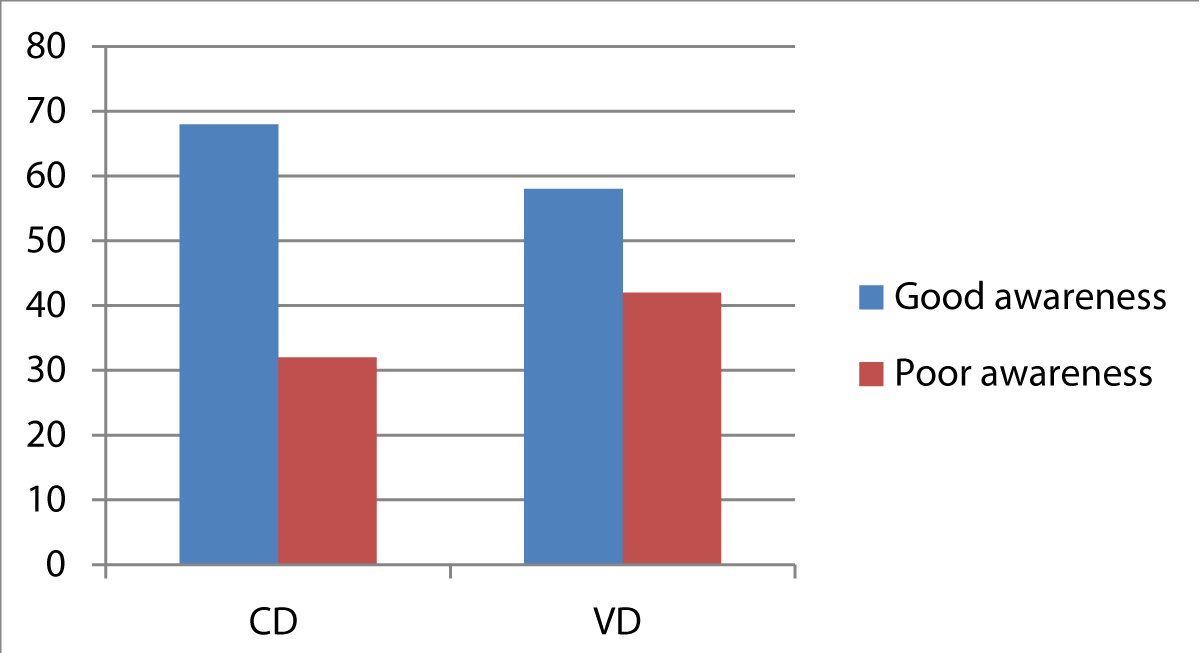
Participants were offered to answer nine questions that assess their awareness of the timely initiation of breastfeeding. Per the operational definition, 68% of mothers with CD and 58% of mothers with VD had good awareness about the timely initiation of breastfeeding (Figure 1).
Figure 1: Awareness of participants towards timely initiation of breastfeeding.
Factors associated with timely initiation of breastfeeding
Variables having a p - value less than 0.25 were inserted into the multivariate logistic regression model to determine the relationship between the dependent and independent variables. Adjusted odds ratio with 95% CI was computed to see the strength of association. With CD, multiparity (AOR = 2.14, 95% CI: 1.02 - 4.50), health care worker (HCW) support (AOR = 2.60, 95% CI: 1.16 - 5.82), and, avoiding pre-lacteal feeding (AOR = 2.54, 95% CI: 1.13 - 5.75) were significantly associated with TIBF. For respondents with VD avoiding pre-lacteal feeding (AOR = 2.54, 95% CI: 1.13 - 5.75) was the only significantly associated factor (Table 4).
