More Information
Submitted: 08 September 2020 | Approved: 30 November 2020 | Published: 01 December 2020
How to cite this article: Farid G, Kamal R, Al-Shammari MT, Swaraldahab M, Swaraldahab H. Experience with trans radial uterine artery embolisation for uterine fibroids in a tertiary center in Saudi Arabia. Clin J Obstet Gynecol. 2020; 3: 167-174.
DOI: 10.29328/journal.cjog.1001072
Copyright License: © 2020 Farid G, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abbreviations: UAE: Uterine Artery Embolization; MRI: Magnetic Resonance Imaging; PT: Prothrombin Time; APTT: Activated Partial Thromboplastin Time; PCA: Patient Controlled Analgesia; Ant.: Anterior; Post: Posterior; (O): Include Anterior, Posterior And Lateral Collectively; F: Fundal; Cx: Cervical; I.M: Intramuscular; S.S: Subserous; S.M: Submucosal
Experience with trans radial uterine artery embolisation for uterine fibroids in a tertiary center in Saudi Arabia
Gehan Farid*, Reem Kamal, Mohammed Thani Al-Shammari, Mohamed Swaraldahab and Hassan Swaraldahab
Department of Obstetrics and Gynecology, Security Forces Hospital, Riyadh, Saudi Arabia
*Address for Correspondence: Dr. Gehan Farid, Department of Obstetrics and Gynecology in Security Forces Hospital, Riyadh, Saudi Arabia, Email: [email protected]
Trans-radial uterine artery embolization (UAE) is acknowledged as a non- invasive, cost-effective and safe procedure for the treatment of symptomatic fibroids. However, it is associated with the recurrence of symptoms like abnormal uterine bleeding and pressure symptom in some patients. This is a comparative study of our data with other international data, in the context of percentage reduction in fibroid size, accompanying controlling factors, short and long term follow up data analysis of the first two years was done. Careful pre-procedural counseling of future possibility of fibroid recurrence and means of management should be stressed.
Materials and methods: A retrospective cohort study at the Security Forces Hospital in Riyadh, Saudi Arabia, was conducted. The study was done from 1st November 2017-31st October 2019, on symptomatic patients diagnosed with fibroids, who refused surgical treatment.
The outcomes included: fibroid site, size and anatomical position, patients’ symptoms, general condition, and early and delayed complications. These data were compared with those from other international studies.
Results: The study involved 23 patients (mean age: 39 years). The average percentage reduction in fibroid volume was 49%. There were no major complications and no recurrence of symptoms during the covered period. Data analysis revealed a poor correlation between the overall percentage reduction of fibroid size with fibroid number, age of patients’, and body mass indices.
Conclusion: Despite poor correlation, we provided preliminary data of the first two years out of the total five-year projected period of the study where it showed effectiveness and relative safety of radial - UAE for fibroid.
Uterine Leiomyomas occur in about 20% - 80% of females by the age of 50 years, and in most patients it’s asymptomatic. The treatment options include medical as well as surgical methods in the form of a myomectomy and hysterectomy. Medical treatment can be in the form of combined oral contraceptives, oral progestogens, progestin releasing intrauterine devices, gonadotrophin releasing hormone analogues (GnRHa), selective progesterone receptor modulators (SPRM), tranexamic acid (Cyklokapron) and nonsteroidal anti- inflammatory drugs. Other forms of treatment include minimally invasive methods, such as high intensity ultrasound (HIFU), myolysis, crymolysis, laser, laparoscopic bipolar coagulation of uterine vessels and uterine artery embolization. The uterine artery embolization treatment method was used to treat patients at Security Force Hospital, and due to this, it became the focus of our study.
Our experience with uterine artery embolization, in this institute, dates to the year 2004, where all cases done, then, were via the Trans-Femoral route. The transition to the trans-radial route was instituted in 2017, by the radiology department, and from there on became the preferable route of the procedure.
This retrospective study was conducted between November 1st 2017 to October 31st 2019 and illustrates our experience with trans-radial uterine artery embolization method used to treat symptomatic fibroids in a Saudi population of the dependents of Ministry of Interior who were treated at the Security Forces Hospital, in Riyadh, Saudi Arabia. No agreement from the ethical committee at the hospital was needed. The data obtained through the computerized medical record viewer (MR Viewer) included the patient’s age, parity, marital status, employment history, smoking history, and past periods of follow-up.
Furthermore, any previously received therapy, duration, type of symptoms, investigations conducted, major effects of fibroids on the patient, and associated medical and surgical disorders that co-exist with the symptomatic fibroids were thoroughly studied.
Additionally, a Two-dimension ultrasound was conducted to confirm the initial diagnosis of fibroid and to review the number, size, anatomical site, and the presence of related cystic and other degenerative changes, as well as the co-existence of pedunculated changes. These symptomatic patients were counseled on the definitive methods of treatment, namely myomectomy, trans-radial uterine artery embolization and hysterectomy as a final resort. Once embolization was chosen, contraindications such as pelvic infection, pregnancy and malignancy were ruled out. Furthermore, the patients were informed about early (occurring within four weeks) and late (occurring beyond one month) complications of radial –UAE with special stress on the failure rate that can occur in up to one third of the patients within five years’ time. Therefore, this mandated the possible repetition of the procedure or the implementation of other forms of treatment such as a hysterectomy. A pre-procedure general systemic examination was conducted for all patients, in addition to the clinical pelvic exams for married female participants, where Pap smears, high vaginal swabs (if needed), and endometrial samples, if there were suspicious ultrasound findings, were obtained. A basal MRI of the pelvis was requested followed by repetition in six to ten months post procedure. The MRI provided more details on the presence of cystic and necrotic changes in fibroids, both before and after the procedure. In addition, it helped in the elucidation of adenomyosis, as well as any existing ovarian and tubal pathologies.
