More Information
Submitted: August 03, 2021 | Approved: August 13, 2021 | Published: August 16, 2021
How to cite this article: Tang TW, Jessie PWL. Leiomyosarcoma in pregnancy: Incidental finding during routine caesarean section. Clin J Obstet Gynecol. 2021; 4: 092-095.
DOI: 10.29328/journal.cjog.1001094
Copyright License: © 2021 Tang TW, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Leiomyosarcoma; Pregnancy; Caesarean section
Leiomyosarcoma in pregnancy: Incidental finding during routine caesarean section
Toon Wen Tang* and Phoon Wai Leng Jessie
Obstetrics and Gynaecology, KK Women’s and Children’s Hospital, Singapore, Singapore
*Address for Correspondence: Dr. Toon Wen Tang, Department of Obstetrics and Gynaecology, KK Women’s and Children’s Hospital, 100 Bukit Timah Rd, Singapore 229899, Singapore, Tel: +6597358506; Email: [email protected]
Uterine leiomyosarcoma (LMS) is uncommon tumour arising from the female reproductive tract. Incidence of LMS in pregnancy is extremely rare, with only 10 cases reported thus far in medical literature.
We present a case of myomectomy performed during elective caesarean section for breech presentation, due to its easy accessibility and well contracted uterus. Subsequent histology revealed LMS on final specimen. Patient subsequently underwent total abdominal hysterectomy, bilateral salpingo-oophorectomy. No chemotherapy was given as she opted for close clinical- radiological monitoring instead.
This case report highlights the importance of discussion with patients regarding the risk of occult malignancy in a fibroid uterus. Appropriate management of uterine leiomyosarcoma in pregnancy remains unclear. Consideration of removing an enlarging leiomyoma during caesarean section might be ideal in view of its malignant potential, just like in this case; however, location of the tumour and risk of bleeding needs to be weighed. Ultimately, management of such cases needs proper discussion between obstetrician and the patient.
The incidence of uterine leiomyosarcoma (LMS) is uncommon, registering 0.64/100 000 women annually [1]. It accounts for approximately 1.3% of all uterine malignancies. LMS tumours are usually highly malignant neoplasms with an overall poor prognosis. Most commonly, LMS presents after childbearing age, and the reported mean age of patients range from 45.0 to 56.9 years old [2,3]. Occurrence during childbearing age is not common and uterine LMS during pregnancy is even rarer, with only 10 cases reported thus far in medical literature.
Myomectomy is not routinely practiced during caesarean section due to the associated risk of severe haemorrhage. Exceptions include small, pedunculated fibroids; those obstructing the delivery of the foetus or fibroids which are highly suspicious of malignancy based on scans. Therefore, there are cases in which diagnosis of LMS are missed and are only incidentally picked-up during caesarean section for other reasons.
We present a case of uterine LMS incidentally diagnosed after elective caesarean section for breech, in which, myomectomy was done for an intramural/submucosal fibroid.
Investigations
A 30 year old Gravida 2 Parity 2 has been on regular follow up for her stable fibroid of 5 cm in KK Women’s and Children’s Hospital since 2015. She achieved spontaneous pregnancy and regular ultrasonography was done for the follow up for her fibroid. This fibroid was present in her first pregnancy and grew to 11cm then too – but shrunk back to 5 cm after her first delivery in 2015. In the latter pregnancy in 2018, the uterine mass (what thought to be the fibroid) increased in size and subsequently remained stable throughout the rest of the pregnancy, ranging from 11-13 cm.