| Table 4: Factors associated with timely initiation of breastfeeding. | |||||
| Variable by delivery mode | Category | TIFF | 95% CI | ||
| Yes | No | COR | AOR | ||
| Cesarean delivery | |||||
| Parity | Primi parous | 55 | 25 | 2.58 (1.34,4.99) | 2.14 (1.02-4.50)* |
| Multi parous | 34 | 40 | 1 | 1 | |
| HCW | Yes | 51 | 49 | 1 | 1 |
| No | 13 | 40 | 3.20 (1.53-6.70) | 2.60 (1.16-5.82)* | |
| Pre-lacteal feeding | Yes | 45 | 13 | 4.01 (1.92-8.38) | 2.54 (1.12-5.75)* |
| No | 44 | 51 | 1 | 1 | |
| Vaginal delivery | |||||
| Pre-lacteal feeding | Yes | 14 | 6 | 7.67 (2.72-21.65) | 5.49 (1.82-16.57)* |
| No | 31 | 102 | 1 | 1 | |
| *Significant at p < 0.05; COR: Crude Odd Ratio; AOR: Adjusted Odds Ratio; HCW: Health Care Worker. | |||||
This study aimed to compare the timely initiation of breastfeeding by the mode of delivery. The study identified that TIBF was higher for mothers with VD (80%) than mothers with CD (51%). The rate of TIBF for mothers with CD was higher in studies done in Sudan [16], Nigeria [41], Saudi Arabia [45], United Arab Emirates (UAE) [46], and China [47]. The TIBF rate was low in studies done in Dese, Ethiopia [48], and Brazil [49]. For the vaginally delivered mothers, the TIBF was higher as compared to studies from different parts of Ethiopia [14,50], Sudan [16], Nigeria [41], Saudi Arabia [45], UAE [46], while it was low for a study done on Namibia [29]. The inconsistency of findings could be a result of differences in the study area, study period, or socio-cultural factors which may lead to discrepancies in the practice of breastfeeding initiation.
Multiparity and support from the health care provider were significantly associated with the timely initiation of breastfeeding among mothers with CD. While pre-lacteal feeding status was significantly associated with TIBF among mothers with VD. Colostrum feeding status was significantly associated with the practice of timely initiation of breastfeeding with both delivery methods. With cesarean delivery, multiparous mothers were 2.14 (AOR = 2.14, 95% CI: 1.02 - 4.50) more likely to initiate breastfeeding within an hour than primiparous mothers. Women who have breastfed previously have significantly different breastfeeding experiences than primiparous women [51]. Multiparous mothers could have a personal experience in the practice of timely initiation of breastfeeding while primiparous mothers are devoid of any personal experience. Our finding was supported by studies done in the South Gondar zone in Ethiopia and Sudan [16,52]. This can be justified by the fact that multiparous mothers will have more information exposure regarding the importance of timely initiation of breastfeeding while receiving care at ANC, labor, and delivery, or post-natal services. Based on this finding, we recommend health care providers give extended support to primiparous mothers to initiate breastfeeding early.
Mothers with CD who got support from health care workers were 2.60 (AOR = 2.60, 95% CI: 1.16 - 5.82) times more likely to initiate breastfeeding than those mothers who did not get support. Breastfeeding difficulties in mothers with CD could be multifactorial. Some of the difficulties can be decreased from support and professional counseling from the health care provider about attachment and positioning of breastfeeding. Our study finding was consistent with studies done in the South Gondar zone and Goba, Ethiopia [33,52]. While breastfeeding is a natural human behavior, most mothers need practical help in learning how to breastfeed [53]. This might be the reason for the consistent finding between our study and other studies. Similar to our recommendation with primiparous mothers, health care providers should offer protracted support to mothers with cesarean section.
For mothers with VD, those who did not give pre-lacteal feeding were 2.54 (AOR = 2.54, 95% CI: 1.12 - 5.75) times more likely to initiate breastfeeding timely than their counterparts. Pre-lacteal feeding is one of the sociocultural mal-practice which may interfere with breastfeeding initiation. Our study finding was supported by studies done in different parts of Ethiopia [26,54]. The similarities of the findings could be a result of the perception of mothers about the harmfulness of pre-lacteal feeding. We recommend pre-lacteal feeding should be discouraged and mothers should be given pertinent health education regarding the harmful effect of pre-lacteal feeding during ANC follow-up.