The procedure was done via an inpatient set up, by a specialized intensive Radiologist, in the radiology department. Pre- admission basic laboratory investigations included complete blood picture, thyroid function tests, pregnancy test, prolactin level tests, and the Luteinizing and Follicle stimulating hormones. After admission by the attending gynecologist, with shared care by the radiologist and any other needed specialists (a multidisciplinary team approach), post-admission investigations and tests included repeat complete blood count, PT/APTT levels, blood urea, electrolyte levels, and blood group. Informed consent for the procedure was obtained. A pre-procedure eight hour fast, thrombo- embolic deterrant (TED) stockings, as well as Foley catheter insertion was mandatory prior to embolization. Peri procedure Patient Controlled Analgesia (PCA) with a Lock-out time of 10 minutes was used, in the presence of regular blood pressure, temperature, respiratory and oxygen saturation monitoring. Pre-procedure intravenous Cefazolin and per rectal Diclofenac were given, and once the patient was on the procedure bed, intravenous Midazolam: 0.5mgs, Fentanyl: 25 micrograms, and 10 milligrams of Metocloprpamide were injected.
The Barbeau Test was then conducted on the left arm, to assess the Ulno- Palmer vessel patency. With the arm positioned at 70-90 degrees, wrist hyperextendedand in addition to support by towels, and after disinfection by Chlohexidine, lignocaine (2%) and nitroglycerine ointment were applied and an 18-21 gauge needle was fixed under ultrasound guidance. A 0.035 Access Guidance wire (with hydrophilic coating) and then a 5 F catheter (BERN, impress) were introduced into the radial artery. Once the sheath was in place, a cocktail made up of Heparin 1000 Units, nitroglycerin 200 mgs and Verapamil 2.5 mgs was injected slowly intra- arterially. With the Glidewire - catheter combination and with access to right and left uterine arteries, Embosphere (500 micrometers, Embozene: Color Advanced microspheres) particle embolization was done in 20 patients and 500-700 micrometer Polyvinyl Alcohol (PVA) was used on the remaining 3 female participants. Satisfactory stasis of the blood flow was illustrated by post Embolization arteriogram of the uterine arteries. Transradial bands were applied for hemostasis, after sheath removal. Further observation for bleeding, hematoma formation and peripheral pulse at the incision point was conducted, with strict instructions of non-bending or lifting of the forearm for a period of six hours, after which the wrist pressure band was removed. An additional sedation in the form of intravenous Paracetamol was available, if needed, after P.C.A discontinuation. On the following day, oral Diclofenac was prescribed for five days, as needed, and a prophylactic dose of Enoxaparin given. A two to three weeks appointment was then arranged for follow-up and booking of MRI repetition. Measurement of the dominant fibroid on MRI was done before and after the procedure and percentage reduction calculated.
In this study the ages of the patients ranged from 20 to over 52 years, with an average of 39 years. 70% were in the age groups 30-49.9 years and 22% were in the age group of 20-29.9 years, whereas 8% were over 50 years of age. Out of the 23 patients there were 26% single, 61% married and 13% separated. 74% of cases were electively admitted, as arranged, from outpatient clinics and 26% were on emergency basis because of acute symptoms. Out of both married and separated patients, 30% had no children, 26% had history of one to two miscarriages. 30% had four to six children. 9% had more than seven children and 5% had two children only. The height of the patients ranged from 130- 172 cm, with an average of 157 cm. The patients’ weight ranged from 48-91 kgs. With these parameters the Body Mass Index (BMI) was calculated in kgs/m2. The BMI values were stratified into groups arranged as follows: group A was made of BMI 15-19.9 and 20-24.9 kg/m2.
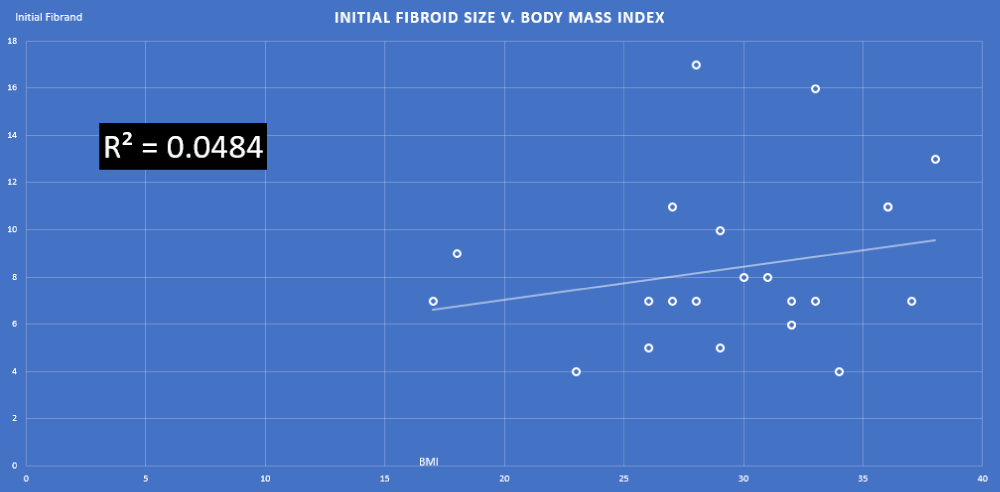
The patients in group B was composed of the BMI 25-28.9, 29- 31.9, & 32- 36.9 kg/m2. The third group C contained those with BMI of 37- 39.9 kg/m2. The BMI values were correlated to the degree of fibroid reduction, where in group A, 13% had reduction of fibroid size by 50% - 70%. In group B, 78% had a reduction by 30% - 65%. In group C, 30% - 50% reduction was seen in 9% of cases. In figure 1, r2= 0.0484 value revealed a poor correlation between Body Mass Index and percentage reduction of fibroids. 78% of patients were between the age groups 30- 52 years of age and were mainly in categories B and C of BMI and had an average percentage reduction of fibroids by 30-70%. Younger patients in the age range of 20-29.9 years made up to 22% of the population and were in category B of BMI and with percentage reduction of 30% - 65%. The patients with no living children made up 57% of cases and out of these 85% were in category B & C of BMI, with a percentage reduction of 30% - 65%.