Diagnosis
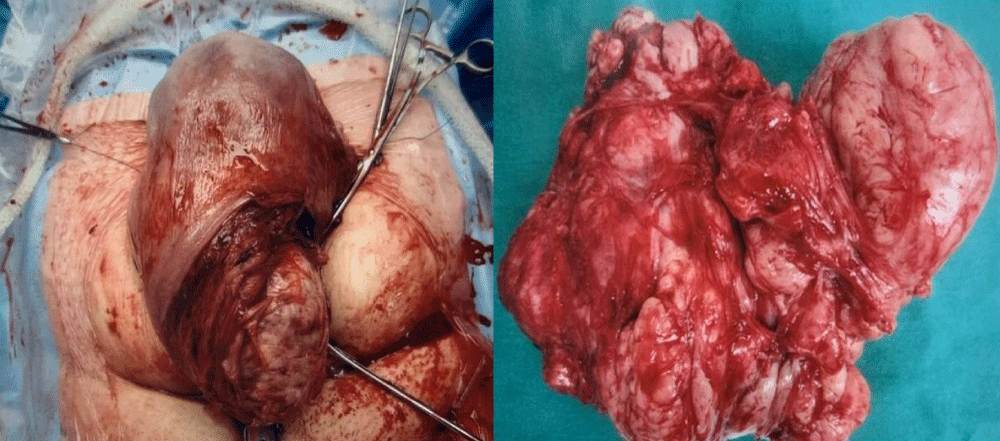
She underwent lower midline caesarean section for breech on 21/12/18 at 38+3 weeks. Intraoperatively: a 19 cm in largest diameter intramural/submucous fibroid was noted in the right lower uterine segment (Figure 1). Uterine incision was made above the fibroid and baby was delivered via breech extraction. Decision for myomectomy was made as the intramural/submucous fibroid was easily accessible and uterus was well contracted. Fibroid was sent for histology and the report revealed high grade spindle cell leiomyosarcoma.
Figure 1: 19 cm intramural/submucous fibroid noted in the right lower uterine segment during caesarean section
Treatment
She was recalled back early for CT thorax, abdomen, pelvis on 22/1/19. Scan showed a stable fibroid corresponding to the one seen on ultrasound previously in 2015, with no radiological evidence of distant metastases.
Completion surgery with total abdominal hysterectomy, bilateral salpingo-oophorectomy, bilateral pelvic lymph nodes dissection and omental biopsy was done on 14/2/19. Post operatively, she recovered well and was discharged on post-operative day 3. Histology showed small amount of focal residual leiomyosarcoma within its wall with no evidence of local or distant metastasis.
Follow up and outcomes
Tumour board discussion was done and staging was confirmed to be Stage 1B high grade leiomyosarcoma. Systemic chemotherapy was recommended in view of high risk of recurrence and medical oncologist was referred. However, patient opted for close clinic radiologic monitoring instead, after weighing the risks and benefits. Till date, her 3 monthly scans showed no evidence of local recurrence and she remains well and healthy.
Uterine leiomyosarcoma (LMS) is an uncommon smooth muscle tumour and they account for just 1.3% of all uterine malignancies. Presentation of LMS can include abnormal uterine bleeding, abdominal pain and/or pelvic mass. Incidence of uterine LMS in pregnancy is even rarer and only a total of 10 cases have been reported in medical literature. In addition, all cases of uterine leiomyosarcoma associated with pregnancy from the literature were found incidentally. Similarly to the literature, the diagnosis of leiomyosarcoma for our case was only made histologically, post caesarean section.
For our case, despite noting the fibroid prior to pregnancy and ensuring regular follow up scans throughout pregnancy, there were no clinical suspicions to indicate malignancy. Therefore, the tumour was mistakenly diagnosed as leiomyoma. Unlike Kyodo, et al. [4] case, which is the only case that myomectomy was performed during caesarean as ultrasonography showed suspicious features; the indication for caesarean in our case was for breech presentation. Additionally, myomectomy was performed in the same setting only because the fibroid was easily accessible (largely submucosal with clear margin capsule) and the uterus being well contracted.
Although a rapidly growing uterus may anecdotally raise concerns regarding uterine sarcoma, pregnancy complicates this as approximately 25% of leiomyoma routinely enlarge during pregnancy due to elevated levels of oestrogen and progesterone levels [5]. Oestrogen and progesterone have been thought to be the primary promoter of uterine leiomyoma growth. This is based on clinical observation that fibroids only occur after menarche, developmental during reproductive years and regression following menopause. This hypothesis is supported by regression of myomas with medical treatment via GnRH agonists [6]. Hence, although diagnosis of cancer is unlikely during pregnancy, it is important to be aware of the possibility in order to better counsel patients with a known fibroid to determine the necessity for a myomectomy during the time of delivery.
Nonetheless, myomectomy during caesarean section has and is still a controversial topic due to the attendant risk of severe haemorrhage. Exception includes: small, pedunculated fibroids, location at the lower segment in which removal of myoma is mandatory in order for delivery of the foetus. In medical literature, however, there are few studies which directly address this controversy. Case studies by Tinelli, et al. [7], Ramesh Kumar, et al. [8], Kanthi, et al. [9], Li, et al. [10] and Machado, et al. [11] have shown that myomectomy during caesarean section can be safe, effective, with minimal intra and post op complications in the hands of experienced surgeons. Review article of nine studies by Song, et al. [12] concluded that caesarean myomectomy may be a reasonable option in some patients but data driven from the meta-analysis were low quality, and definitive conclusion on this issue cannot be drawn. The recommendation of whether caesarean myomectomy should be done relies entirely on a body of evidence consisting of case series and anecdotes which give conflicting results.
