More Information
Submitted: 12 October 2020 | Approved: 27 November 2020 | Published: 30 November 2020
How to cite this article: Sharma B, Deep J, Pandit C, Basnyat B, Khanal B, et al. Overview on current approach on recurrent miscarriage and threatened miscarriage. Clin J Obstet Gynecol. 2020; 3: 151-157.
DOI: 10.29328/journal.cjog.1001070
Copyright License: © 2020 Sharma B, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Miscarriage; Pregnancy; Recurrent; Threatened
Overview on current approach on recurrent miscarriage and threatened miscarriage
Basant Sharma1*, Jagat Deep2, Chandrika Pandit3, Bina Basnyat4, Bandana Khanal5, BB Raut6, Brij Mohan Rajak7, Deepak Patel8, Rangina Laikangbam9 and Rajendra Basyal10
1Assistant Professor, Obs/Gyne, Citwan Medical College, Narayanghat, Nepal
2HOD, National Medical College, Birjung, Nepal
3Senior Consultant, Obs/Gyne, Fewa City Hospital, Pokhara, Nepal
4Senior Consultant, Obs/Gyne, Valley Maternity Hospital, Kathmandu, Nepal
5Assistant Professor, Obs/Gyne, Citwan Medical College, Narayanghat, Nepal
6Senior Consultant, Obs/Gyne, Lumbini Zonal Hospital, Butwal, Nepal
7Senior Consultant, Obs/Gyne, Specializtion in Infertility, Janakpur Zonal Hospital, Janakpur, Nepal
8Consultant, Obs/Gyne, Siddharthanagar City Hospital, Bhairawha, Nepal
9Infertility Specialist, Obs/Gyne, Bluecross Hospital, Kathmandu, Nepal
10HOD, Siddhartha Children and Women Hospital, (AMDA) Butwal, Nepal
*Address for Correspondence: Basant Sharma, Assistant Professor, Obs/Gyne, Citwan Medical College, Narayanghat, Nepal, Tel: 9313533877; 9810360174; Email: [email protected]
Miscarriage is a frequent outcome of pregnancy, with major emotional implications to the couple experiencing such an event. Threatened miscarriage is the commonest complication of early pregnancy and affects about 20% of pregnancies. It presents with vaginal bleeding with or without abdominal cramps. On the other hand recurrent miscarriages are post implantation failures in natural conception. Increasing age of women, smoking, obesity or polycystic ovary syndrome (PCOS) and a previous history of miscarriage are risk factors for threatened miscarriage. The pathophysiology has been associated with changes in levels of cytokines or maternal immune dysfunction. Clinical history and examination, maternal serum biochemistry and ultrasound findings are important to determine the treatment options and provide valuable information for the prognosis. Many surgical and non-surgical interventions are used in the management of threatened and recurrent miscarriages. In this review, we present available evidence-based guidance on the incidence, pathophysiology, investigation and clinical management of recurrent miscarriage and threatened miscarriage, focusing mainly on the first trimester of pregnancy and primary healthcare settings. The review is structured to be clinically relevant. We have critically appraised the evidence to produce a concise answer for clinical practice.
Miscarriage is defined as the spontaneous loss of pregnancy before the fetus reaches viability. The term therefore includes all pregnancy losses from the time of conception until 24 weeks of gestation [1]. Early miscarriage is experienced by women globally and is considered to be a universally traumatic and distressing experience. The definition of early miscarriage is defined by the Royal College of Obstetrics and Gynaecologists (RCOG 2006) as loss within the first 12 completed weeks of pregnancy [2].
Recurrent miscarriage
Recurrent miscarriage (RM) affects 1% of all women. It is defined as the occurrence of three consecutive first trimester losses of pregnancy. It is a very frustrating condition for both the couple and the clinician, because it is rare to find a clear-cut reason for the repeated failure to sustain a pregnancy and, as a consequence, the prospect of a satisfactory treatment [3].
The definition of recurrent pregnancy loss (RPL) has long been debated and differs among international societies [4]. The UK Royal College of Obstetricians and Gynaecologists (RCOG) define RM as ‘the loss of three or more consecutive pregnancies’. The German, Austrian and Swiss Societies of Gynaecology and Obstetrics (DGGG/OEGGG/SGGG) also consider RM as 3 consecutive losses. The American Society for Reproductive Medicine (ASRM), on the other hand, defines RM as ‘two or more failed clinical pregnancies’ (pregnancy in this case requiring ultrasound or histological confirmation) thereby excluding biochemical pregnancies but requiring only two losses [5].