Figure 1: Correlation between the Body Mass Index and percentage reduction of fibroid.
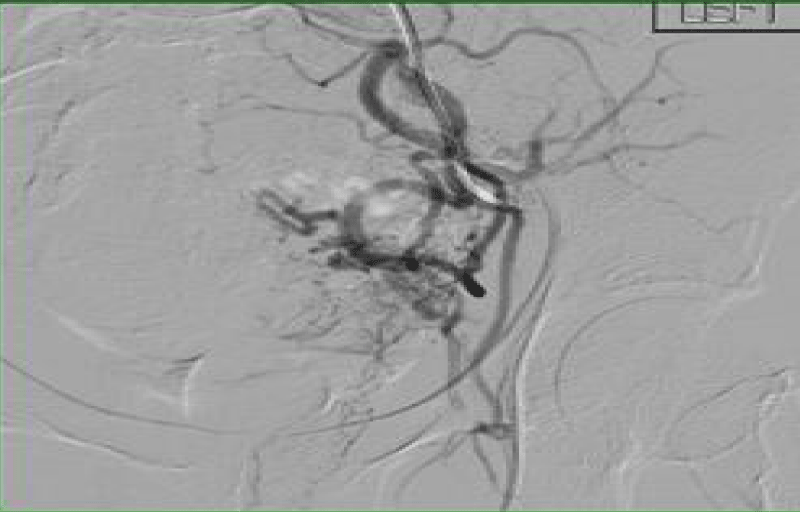
Figure 2: Digital Subtraction Angiography of pelvic arteries showing left hypertrophied uterine artery supplying the fibroid.
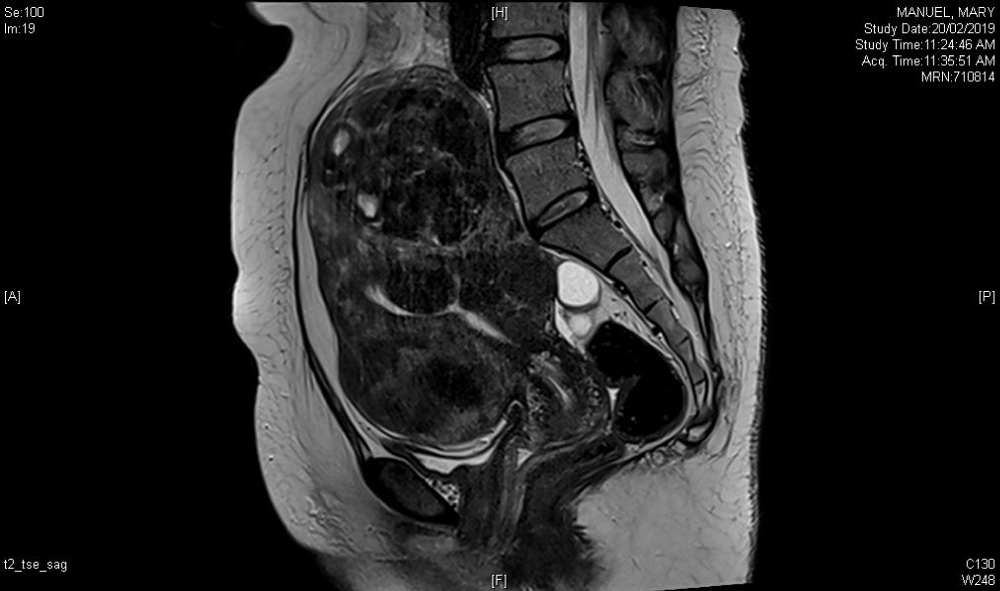
Figure 3: Contrast enhanced MRI for 43 years old patient before uterine artery embolization.
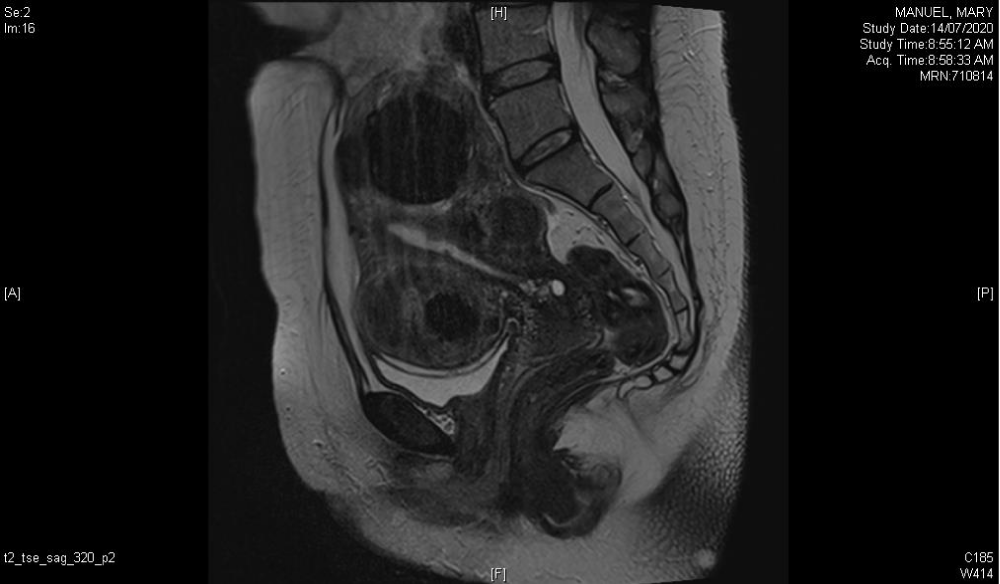
Figure 4: Contrast enhanced MRI of the same 43 year lady, with changes seen eight months post embolization.