The limitation of this study is it lacks a qualitative approach that may help to know how the mode of delivery affects breastfeeding initiation. Additionally, the nature of the study by itself does not assess the cause-and-effect relationship of factors affecting breastfeeding initiation rates. Recall bias may be introduced since the elapsed time for the first breastfeeding after delivery was recorded solely based on maternal response. Another limitation is the small sample size used for the study.
The study showed that the rate of timely initiation of breastfeeding was low from the plan set by the Ministry of Health, Ethiopia to increase the proportion of newborns to start breastfeeding within the first hour of life by the year 2015. The breastfeeding initiation rate was different from the mode of delivery. Cesarean delivery was associated with a lower breastfeeding initiation rate and a higher mean time of breastfeeding initiation. Therefore we would like to recommend the health care providers in the maternity ward of public hospitals in Addis Ababa give appropriate and adequate support to the mothers for timely initiation of breastfeeding with emphasis on cesarean delivered and first-time mothers.
Author contributions: A.M and Z.S made an equal contribution during topic conceptualization, proposal development, design, analysis, and interpretation. A.M prepared the manuscript.
Funding: This research received no external funding
Institutional review board statement: The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board Committee of Menilik II Health and Medical Sciences College, Kotebe Metropolitan University.
Informed consent statement: Informed consent was obtained from all subjects involved in the study.
Data availability statement: The datasets analyzed during the current study are available from the corresponding author on reasonable request.
Acknowledgment: We would like to acknowledge Kotebe Metropolitan University, Menelik II Medical and Health Science College, the facilitator, data collectors, and study participants.
Conflicts of interest: The authors declare no conflict of interest.
- Chamotra S, Chaudhary A, Sachdeva A. Breastfeeding: Why We Still Need To Address This Universal Truth? 2020; 4421:16–18.
- Binns C, Lee M, Low WY. The Long-Term Public Health Benefits of Breastfeeding. Asia-Pacific J Public Health. 2016; 28:7–14. PubMed: https://pubmed.ncbi.nlm.nih.gov/26792873/
- Hahn-Holbrook J, Schetter CD, Angeles L, Haselton MG, Angeles L. The Advantages and Disadvantages of Breastfeeding for Maternal Mental and Physical Health. Reprod Health. 2013; 414–39.
- Barriers to Breastfeeding: Supporting Initiation and Continuation of Breastfeeding: ACOG Committee Opinion Summary. Obstetr Gynecol. 2021; 137: 396–397. PubMed: https://pubmed.ncbi.nlm.nih.gov/33481527/
- WHO. Infant and Young Child Feeding A tool for assessing national practicies, policies and programmes World Health Organization. 2003; 156.
- Debes AK, Kohli A, Walker N, Edmond K, Mullany LC. Time to initiation of breastfeeding and neonatal mortality and morbidity: A systematic review. BMC Public Health. 2013; 13:S19. PubMed: https://pubmed.ncbi.nlm.nih.gov/24564770/
- Mullany LC, Katz J, Khatry SK, LeClerq SC, Darmstadt GL, T et al. Neonatal hypothermia and associated risk factors among newborns of southern Nepal. BMC Med. 2010; 8: 43. PubMed: https://pubmed.ncbi.nlm.nih.gov/20615216/
- Phukan D, Ranjan M, Dwivedi LK. Impact of timing of breastfeeding initiation on neonatal mortality in India. Int Breastfeed J. 2018; 13:1–10.