Incidence of recurrent miscarriage
Global risk of miscarriage for a clinically recognized pregnancy is 10% - 15%. However, the actual rates of miscarriage might be higher as many women have very early miscarriages without ever realizing that they are pregnant [6]. Recurrent miscarriage occurs in up to 15% – 20% of apparently normal couples and becomes recurrent in 2% – 3% of these couples [7]. Indeed, the risk is between 9% and 12% in women aged ≤ 35 years, but increases to 50% in women aged ˃ 40 [4]. The risk of further miscarriage increases to approximately 50% for women with three or more losses without a live born infant [5].
Pathophysiology involved in recurrent miscarriage
Anatomic factors
Uterine anomalies, both congenital and acquired, can account for up to 19% of RPLs [8]. Congenital uterine anomalies that potentially cause RPL include unicornuate, didelphic, bicornuate, septate, and arcuate uteri. Acquired anomalies that may contribute to RPL include fibroids, endometrial polyps, and uterine adhesions. Uterine fibroids are the most common of the defects that are acquired, but their role in RPL and management is debatable and may depend on size and location to determine if surgical management is warranted [9].
Thyroid dysfunction and recurrent pregnancy loss
Abnormalities in thyroid function, including hyperthyroidism and hypothyroidism, can have an adverse effect on reproductive health and result in reduced rates of conception, increased early pregnancy loss, and adverse pregnancy and neonatal outcomes. ASRM 2012 have clarified that thyroid stimulating hormone (TSH) above 2.5 uIU/ml are outside the normal range and must be treated. The effect of the physiological changes in pregnancy on the thyroid gland has led to the development of specific reference ranges for thyroid function tests in pregnancy (Table 1) [10].
| Table 1: Reference range of thyroid stimulating hormone TSH. | |
| Trimester | TSH (mIU/L) |
| 1st Trimester | 0.1–2.5 |
| 2nd Trimester | 0.2-3 |
| 3rd Trimester | 0.3–3.5 |
| TSH: Thyroid Stimulating Hormone | |
Genetic factors
After 2 or 3 miscarriages, a genetic evaluation of the products of conception (POCs) and the parents should be considered early in the work-up. In couples with RPL, 3% to 5% have chromosomal abnormalities in 1 of the partners. The most common chromosomal anomaly associated with RPL is a balanced translocation [11].
Endocrine factors
It evolves diabetes mellitus, thyroid antibodies and dysfunction and Hyperprolactinemia. Though diabetes is not a direct cause of RPL but uncontrolled diabetes can cause of congenital anomaly [9].
Inherited thrombotic disorders
Pregnancy itself is known to be a hypercoagulable state. Additionally, thrombophilias are responsible for more than 50% of maternal venous thromboembolisms during pregnancy [9].
The recommended evaluations are as follows: [12].
• Factor V Leiden screening with activated protein C (APC) resistance using a second-generation coagulation assay is probably the most cost-effective approach. Patients with a low APC resistance ratio (<2.0) should then be genotyped for the factor V Leiden mutation.
• Protein S activity with normal levels between 60% and 145%.
• Protein C activity with normal levels between 75% and 150%.
Investigations
Investigation in recurrent pregnancy loss
Patients with recurrent miscarriages deserve special attention, as the risk of recurrence is higher and the causes tend to be different from sporadic miscarriages [13]. The recommended investigations for recurrent miscarriages are listed in table 2.
| Table 2: Investigation summary for recurrent pregnancy loss. | |||
| Investigations | Yes | Maybe | No |
| Anatomical | Two-dimensional/three-Dimensional Ultrasonography and Sonohysterography or Combination laparosopy and hysteroscopy |
MRI | |
| Genetic | Kartotype: POC | Karyotype: parental | |
| Thrombophilla | Acquired: APS | Anti-b2 glycoprotein | Congenital thrombophilia |
| Infection | LVS/HVS/chlamydia Endometrial biopsy and culture |
Torch | |
| Immunological | Antinuclear antibody | HLA Natural killer cells (research only) |
|
| Endocrinological | TSH (FT ¾ and antibodies if TSH abnormal) | ||
| Male factor | Sperm DNA fragmentation index | ||
| APS: Antiphospholipid Syndrome; β-hCG, beta human chorionic gonadotropin; BMI: Body Mass Index; IMSI: Intracytoplasmic Morphologically Selected Sperm Injection; IVIG: Intravenous Immunoglobulin; LH: Luteinising Hormone; PICSI: Physiological Intracytoplasmic Sperm Injection; TORCH: Toxoplasmosis, Other Agents, Rubella; Cytomegalovirus and Herpes simplex | |||
Anatomical investigation
Many anatomical anomalies have been associated with RPL. Uterine leiomyoma, Müllerian anomalies and uterine synechiae are the most significant. Two-dimensional/three-dimensional ultrasonography with sonohysterography is recommended for couples with two or more pregnancy losses.