The remaining 15% were in the A category with 50% - 70% reduction in fibroid size. 35% of patients with BMI groups A and B & who had a 30% - 70% reduction in size of fibroid were those with a parity of 1-6. Those with 7-9 children were in category B & C of BMI with a percentage reduction of 30% - 65%
of size of fibroid. Table 1 shows the degree in percentage reduction of fibroids in relation to the number of fibroid and BMI. Generally, there was found to be a poor correlation where r2 = 0.036. The table shows the relationship of fibroid sites and degree of percentage reduction post- embolization as seen in the fibroids in the fundal (F), cervical (Cx), and in anterior, posterior and lateral (o) position. There were pedunculated ones as well. A combination of these sites was also encountered. Degenerative changes seen in radiological studies existed in 30% of cases and were in categories A & B of BMI and had 30% - 70% reduction in size of fibroids. This included patients that had these changes before and after the procedure. Three patient had elevated Follicle Stimulating and Luteotropic hormones, which exceeded a value of 10, and were 22, 24 and 45 years in age, with a percentage reduction of 40% - 52% in fibroid size. There were two cases of co-existent adenomyosis with the fibroids, 41 & 42 years of age and had percentage reduction of fibroid by 40% - 50%. One patient had previous myomectomy and had 50% reduction in size of the fibroid (Figures 2-4).
| Table 1: Correlation of fibroid number and site with the degree of Fibroid reduction. | |||
| BMI | |||
| No. of Fibroids | 15-24.9 (A) | 25-36.9 (B) | 37-39.9 (C) |
| 1 | - | 7 | 1 |
| 2 | 1 | 4 | 1 |
| 3 | 2 | 5 | 1 |
| >4 | - | 1 | - |
| Total | 3 | 17 | 3 |
| % of Fibroid reduction | 50-70% | 30-65% | 30-50% |
| Anatomical site | |||
| Fundal (F) | - | 4 | 2 |
| Cervical (Cx) | - | - | - |
| Ant. Post. Lateral(O) | 1 | 11 | 1 |
| Pedunculated | - | 3 | - |
| F + Cx | - | 1 | - |
| F + O | 1 | 1 | - |
| Cx + O | 1 | 1 | 1 |
| Degenerative Changes | 1* | 6*#@ | - |
| *Degenerative changes during pre-procedure (2 patients) #Degenerative changes before & after procedure @Degenerative changes after procedure |
|||
In table 2 it is observed that there was a weak correlation between BMI and initial fibroid size where r2= 0.048. Study of the anatomical and histological layers of the uterus revealed that 65% of patients had intramural fibroids (I.M) with the majority being in category C of BMI, followed by A and then B consecutively and the reduction size achieved was from 30% - 70%. Subserous (S.S) and submucous (S.M) types of fibroids were seen in 13% of cases, were in B & C categories of BMI and with a percentage reduction of 30% - 65%. A combination of subserous, intramural and submucous fibroids was seen in 4% of cases, in category B of BMl and with a percentage reduction of 30% - 65%.
| Table 2: Correlation of the size and anatomical site of fibroids with the degree of fibroid reduction. (N = 23 patients). | ||||
| BMI | ||||
| Size of Fibroid (cm.) |
15-24.9 (A) | 25-36.9 (B) | 37-39.9 (C) | TOTAL |
| 2-6.9 | 2 | 4 | - | 6 |
| 7-11.9 | 5 | 3 | 6 | 14 |
| 12-14.9 | - | - | 1 | 1 |
| >15 | - | 1 | 1 | 2 |
| TOTAL | 23 | |||
| % of Fibroid reduction | 50-70% | 30-65% | 30-50% | - |
| Anatomical site (Histological) | ||||
| I.M | 3 | 4 | 8 | 15 |
| I.M + S.S | - | 1 | - | 1 |
| S.S | - | - | 1 | 1 |
| S.M | - | 1 | - | 1 |
| S.S + I.M | - | 1 | - | 1 |
| S.S + S.M | - | 2 | 1 | 3 |
| All types | - | 1 | - | 1 |
| TOTAL | 3 | 10 | 10 | 23 |
| I.M: Intramural; S.S: Subserosal; S.M: Submucosal fibroids | ||||
The main presentation of fibroids was in the form of abdominal mass and discomfort in 52% of cases, abnormal bleeding presenting as menorrhagia in 70% and metrorrhagia in another 48% group of cases. Recurrent anemia made up to 43% of the presentations, 17% had intermittent abdominal pain and 17% complained of pressure symptoms.
Infertility was the main problem in 26% of cases, dysmenorrhea in 9% and urinary frequency and incontinence was the problem in 4%.
Associated medical disorders seen in the population studied included diabetes mellitus in 17%, hypothyroidism in 9%, 13% hypertension and 9% dyslipidemia in cases. The hematological disorders encountered were in 9% of cases where one had sickle cell disease, and another was with symptomatic protein S deficiency manifested by history of repeated venous and pulmonary emboli. 17% had gastrointestinal disorders including diverticulosis, peptic ulcer, gastritis, hepatitis and hepatomegaly. 9% had depression, 4% amyloidosis, and 9% had severe bronchial asthma.
Previous surgical procedures done for such patients included cesarean section in 17% and dilatation and curettage in 4% of cases. Other surgical (interferences) included appendectomy, tonsillectomy and two patients had operations: One for breast cancer and one for thyroid cancer. Further, other operations included myomectomy, sleeve gastrectomy and laparotomy. Two patients had Polycystic ovary syndrome and another had bilateral Fallopian tube dilatation.