- Lim G, Facco FL, Nathan N, Waters JH, Wong CA, et al. A review of the impact of obstetric anesthesia on maternal and neonatal outcomes. Anesthesiology. 2018; 129:192–215. PubMed: https://pubmed.ncbi.nlm.nih.gov/29561267/
- Smith ER, Hurt L, Chowdhury R, Sinha B, Fawzi W, et al. Delayed breastfeeding initiation and infant survival: A systematic review and meta-analysis. PLoS One. 2017; 12:e0180722. PubMed: https://pubmed.ncbi.nlm.nih.gov/28746353/
- Ezeh OK, Ogbo FA, Stevens GJ, Tannous WK, Uchechukwu OL, et al. Factors associated with the early initiation of breastfeeding in economic community of West African States (ECOWAS). Nutrients. 2019; 11:2765. PubMed: https://pubmed.ncbi.nlm.nih.gov/31739498/
- Paksoy Erbaydar N, Erbaydar T. Relationship between caesarean section and breastfeeding: Evidence from the 2013 Turkey demographic and health survey. BMC Pregnancy Childbirth. 2020; 20:55. PubMed: https://pubmed.ncbi.nlm.nih.gov/31992238/
- Ephrem Y, Tsegaye T. Timely initiation of breastfeeding and associated factors among mothers who have infants less than six months of age in Gunchire Town, Southern Ethiopia 2019. Clin J Obstet Gynecol. 2020; 3:026–032. PubMed: https://www.obstetricgynecoljournal.com/journals/cjog/cjog-aid1106.php
- Ahmed KY, Page A, Arora A, Ogbo FA. Trends and determinants of early initiation of breastfeeding and exclusive breastfeeding in Ethiopia from 2000 to 2016. Int Breastfeed J. 2019; 14: 40. PubMed: https://pubmed.ncbi.nlm.nih.gov/31528197/
- Hobbs AJ, Mannion CA, McDonald SW, Brockway M, Tough SC. The impact of caesarean section on breastfeeding initiation, duration and difficulties in the first four months postpartum. BMC Pregnancy Childbirth. 2016; 16:90. PubMed: https://pubmed.ncbi.nlm.nih.gov/27118118/
- Abdel-Rahman ME, El-Heneidy A, Benova L, Oakley L. Early feeding practices and associated factors in Sudan: A cross-sectional analysis from multiple Indicator cluster survey. Int Breastfeed J. 2020; 15:1–11.
- Yisma E, Mol BW, Lynch JW, Smithers LG. Impact of caesarean section on breastfeeding indicators: Within-country and meta-analyses of nationally representative data from 33 countries in sub-Saharan Africa. BMJ Open. 2019; 9:1–12. PubMed: https://pubmed.ncbi.nlm.nih.gov/31488470/
- Nkoka O, Ntenda PAM, Kanje V, Milanzi EB, Arora A. Determinants of timely initiation of breast milk and exclusive breastfeeding in Malawi: A population-based cross-sectional study. Int Breastfeed J. 2019; 14:1–9.
- Liben ML, Yesuf EM. Determinants of early initiation of breastfeeding in Amibara district, Northeastern Ethiopia: a community based cross-sectional study. Int Breastfeed J. 2016; 1–7. PubMed: https://pubmed.ncbi.nlm.nih.gov/27064535/
- Whitaker B. 110 Guided Imagery: Beyond Procedural Fear and Pain - Techniques For Children, Adolescents and You, the Health Professional. Arch Dis Child. 2012; 97:A31–A31.
- Guala A, Boscardini L, Visentin R, Angellotti P, Grugni L, et al. Skin-to-Skin Contact in Cesarean Birth and Duration of Breastfeeding: A Cohort Study. Sci World J. 2017; 2017: 1940756. PubMed: https://pubmed.ncbi.nlm.nih.gov/29082306/
- Essa RM, Abdel Aziz Ismail NI. Effect of early maternal/newborn skin-to-skin contact after birth on the duration of third stage of labor and initiation of breastfeeding. J Nurs Educ Pract. 2015; 5.
- Kuyper E, Vitta B, Dewey K. Implications of Cesarean Delivery for Breastfeeding Outcomes and Strategies to Support Breastfeeding association of cesarean delivery with reduced rates of initiation of breastfeeding. Alive & Thrive. 2014.
- Mutia C, Kamil H, Susanti SS. Determinant Factors of Early Initiation of Breastfeeding in Postpartum Sectio Caesarean Mothers in Aceh, Indonesia. 2020; 0966:96–101.