Genetic investigation
The RCOG states that cytogenetic analysis should be performed on products of conception (POC) in patients with RPL. Peripheral blood karyotyping of both parents should be performed if the POC have an unbalanced structural chromosomal abnormality. However, the ASRM recommends that all RPL parents should have peripheral karyotyping independently of the POC karyotyping. But Karyotyping of the parents is not routinely recommended because of ongoing pregnancies.
Thrombophylia investigation
RCOG, ASRM, European Society of Human Reproduction and Embryology (ESHRE) guidelines suggest testing for Antiphospholipid syndrome (APS) in RPL. There is also some evidence linking RPL to b2 glycoprotein1 (b2GP1) antibodies; thus, both the ASRM and ESHRE guidelines suggest including b2GP1 antibodies in the investigations.
Investigation of infection
There is evidence that bacterial vaginosis can lead to miscarriage in the second trimester; the evidence for its link to 1st trimester miscarriage is tenuous. Work done in Ureaplasma, Listeria, Chlamydia and Mycoplasma, and toxoplasmosis, other agents, rubella, Cytomegalovirus and Herpes simplex (TORCH) infections has not shown any link to RPL.
Immunological investigation
There is currently no good evidence that immunomodulation has any effect on RPL. Investigations for auto-immunity outside of APS are not recommended.
Endocrinological investigation