The pre-procedure time frame of follow-up of the patients due to fibroid existence ranged from one to eight years. During that period the patients received various forms of treatment, where 30% of cases had blood transfusion and 43% received intravenous iron. 20% of patients used Non - steroidal Anti- inflammatory medication, 70% used Tranexamic acid (Cyklokapron), and 17% used Gonadotropin - releasing hormone analogs. In turn, oral contraceptives were tried by 52% of the patients. Oral progesterone in the form of Dydrogesterone and Norethindrone Acetate was used by 57% of cases and 13% were prescribed Dienogest. Intrauterine devices with Levonorgestrel was used in 4% of cases. Daflon (Diosmin & flavonoids) was also tried with 52% of patients.
26% of the patients were employed and 45% had Higher Education. There were no illiterate patients. The pre- procedure hemoglobin level was in the range of 5.0- 6.8 g/ dl. In 22% of cases and 7-9.9 g/dl in 78% of the remaining patients. The three months post-procedure hemoglobin level became 10-11.9g/dl in 83% of cases, 12-13.9 g/ dl in 13% and even reached a level of 14-15.9 g/ dl in 4% of cases. This was due to the significant reduction of previous persistent bleeding. The length of hospital stay was 2-4 days for almost 87% of cases, except for 13% where it was 5-6 days for cases that were urgently admitted with bleeding and anemia and kept in for management, due to social and geographical reasons.
The time taken from immediate pre-procedural preparation until completion of the embolization was on the average 70-89.9 minutes for 65%, 50-59.9 minutes for 9%. Whereas 26% of cases needed 90-119 minutes because of technical reasons surrounding the procedure setup and not due to the procedure itself. The exact time of exposure to fluoroscopy was not registered. The same interventional radiologist performed all the procedures, where both the right and left uterine arteries were successfully accessed and blocked.
Table 3 shows the early and delayed complications of the procedure where there was an observed reduction in the percentage on comparison of namely: nausea alone, as well as in association with vomiting, abdominal pain, vaginal discharge and per vaginal spotting. One patient, 4%, had non anemic dizziness around the time of the procedure that spontaneously abated. Sloughing of necrotic tissue, fever, and signs of infection were all evident in one patient who was admitted, covered by antibiotics and had initial partial removal of pedunculated fibroid exiting through the cervical opening. Eventually, that same fibroid, ended in spontaneous complete expulsion, within three weeks. Post Embolization syndrome was seen in 4% of patients and managed by symptomatic treatment.
| Table 3: Early and Delayed Post embolization Complications (n = 23 patients). | ||||
| Signs and Symptoms | Early | % | Delayed | % |
| Nausea only | 4 | 17 | - | - |
| Nausea & Vomiting | 4 | 17 | - | - |
| Abdominal Pain | 9 | 39 | 3 | 13 |
| Fever | - | - | 1* | 4 |
| Vaginal Discharge | 8 | 35 | 5 | 22 |
| Dizziness (non-anemic) | 1 | 4 | - | - |
| Sloughing of tissue | 1* | 4 | 1* | 4 |
| Post embolization syndrome | 1 | 4 | - | - |
| Pain in flanks | 1 | 4 | 1 | 4 |
| Pain in arm | 1 | 4 | 1 | 4 |
| Epigastric Pain | 1 | 4 | - | - |
| Urinary symptoms | 1 | 4 | - | - |
| P/V spotting | 8 | 35 | 2 | 9 |
| Amenorrhea | - | - | 1 | 4 |
| *Same patient. | ||||
Flank pain was seen in one patient in early and delayed complication period of the study, which was uneventful post-investigations. The left arm pain and epigastric pain experienced in two different patients was managed by a multidisciplinary team and settled down by symptomatic treatment.
Dysuria was experienced in one patient as an early, and amenorrhea in another patient as a delayed complication.
Pre-procedure Luteinizing and Follicle Stimulating Hormones requested were done by only 13 patients and found to be elevated in three cases (A cut off value of 10 or more was considered). Post procedure repetition was done by only 3 candidates.
Tran- radial Uterine Artery Embolization is a relatively recent minimally invasive method and a breakthrough in the conservative management of symptomatic patients. The candidates for its indication are those refusing surgical options out of sheer fear or because of co-existing high-risk medical status. Further reasons might be due to religious beliefs, taboos and cultural concerns for uterine conservation.
Our experience agrees with Gjoreski, et al. [1] in the comparison of routes used, where it was evident that the Trans- Femoral route in comparison to the Trans-radial one, took longer time to perform, was associated with more exposure to fluoroscopy, increased demand on post procedure site physical pressure for hemostasis and possibly more length of hospital stay. In accordance, the trans- radial route gained increased popularity amongst the treating physicians as well as the patients.
The degrees of percentage reduction of fibroids in our study ranged from 30% - 70%, with an average of 49%. This figure is almost akin to Coleman, et al. [7], more than O’Grady, et al. of 40.0% [11] but lesser than the high percentages of 68% achieved by Anderson, et al. [2]. However, the completed five-year follow-up is yet to be awaited before the final effect of Embolization in our study is apparent & so far, the first two important years were analyzed.
The length of hospital stay in our study was longer than other studies [1], and that can be explained by our strict adherence and following of the meticulous protocol of our institute provided for pain management and prophylactic measures set to avoid infection and thrombosis. However, with the good outcome, increased demand on the procedure and acquired experience, a shift to short hospital stays rather than the current prolonged one can be implemented in future.
The consumption time of Patient Controlled Analgesia (PCA) in our studied population never exceeded 18 hours, and which is probably due to the pain experienced due to ischemia of the uterus, resulting from occlusion of second uterine artery at the occurrence of the procedure, which is estimated to last 12-18 hours [20].