- Kutlucan L, Seker İS, Demiraran Y, Ersoy Ö, Karagöz İ, et al. Effects of different anesthesia protocols on lactation in the postpartum period. J Turkish Ger Gynecol Assoc. 2014; 15:233–238. PubMed: https://pubmed.ncbi.nlm.nih.gov/25584032/
- Derso T, Biks GA, Tariku A, Tebeje NB, Gizaw Z, et al. Correlates of early neonatal feeding practice in Dabat HDSS site, northwest Ethiopia. Int Breastfeed J. 2017; 12: 25. PubMed: https://pubmed.ncbi.nlm.nih.gov/28592986/
- Woldeamanuel BT. Trends and factors associated to early initiation of breastfeeding, exclusive breastfeeding and duration of breastfeeding in Ethiopia: Evidence from the Ethiopia Demographic and Health Survey 2016. Int Breastfeed J. 2020; 15:3. PubMed: https://pubmed.ncbi.nlm.nih.gov/31924229
- Albokhary AA, James JP. Does cesarean section have an impact on the successful initiation of breastfeeding in Saudi Arabia? Saudi Med J. 2014; 35:1400–1403. PubMed: https://pubmed.ncbi.nlm.nih.gov/25399221/
- Ndirangu MN, Gatimu SM, Mwinyi HM, Kibiwott DC. Trends and factors associated with early initiation of breastfeeding in Namibia: Analysis of the Demographic and Health Surveys 2000-2013. BMC Pregnancy Childbirth. 2018; 18:171. PubMed: https://pubmed.ncbi.nlm.nih.gov/29769063/
- Hailemariam TW, Adeba E, Sufa A. Predictors of early breastfeeding initiation among mothers of children under 24 months of age in rural part of West Ethiopia Global health. BMC Public Health. 2015; 15:1076. PubMed: https://pubmed.ncbi.nlm.nih.gov/26489955/
- Bimerew A, Teshome M, Kassa GM. Prevalence of timely breastfeeding initiation and associated factors in Dembecha district, North West Ethiopia: A cross-sectional study. Int Breastfeed J. 2016; 11:28. PubMed: https://pubmed.ncbi.nlm.nih.gov/27757141/
- Tilahun G, Degu G, Azale T, Tigabu A. Prevalence and associated factors of timely initiation of breastfeeding among mothers at Debre Berhan town, Ethiopia: a cross- sectional study. Int Breastfeed J. 2016; 11: 27. PubMed: https://pubmed.ncbi.nlm.nih.gov/27729937/
- Setegn T, Gerbaba M, Belachew T. Determinants of timely initiation of breastfeeding among mothers in Goba Woreda, South East Ethiopia: A cross sectional study. BMC Public Health. 2011; 217. PubMed: https://pubmed.ncbi.nlm.nih.gov/21473791/
- Parthasarathy S, Rajah C. Feasibility of early breast feeding after caesarean section. Sri Lanka J Child Heal. 2011; 40:11–2.
- Yaya S, Bishwajit G, Shibre G, Buh A. Timely initiation of breastfeeding in Zimbabwe: Evidence from the demographic and health surveys 1994-2015. Int Breastfeed J. 2020; 15:10. PubMed: https://pubmed.ncbi.nlm.nih.gov/32070375/
- Kiani SN, Rich KM, Herkert D, Safon C, Pérez-Escamilla R. Delivery mode and breastfeeding outcomes among new mothers in Nicaragua. Matern Child Nutr. 2018; 14:e12474. PubMed: https://pubmed.ncbi.nlm.nih.gov/28621054/
- Victora CG, Bahl R, Barros AJD, França GVA, Horton S, et al. Breastfeeding in the 21st century: Epidemiology, mechanisms, and lifelong effect. Lancet. 2016; 387:475–490. PubMed: https://pubmed.ncbi.nlm.nih.gov/26869575/
- UNICEF, WHO. Capture the Moment – Early initiation of breastfeeding: The best start for every newborn. Int Unicef. 2018. 1–42.
- Ethiopian Demographic Health Survey, 2016.