Endocrinological associations investigated in the context of RPL include thyroid function, glucose metabolism, polycystic ovary syndrome (PCOS), progesterone and prolactin. All guidelines recommend testing for thyroid-stimulating hormone (TSH) levels, but there is contention about what is considered a ‘normal’ TSH.
Male factor investigation
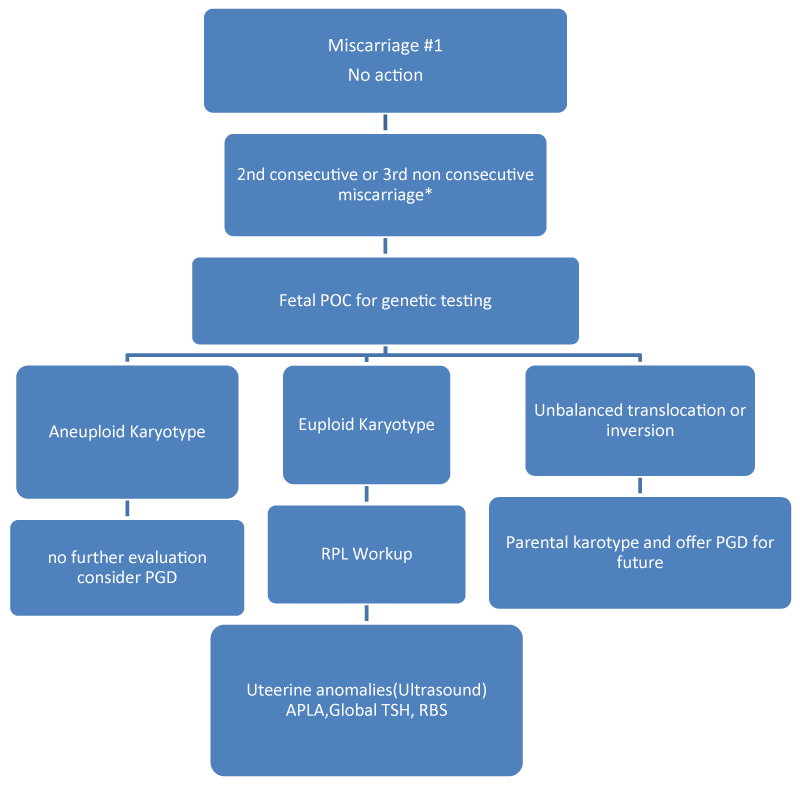
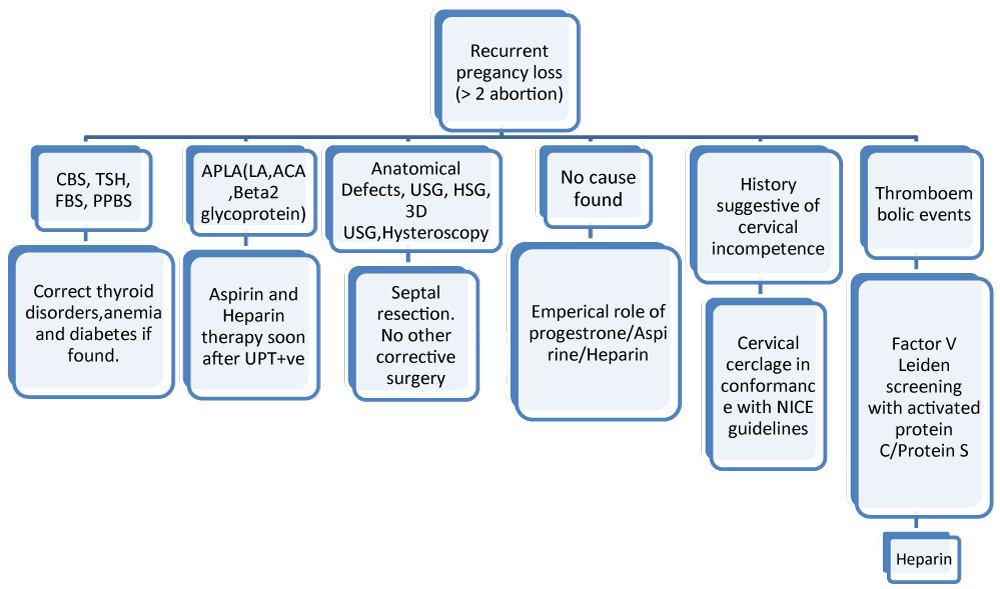
The ASRM guidelines state that routine sperm DNA fragmentation indexing is not indicated because of the weak evidence, but the ESHRE guidelines state that this can be done to provide an explanation for RPL [14]. A new testing evaluation algorithm has been established based on the testing of the products of conception after a second miscarriage (Figure 1). Using this algorithm, the karyotype on the second miscarriage determines the next step in the evaluation for RPL [15]. The further work-up of early RPL is continued in figure 2. The evaluation begins after 2 miscarriages with either no evaluation or euploid POC [15,16].
Figure 1: Algorithm for evaluation of recurrent pregnancy loss (RPL).
Figure 2: Work-up for early RPL.
Management of recurrent miscarriage
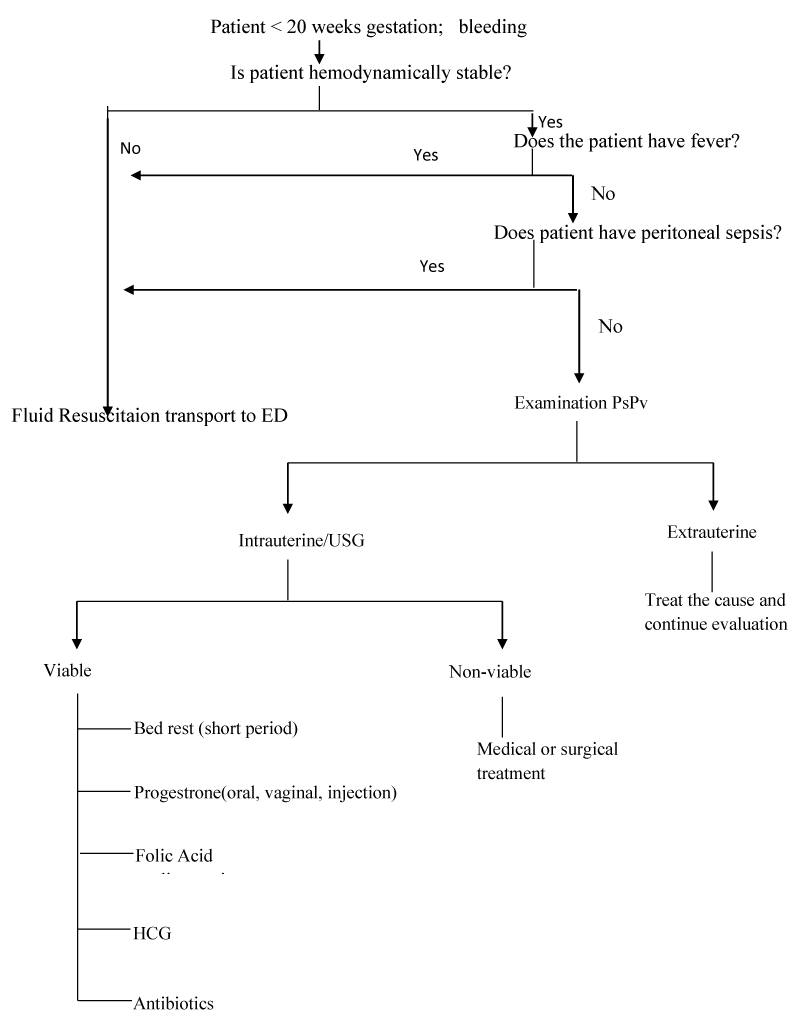
Patients with a threatened abortion should be managed expectantly until their symptoms resolve. Patients should be monitored for progression to an inevitable, incomplete, or complete abortion [15]. Figure 3 presents an algorithm for management of spontaneous abortion [13,17]. Doctors often prescribe bed rest and progesterone for women with symptoms of threatened miscarriage [18].