With regards to the complications encountered in the form of lessening vaginal discharge, post - embolization syndrome fibroid expulsion and amenorrhea in a 45-year-old patient, are all lesser than other studies [11,13,14,17]. In fact, Laios, et al. [19] considered these presentations as an expected normal consequence of any embolization process done and not a complication per se.
Adherence to the mentioned procedure protocol was a major reason of the well achieved outcome, despite the presence of high-risk patients including one with previous thrombotic attacks and another with bilateral dilated Fallopian tubes. Many contents of that protocol were shared by Spies, et al. [17].
We encountered an isolated case of left arm pain that was eventually relieved by symptomatic treatment and most probably was not related to the procedure and is not a reason to change our policy like Gjoreski, el al. [1] where routine ultrasound check up of the radial artery, one month post-procedure was done to check on arterial patency .
Patients seeking pregnancy were thoroughly counseled with regards the, yet, unclear definitive outcome on ovarian reserve and fertility outcome post procedure. Further information in the case of occurrence of pregnancy were embarked on with the patients, including recurrent abortions, premature birth, increased cesarean section rate, placental accidents and postpartum bleeding.
Almost 70% of our young and older premenopausal patients with intramural fibroid of size range of 2-15 cm had a degree of percentage reduction similar to that of Czuczwar, et al. [3], who reported greater volume reduction of this type of fibroid in premenopausal women. On the other hand, Spies, et al., Naguib, et al. and Jha, et al. [24-26] believe that sub-mucous fibroids shrink to a greater extent than intra mural and sub-serous ones. In addition, Sasa, et al. [28] documented that there was an even better outcome with Leiomyomas less than 7 cm in size. In fact Mailli, et al. [33] described migration of small intra mural fibroids with a maximum diameter of 5.4 cm towards the endometrial cavity of the uterus after uterine artery embolization, a fact that would explain the vaginal discharge and expulsion associated with such fibroids, which was seen with one of our cases.
The inclusion of two patients with adenomyosis and with good reduction in size and symptoms was a positive point in our study and opened a new avenue for the management of such patients. This finding agrees with Dariushnia, et al. [12] and Siskin, et al. [36]. However, it conflicts with earlier studies of Mclucas, et al. [31], who expressed that the mere presence of adenomyosis increased the failure rate of fibroid size reduction by up to 50% in patients managed by embolization. Fundal fibroids, seen in 40% of cases illustrated good response in size and symptoms. The findings come within the purview of Kim, et al. [32], who showed that there was significant necrosis in embolized fundal fibroids than those in the cervical area. Firouznia and de Souza, et al. [22,23] found no correlation between fibroid location and reduction of fibroid size in patients managed by Embolization In addition, Lohle, et al. [21] revealed no correlation between patient age and degree of fibroid reduction and which agreed with our data.
Yamashita, et al. [37] pointed out that degenerative changes in Leiomyomas seen in MRI with high T2 signal was indicative of greater volume reduction on embolization .In our study we encountered two out of seven cases that had such similar changes and had a percentage reduction in fibroid size by 30% - 46%. Other changes that warrant studying, are the findings associated with low signal intensity on T2 images, encountered in some cases, which probably might be indicative of non-degenerate or myxoid changes in the fibroids. Bigger studies are needed to help understand the significance of these changes.
The 20% - 30% recurrence of symptoms post-embolization and with the availability of voluminous data illustrating the correlation of several factors affecting the outcome, Gjoreski, et al. [1] suggested the study of the heights of patient as a prognostic factor for the outcome. In an analogous manner, we tried to review a factor, which was not encountered before in the literature, that demonstrates the relationship between Body Mass Index of patients and its correlation with the percentage reduction of fibroid size. This fact was considered after noticing more decrease in fibroid size in patients with low body mass indices in comparison with those having higher parameters. However, this relationship together with age and numbers of fibroids were weakly correlated in our study. A possible explanation might probably be due to the small sample size analyzed.
These findings warrant future bigger studies, with the help of other international data to help in the construction, enumeration and stratification of a method in an algorithmic manner. This can be used at the pre- procedure counseling sessions, where rejection due to irrelevance of the procedure might be decided, hence saving the cost and avoidance of psychological trauma to the patient.
Recommended availability of easy access of follow-up for the treated patients, where a biennial or triennial MRI versus 3D ultrasound, should be part of the scheme of follow-up for detection of any ‘silent’ changes in quiescent fibroids.
Although our success rate was within the international figures of fibroid size reduction, a hypothetically higher percentage might have been achieved. The probable factors that could have led to such a lower percentage of success, might be due to the inclusion of older patients including age groups 40-52, which made up to 61% of cases, and where in that aspect Czuczwar, et al. [3] stated that the percentage of fibroid reduction was lowered by 13% for every ten year increase in age, being proportional to estrogen receptors availability, that depreciates with age. Further, incorporating big fibroids in our study maybe another additional factor. In elaboration, according to Lipscomb, et al. [39] fibroids larger than 8.7 cm showed lesser reduction in size where stated each centimeter increase in fibroid size there was a corresponding 10% increase in failure rate. Having multiple fibroids per se is another cause, as El-Sharkawy, et al. [40] observed a significant reduction in single rather than multiple fibroids.
Total fibroid volume change measurements are preferable to a single dominant fibroid volume study, for the detection of percentage reduction, since clinical relevance and symptoms are the result of the summation of all available fibroids and not a single entity.
This form of fibroid management is rapidly gaining popularity and represents a florid area for excellence of treatment backed by bigger studies, targeting improvement of the outcome, by careful patient selection, based on strict criteria.
Trans-radial uterine artery embolization is a highly attractive, and effective minimally invasive method of management of symptomatic patients with fibroids, who refuse other modes of treatment.
A major drawback to this treatment is the recurrence of symptoms in almost one third of patients, who undergo embolization.