- Takahashi K, Ganchimeg T, Ota E, Vogel JP, Souza JP, et al. Prevalence of early initiation of breastfeeding and determinants of delayed initiation of breastfeeding: Secondary analysis of the WHO Global Survey. Sci Rep. 2017; 7:44868. PubMed: https://pubmed.ncbi.nlm.nih.gov/28322265/
- Berde AS, Yalcin SS. Determinants of early initiation of breastfeeding in Nigeria: A population-based study using the 2013 demograhic and health survey data. BMC Pregnancy Childbirth. 2016; 16:32. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4744410/
- Draft F. Federal Democratic Republic of Ethiopia Ministry of Health Health Sector Development Program IV October 2010 Contents. 2014.
- Dudeja S, Sikka P, Jain K, Suri V, Kumar P. Improving First-hour Breastfeeding Initiation Rate After Cesarean Deliveries: A Quality Improvement Study. Indian Pediatr. 2018; 55:761–764. PubMed: https://pubmed.ncbi.nlm.nih.gov/30345980/
- Patel A, Bucher S, Pusdekar Y, Esamai F, Krebs NF, et al. Rates and determinants of early initiation of breastfeeding and exclusive breast feeding at 42 days postnatal in six low and middle-income countries: A prospective cohort study. Reprod Health. 2015; 12: S10. PubMed: https://pubmed.ncbi.nlm.nih.gov/26063291/
- Ahmed AE, Salih OA. Determinants of the early initiation of breastfeeding in the Kingdom of Saudi Arabia. Int Breastfeed J. 2019; 14:13. PubMed: https://pubmed.ncbi.nlm.nih.gov/30984282/
- Taha Z, Hassan AA, Wikkeling-Scott L, Papandreou D. Prevalence and associated factors of caesarean section and its impact on early initiation of breastfeeding in Abu Dhabi, United Arab Emirates. Nutrients. 2019; 11: 2723. PubMed: https://pubmed.ncbi.nlm.nih.gov/31717627/
- Chen C, Yan Y, Gao X, Xiang S, He Q, et al. Influences of Cesarean Delivery on Breastfeeding Practices and Duration: A Prospective Cohort Study. J Hum Lact. 2018; 34:526–534. PubMed: https://pubmed.ncbi.nlm.nih.gov/29365288/
- Shiferaw R, Tadesse SE, Mekonnen TC, Zerga AA. Timely initiation of breast feeding and associated factors among caesarian section delivered mothers in health facilities of dessie city administration, North Eastern Ethiopia. Pediatr Rep. 2020; 13:1–8. PubMed: https://pubmed.ncbi.nlm.nih.gov/33374654/
- Tavares de Arruda G, Cabreira Barreto S, Lago Morin V, do Nascimento Petter G, Medeiros Braz M, et al. Existe relação da via de parto com a amamentação na primeira hora de vida? Rev Bras em Promoção da Saúde. 2018; 31:1–7.
- Gebremeskel SG, Gebru TT, Gebrehiwot BG. Early initiation of breastfeeding and associated factors among mothers of aged less than 12 months children in rural eastern zone , Tigray , Ethiopia : cross ‑ sectional study. BMC Res Notes. 2019; 12: 671. PubMed: https://pubmed.ncbi.nlm.nih.gov/31639055/
- Hackman NM, Schaefer EW, Beiler JS, Rose CM, Paul IM. Breastfeeding Outcome Comparison by Parity 1 1. 2015; 10:156-162. PubMed: https://pubmed.ncbi.nlm.nih.gov/25549051/
- Getnet B, Degu A, Yenealem F. Prevalence and associated factors of early initiation of breastfeeding among women delivered via Cesarean section in South Gondar zone hospitals Ethiopia, 2020. Matern Heal Neonatol Perinatol. 2020; 6:6. PubMed: https://pubmed.ncbi.nlm.nih.gov/33298188/
- Baby Friendly Hospital initiative, Frequently Asked Questions. 2018.
- Temesgen H, Negesse A, Woyraw W, Getaneh T, Yigizaw M. Prelacteal feeding and associated factors in Ethiopia: Systematic review and meta-analysis. Int Breastfeed J. 2018; 13:49. PubMed: https://pubmed.ncbi.nlm.nih.gov/30505338/