Figure 3: Algorithm for management of spontaneous abortion.
Bed rest
Bed rest is one of the most commonly-prescribed interventions for threatened miscarriages. Although there is no definite evidence that bed rest can affect the course of pregnancy, but one randomized controlled trial showed the impact of bed rest on the course of threatened miscarriage [18,19].
Pharmacological evaluation of supplemental progestin
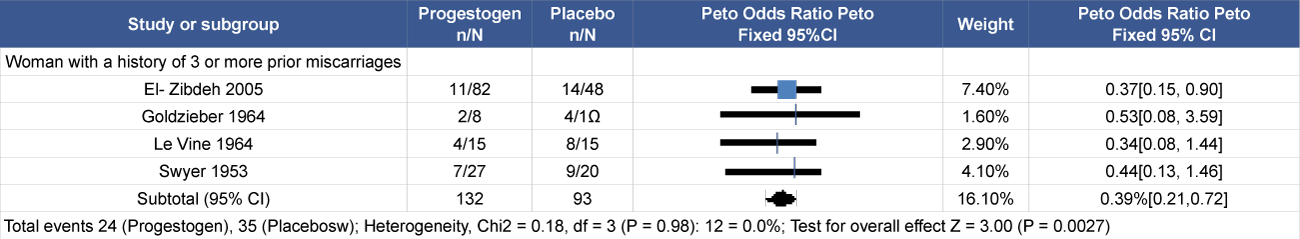
Progesterone sustains decidualization, controls uterine contractility and cervical competence, and functions as an ‘immunosteroid’ by promoting maternal immune tolerance to the fetal semi-allograft and controlling the bias towards a pregnancy protective immune milieu via a protein known as progesterone-induced blocking factor (PIBF) [20]. Exogenous progesterone supplementation can occur in various forms such as medroxyprogesterone acetate, 17-alpha-hydroxyprogesterone caproate, progesterone and dydrogesterone [13]. Evidence from studies show reduced miscarriage and better pregnancy chances Systematic review/meta-analysis (Table 3) [21].
Table 3: Algorithm for management of spontaneous abortion.
Aspirin and heparin
Anticoagulants, including aspirin and low molecular weight heparin (LMW heparin) or unfractionated heparin, have been used in the management of recurrent miscarriages in cases of antiphospholipid syndrome (APS). Both unfractionated heparin and LMW heparin do not cross the placenta and do not have teratogenic effects, or cause bleeding in the foetus [13].
Human chorionic gonadotrophin (hCG)
hCG is produced by the trophoblast in pregnancy and stimulates both the corpus luteum and the foetoplacental endocrine functions, resulting in progesterone production [4]. RCOG recommends the use of hCG supplementation in early pregnancy only in the context of randomized control trial (RCT)s [21].
Vitamins
Oxidative stress has been associated with spontaneous and recurrent miscarriages, antioxidants such as vitamins C and E could be beneficial in preventing miscarriages [13].
Antibiotics
Bacterial vaginosis (BV) is a condition in which the normal vaginal flora, mainly Lactobacillus, is replaced by an overgrowth of anaerobic bacteria (Mycoplasmahominis, Bacteroides spp., Mobiluncus spp.). It is well established that BV in pregnancy predisposes to both preterm labour and second trimester miscarriages, with an increased relative risk of 3.1–3.9 times in second trimester miscarriages among women who had BV. Treatment with antibiotics lowered the risk of preterm rupture of membranes and low birth weight even though the risk of preterm labor was not reduced [13].