Careful pre-procedural counseling should be done, with a briefing on the recurrence rate, and future algorithmic tables should be constructed so patients can be directed to alternative and suitable treatments, to reduce expenses and avoid psychological trauma.
Treatment facilities should have post-procedural follow-up and treatment for recurring symptoms. Additionally, radiological backup studies should be available for long-term follow-up for early detection of changes in ‘quiescent ‘fibroids, in spite of the rare occurrence of malignant changes.
- Gjoreski A, Gjoreski J, Nancheva A. Uterine Fibroid Embolization via Transradial versus Tran femoral Arterial Access: Technical Results. Open Access Maced J Med Sci. 2019; 7: 579-582. PubMed: https://pubmed.ncbi.nlm.nih.gov/30894915/
- Anderson PE. Uterine Artery Embolization of symptomatic uterine fibroid- Initial success and short-term results. Acta Radiologica. 2001; 42: 234-238.
- Czuczwar P, Wozniak S, Popajewski M: Predicting the results of uterine artery embolization: correlation between initial intramural fibroid volume percentage decrease. Menopause Review (Prseglad/Menopauzalny). 2014; 13: 247-252. PubMed: https://pubmed.ncbi.nlm.nih.gov/26327862/
- Freed MM, Spies JB. Uterine artery embolization for fibroids: a review of current outcomes. Semin Reprod Med. 2010; 28: 235-241. PubMed: https://pubmed.ncbi.nlm.nih.gov/20414846/
- Van der Kooij SM, Hehen Kamp WJK, Volkers N A, Birnie E, Ankum W M, Reekers J.A. Uterine artery embolization vs hysterectomy in the treatment of symptomatic uterine fibroid: 5-year outcome from the randomized EMMY trial. Am J Obstet Gynecol. 2010; 203: 105-113. PubMed: https://pubmed.ncbi.nlm.nih.gov/20579960/
- Moss JG, Cooper KG, Khaund A. Randomized comparison of uterine artery embolization (UAE) with surgical treatment in patients with symptomatic uterine fibroids (REST trial): 5-year results. BJOG. 2011; 118: 936-944. PubMed: https://pubmed.ncbi.nlm.nih.gov/21481151/
- Coleman P, Ayiku L, Nicholl J. Systemic review of the efficacy & safety of uterine artery embolization in the treatment of fibroids. Sheffield: Review Body for Interventional Procedures. 2004.
- Volkers NA, Hehenkamp WJK, Birnie E. Uterine artery embolization versus hysterectomy in the treatment of symptomatic uterine fibroids: 2 years outcome from the randomized EMMY trial. Am J Obstet Gynecol. 2007; 196: 519. PubMed: https://pubmed.ncbi.nlm.nih.gov/17547877/
- Hehen Kamp WJK, Volkers NA, Birnie E, Reekers JA, Ankum WM. Symptomatic uterine fibroids: treatment with uterine artery embolization or hysterectomy results from the randomized clinical embolization versus hysterectomy (EMMY) trial. Radiology. 2008; 246: 823-832. PubMed: https://pubmed.ncbi.nlm.nih.gov/18187401/
- Spies JB, Bruno J, Czeyda-Pommer Sheim F, Magee ST, Ascher SA, et al. Long term outcome of uterine artery embolization of Leiomyomata. Obstet Gynecol. 2005; 106: 933-939. PubMed: https://pubmed.ncbi.nlm.nih.gov/16260509/
- O Grady EA, Moss JG, Belli AM, Thomas S, Nicholl J, et al. UK Uterine artery embolization for fibroids registry 2003-2008. The British Society of Interventional Radiology & School of Health and related research.
- Dariushnia S, Nikolie B, Strokes L, Spies J. Quality improvement Guidelines for uterine Artery Embolization for Symptomatic Leiomyomata. J Vasc Interv Radiol. 2014; 25: 1737-1747. PubMed: https://pubmed.ncbi.nlm.nih.gov/25442136/
- Hirst A, Dutton S, Wu O, Briggs A, Edwards C, et al. A Multi-Centre retrospective cohort study comparing hysterectomy and uterine artery embolization for the treatment of symptomatic uterine fibroids. The HOPEFUL Study. 2008; 12: 1-248. PubMed: https://pubmed.ncbi.nlm.nih.gov/18331704/
- Clinical recommendation on the use of uterine artery embolization (UAE) in the management of fibroids. Royal College of Obstetrics and Gynecologist and the Royal College of Radiologist. 3rd edition. 2013.
- Schirf BE, Vogelzang RL, Chrisman HB Complications of Uterine Fibroid Embolization. Semin Intervent Radiol. 2006; 23: 143-149. PubMed: https://pubmed.ncbi.nlm.nih.gov/21326757/
- Payne JF, Haney AF. Serious complications of uterine artery embolization for conservative treatment of fibroids. Fertility and Sterility. 2003; 79: 128-131.
- Spies JB, Myers ER, Worthington-Kirsch R, Mulgund J, Goodwin S, et al. The Fibroid registry: symptom and quality of life status 1 year after therapy. Obstet Gynecol. 2005; 106: 1309-1318. PubMed: https://pubmed.ncbi.nlm.nih.gov/16319257/
- Moss J. Christie A. Uterine artery embolization for heavy menstrual bleeding. Women Health (Lond). 2016; 12.71-77. PubMed: https://pubmed.ncbi.nlm.nih.gov/26756068/
- Laios A, Baharuddin N, lliou K, Gubara E, O’Sullivan G. Uterine artery embolization for treatment of symptomatic fibroids; a single institution experience. Hippokratia; 2014; 18: 258-261. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4309148/
- Lund N, Justesen P, Elle B, Thompson SG, Floridon C. Fibroids treated by uterine artery embolization. A review. Acta Obstet Gyecol Scand. 2000; 79: 905-910.