To complicate the issue further, till date, there is no one imaging modality that can accurately and reliably distinguish between benign and malignant leiomyomas. It is thought that pelvic ultrasound followed by magnetic resonance imaging (MRI) is the best imaging strategy for LMS. Sonographic features such as mixed echogenic and poor echogenic parts, central necrosis and colour Doppler findings of irregular vessel distribution in pelvic ultrasound can be suggestive of LMS, however, it may also be present in leiomyomas [13]. Additionally, although scattered haemorrhagic or necrotic mass on MRI should raise a suspicion of LMS, it does not provide a definitive diagnosis.
Primary treatment of leiomyosarcoma is surgery and the standard procedure is total abdominal hysterectomy, bilateral salpingo-oophorectomy. Myomectomy can be considered an alternative if the patient desires future pregnancies, but only if they understand and accept the risk of residual leiomyosarcoma and risk of recurrence. The role of lymphadenectomy for uterine leiomyosarcoma is controversial due to the limited number of studies and conflicting literature. Incidence of lymph node metastasis from uterine leiomyosarcoma is very low and unlikely in absence of extrauterine disease [14]. Therefore, routine lymphadenectomy is not done for patients with localized confined disease and normal lymph nodes on observation and palpation [15,16]. Another school of thought is that lymphadenectomy may be of clinical benefit for both prognostication and potential palliation by determining the need for adjuvant chemotherapy and pelvic radiotherapy as demonstrated by Giuntoli, et al. [17] however, the therapeutic benefit is yet to be proven.
Till date, current literature with regards to role of adjuvant therapy for uterine leiomyosarcoma remains indeterminate. Majority of published studies have reported recurrence rates of 50% - 60% in early stage uterine leiomyosarcoma. Therefore, adjuvant treatment with chemotherapy, specifically gemcitabine/docetaxel alone or together with doxorubicin, can be beneficial for these group of patients [18,19]. Despite a phase III study conducted by the Gynaecologic Oncology Group in 1980s showing a lower recurrence rate in the chemotherapy treated group, the result was not statistically significant and the survival rates were not different between the groups [20]. Given the conflicting evidence, the role of adjuvant chemotherapy remains unclear and should be discussed with the patient, weighing both the benefits and side effects of the treatment.
Learning points
This case report highlights the importance of discussion with patients regarding the risk of occult malignancy in a fibroid uterus. Appropriate management of uterine leiomyosarcoma in pregnancy remains unclear. Consideration of removing an enlarging leiomyoma during caesarean section might be ideal in view of its malignant potential, just like in this case; however, location of the tumour and risk of bleeding needs to be weighed. Ultimately, management of such cases needs proper discussion between obstetrician and the patient.
Declarations
Informed consent: Yes
Data availability: The data supporting the findings of this study are available from the corresponding author upon reasonable request.
- Gallup DG, Cordray DR. Leiomyosarcoma of the uterus: case reports and a review. Obstet Gynecol Surv. 1979; 34: 300-312. PubMed: https://pubmed.ncbi.nlm.nih.gov/471365/
- Park JY, Park SK, Kim DY, Kim JH, Kim YM, et al. The impact of tumor morcellation during surgery on the prognosis of patients with apparently early uterine leiomyosarcoma. Gynecol Oncol. 2011; 122: 255–259. PubMed: https://pubmed.ncbi.nlm.nih.gov/21565389/
- Lissoni A, Cormio G, Bonazzi C, Perego P, Lomonico S, et al. Fertility-sparing surgery in uterine leiomyosarcoma. Gynecologic Oncol. 1988; 70: 348–350. PubMed: https://pubmed.ncbi.nlm.nih.gov/9790786/
- Kyodo Y, Inatomi K, Abe T. Sarcoma associated with pregnancy. Am J Obstet Gynaecol. 1989; 161: 94–96. PubMed: https://pubmed.ncbi.nlm.nih.gov/2750827/
- Matsuo K, Eno ML, Im DD, Rosenshein NB. Pregnancy and genital sarcoma: a systematic review of the literature. Am J Perinatol. 2009; 26: 507–518. PubMed: https://pubmed.ncbi.nlm.nih.gov/19288396/
- Flake GP, Andersen J, Dixon D. Etiology and pathogenesis of uterine leiomyomas: a review. Environ Health Perspect. 2003; 111: 1037-1054. PubMed: https://pubmed.ncbi.nlm.nih.gov/12826476/
- Tinelli A, Malvasi A, Mynbaev OA, Barbera A, Perrone E, et al. The surgical outcome of intracapsular cesarean myomectomy. A match control study. J Matern Fetal Neonatal Med. 2013; 27: 66-71. PubMed: https://pubmed.ncbi.nlm.nih.gov/23662726/
- Ramesh Kumar R, Patil M, Shruthi SA. The utility of caesarean myomectomy as a safe procedure: A retrospective analysis of 21 cases with review of literature. J Clin Diagn Res. 2014; 8: OC05-8. PubMed: https://pubmed.ncbi.nlm.nih.gov/25386485/
- Kanthi, JM, Sumathy S, Sreedhar S, Rajammal B, Usha MG, et al. Comparative Study of Cesarean Myomectomy with Abdominal Myomectomy in Terms of Blood Loss in Single Fibroid. J Obstet Gynaecol India. 2016; 66: 287-291. PubMed: https://pubmed.ncbi.nlm.nih.gov/27382224/
- Li H, Du J, Jin LY, Shi Z, Liu MY. Myomectomy during cesarean section. Acta Obstetricia et Gynecologica Scandinavica. 2009; 88: 183-186.
- Machado LS, Gowri V, Al-Riyami N, Al-Kharusi L. Caesarean myomectomy. Feasibility and safety. Sultan Qaboos Univ Med J. 2012; 12: 190-196. PubMed: https://pubmed.ncbi.nlm.nih.gov/22548138/
- Song DR, Zhang W, Chames MC, Guo J. Review article. Myomectomy during cesarean delivery. Int J Gynaecol Obstet. 2013; 121: 208-213. PubMed: https://pubmed.ncbi.nlm.nih.gov/23507551/
- Bužinskienė D, Mikėnas S, Drąsutienė G. Uterine sarcoma: a clinical case and a literature review. Acta Med Litu. 2018; 25: 206-218. PubMed: https://pubmed.ncbi.nlm.nih.gov/31308826/
- Harry VN, Narayansingh GV, Parkin DE. Uterine leiomyosarcomas: a review of the diagnostic and therapeutic pitfalls. Obstetrician Gynaecologist. 2007; 9: 88-94.
- Leitao MM, Sonoda Y, Brennan MF, Barakat RR, Chi DS. Incidence of lymph node and ovarian metastases in leiomyosarcoma of the uterus. Gynecol Oncol. 2003; 91: 209–212. PubMed: https://pubmed.ncbi.nlm.nih.gov/14529683/
- Goff BA, Rice LW, Fleischhacker DN, Muntz HG, Falkenberry SS, et al. Uterine leiomyosarcoma and endometrial stromal sarcoma: lymph node metastases and sites of recurrence. Gynecol Oncol. 1993; 50: 105–109.
- Giuntoli RL, Metzinger DS, DiMarco CS, Cha SS, Sloan JA, et al. Retrospective review of 208 patients with leiomyosarcoma of the uterus: prognostic indicators, surgical management, and adjuvant therapy. Gynecol Oncol. 2003; 89: 460-469. PubMed: https://pubmed.ncbi.nlm.nih.gov/12798712/
- Hensley ML, Ishill N, Soslow R, Larkin J, Abu-Rustum N, et al. Adjuvant gemcitabine plus docetaxel for completely resected stages I–IV high grade uterine leiomyosarcoma: results of a prospective study. Gynecol Oncol. 2009; 112: 563-567. PubMed: https://pubmed.ncbi.nlm.nih.gov/19135708/
- Hensley ML, Wathen JK, Maki RG, Araujo DM, Sutton G, et al. Adjuvant therapy for high-grade, uterus-limited leiomyosarcoma: results of a phase 2 trial (SARC 005). Cancer. 2013; 119: 1555–1561. PubMed: https://pubmed.ncbi.nlm.nih.gov/23335221/
- Omura GA, Blessing JA, Major F, Lifshitz S, Ehrlich CE, et al. A randomized clinical trial of adjuvant adriamycin in uterine sarcomas: a Gynecol Oncol Group Study. J Clin Oncol. 1985; 3: 1240-1245. PubMed: https://pubmed.ncbi.nlm.nih.gov/3897471/