- Lohle PN, Voogt MJ, De Vries J, Vervest HAM, Lampmann LEH, et al. Long term outcome of uterine artery embolization for symptomatic uterine Leiomyomata. Journal of vascular Intervent Radiology. 2008; 19: 319-326. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2933812/
- Firouznia K, Ghanaati H, Jalali AH. Uterine artery embolization in 101 cases of uterine fibroids: Do size, location and number of fibroids affect therapeutic success and complications? Cardiovascular and Interventional Radiology. 2008; 31: 521-526. PubMed: https://pubmed.ncbi.nlm.nih.gov/18219521
- de Souza NM, Williams AD. Uterine arterial embolization for Leiomyomas: Perfusion and volume changes at MR imaging and relation to clinical outcome. Radiology. 2002; 222: 367-374. PubMed: https://pubmed.ncbi.nlm.nih.gov/11818601/
- Spies JB, Roth AR, Jha RC, Gomez-Jorge J, Levy EB, et al. Leiamyomata treated with uterine artery embolization: factors associated with successful symptom and imaging outcome. Radiology. 2002; 222: 45-52. PubMed: https://pubmed.ncbi.nlm.nih.gov/11756703/
- Naguib NNN, Mbalisike E, Nour-Eldin NA, Jost A, Lehnert T, et al. Leiamyoma volume changes at follow up after uterine artery embolization. Correlation with the initial leiomyoma volume and location. J Ascher Interv Radiol. 2010; 21: 490-495. PubMed: https://pubmed.ncbi.nlm.nih.gov/20149688/
- Jha RC, Ascher SM, Imoaka I, Spies JB. Symptomatic fibroleiomyama: MR imaging of the uterus before and after uterine artery embolization. Radiology. 2000; 217: 228-235. PubMed: https://pubmed.ncbi.nlm.nih.gov/11012449/
- Sweets AJ, Nijenhuis RJ, Rooij WJ, Weimar EAM, Boekkooi PF, et al. Uterine artery embolization in patients with a large fibroid burden: long term clinical and MR follow up. Cardiovasc Intervent Radiol. 2010; 33: 943-948. PubMed: https://pubmed.ncbi.nlm.nih.gov/20066419/
- Sasa H, Kaji T, Furuya K. Indications and outcome of uterine artery Embolization in patient with Uterine Leiomyomas. Obstet and Gyncol International. 2012; Article ID 920831. PubMed: https://pubmed.ncbi.nlm.nih.gov/22135681/
- Siskin GP, Tublin ME, Stain Ken BF, Dolen EG, Dowling K. Uterine Artery Embolization for the treatment of Adenomyosis. Clinical response and evaluation with MR imaging. Am J Roentgenol. 2001; 177: 297-302. PubMed: https://pubmed.ncbi.nlm.nih.gov/11461849/
- Carrillo TC. Uterine artery embolization in the Management of symptomatic uterine fibroids: An overview of complication and follow up. Semin Intervent Radiol. 2008; 25: 378-386. PubMed: https://pubmed.ncbi.nlm.nih.gov/21326579/
- Mclucas B, Adler L, Perrella R. Uterine fibroid embolization: nonsurgical treatment for symptomatic fibroids. J Am College Surg. 2001; 19: 195-105. PubMed: https://pubmed.ncbi.nlm.nih.gov/11192931/
- Kim MD, Lee M, Jung DC, Won JY, Lee DY, et al. Limited Efficacy of Uterine Artery Embolization for cervical Leiomyomas Clinical Study. 2012; 23: 236-240. PubMed: https://pubmed.ncbi.nlm.nih.gov/22177843/
- Mailli L, Auyoung EY, Angileri SA, Renani SA, Ratnam L, et al. Predicting the fibroid Migratory Impact of UAE: Role of Pre embolization MRI characteristics. Cardiovascular Interventioal Radiology. 2020; 43: 453-458. PubMed: https://pubmed.ncbi.nlm.nih.gov/31650245/
- Tulandi T. Fertility and Uterine artery embolization. Obstet Gynecol. 2010; 116: 439-440.
- Aziz A, Retrucco OM, Makinoda S. Trans arterial embolization of the uterine arteries, patient reactions and effects on Uterine vasculature. Acta obstet Gynecol Scand. 2003; 77: 334-340. PubMed: https://pubmed.ncbi.nlm.nih.gov/9539283/
- Siskin GP, Tublin ME, Stainken I, Dawling K, Dolen EG. Uterine Artery Embolization for the treatment of Adenomyosis. Clinical Response and Evaluation with MRI imaging. Am J Roentgenol. 2001; 177: 297-302. PubMed: https://pubmed.ncbi.nlm.nih.gov/11461849/
- Yamashita Y, Torashima M, Takahashi M, Tanak N, Katabuchi H, et al. Hyper intense uterine leiomyoma at T2 weighted MR imaging: differentiation with dynamic enhanced MR imaging and clinical implications. Radiology. 1993; 189: 721-725. PubMed: https://pubmed.ncbi.nlm.nih.gov/8234695/
- Spies JB, Bruno J, Czeyda-Pommersheim F, Magee ST, Ascher SA, et al. Long term outcome of uterine artery embolization of Leiomyomata. Obstet Gynecol. 2005; 106: 933-939. PubMed: https://pubmed.ncbi.nlm.nih.gov/16260509/
- Limpscomb GH. Uterine Artery Embolization and Minimally Invasive Techniques for Uterine Fibroids. The global Library of Women’s medicine. 2008.
- Elsharkawy AM, Elsaeed HH, Kamel AH, Morgan R, El Shafey MH. Comparison between the outcome of single versus multiple uterine fibroids after uterine artery embolization. Egyptian J Radiol Nuclear Med. 2020: 51-77.