Surgical management
Surgical management is indicated for patients with contraindications to medical treatment or failed medical treatment, and for patients who are hemodynamically unstable. Surgical treatment options include salpingectomy and salpingostomy is preferred for patients who wish to preserve fertility; however, it may result in inadequate evacuation of products of conception and a recurrence of symptoms. Laparoscopy is the preferred surgical approach [22].
Threatened miscarriage
A threatened miscarriage is defined as vaginal bleeding, usually painless, that occurs in the first 24 weeks in a viable pregnancy without cervical dilatation [13]. When bleeding is slight or resolves, pregnancy may continue normally but threatened miscarriage can be associated with a higher likelihood of adverse pregnancy outcome like prematurity (which is increased two fold), small-for-gestational-age babies (which is increased three fold), and perinatal death [23].
Incidence of threatened miscarriage
Threatened miscarriage is common, especially in the first trimester, occurring in 14% – 21% of all pregnancies [13]. The risk of miscarriage increases with increasing maternal age and, in some cases, with paternal age [24].
The incidence of early miscarriage significantly increased with advanced maternal age, from 10% - 15% in women aged 20 to 34 years to 51% in women aged 40 to 44 years [25]. A large majority of the pregnancies are lost before the missed period and, therefore, referred to as biochemical pregnancies. Miscarriage can be associated with considerable physical and psychological sequelae ranging from depression to intense grief [23].
Pathophysiology involved in threatened miscarriage
Currently the known cause of threatened miscarriage includes changes in levels of cytokines and placental membranes, maternal immune dysfunction, and endocrine abnormalities.
Abnormal cytokines profiles
The pathophysiology of threatened miscarriage in terms of cytokines involves a change in the T helper (Th) 1/Th2 balance resulting from an increase of uterine Th1 type proinflammatory cytokines and/or a deficiency of Th2/3 type cytokines, therein increased maternal serum interleukin (IL)-2 receptor and tumor necrosis factor (TNF)-α level. Changes in levels of these cytokines could help to predict theoutcome.
Immunological dysfunction
Immunologic recognition of pregnancy is crucial to the maintenance of gestation. And inadequate recognition of fetal antigens may cause abortion [26]. Presence of Anti-b2 -glycoprotein I antibodies is associated with an increased risk of pregnancy loss in women with threatened abortion in the first trimester [27]. Circulating levels of chemokines which are proteins involve in regulation of inflammation and immune response are associated with increased risk of threatened miscarriage and may have a regulatory function in pregnancy. Elevated epithelial cell-derived neutrophil-activating protein-78 (ENA-78) levels, a protein involved in regulation of angiogenesis and leukocyte recruitment, are associated with increased risk interval of miscarriage as the collection-outcome increased [28]. In case of RPL, One specific autoimmune disorder, APS, requires particular attention as it has been clearly linked with many poor obstetric outcomes, including RPL [16].
Oxidative stress
Lipid peroxidation and antioxidant enzyme activity variation may be of importance in the pathogenesis of miscarriage [12]. O2 free radicals are generated under hypoxic conditions and confirmed to be a potential teratogenic threat to the fetal tissues and are known to be related to the pathophysiology of common human pregnancy disorders, including miscarriage [26].
Endocrine disorders:
The most common endocrinologic factors are polycystic ovarian syndrome (PCOS) and obesity. In addition to fetal defects, these include anatomically polycystic ovaries, obesity, endometrial defects, placental thrombosis, and hormonal abnormalities such as insulin resistance or excess androgen secretion [28].
Investigation in threatened miscarriage
First-trimester bleeding in a pregnant woman has an extensive differential diagnosis (Table 4) and should be evaluated with a full history and physical examination [17,18]. A missed spontaneous abortion usually is diagnosed by routine Ultrasonography or when an ultrasound scan is obtained because the symptoms and physical signs of pregnancy are regressing [17].
| Table 4: Differential Diagnosis of First-Trimester Vaginal Bleeding. | |
| Favourable prognostic factors | Adverse prognostic factors |
| History | |
| Advancing gestational age | Maternal age >34 years |
| Spontaneous abortion | |
| Infection of the vagina or cervix | |
| Sonography | |
| Fetal heart activity at presentation | Fetal bradycardia |
| Discrepancy between gestational age and crown to rump length | |
| Maternal serum biochemistry | |
| Normal levels of these markers | Low β hCG values |
| Free β hCG value of 20 ng/ml | |
| β hCG increase <66% in 48 hrs | |
| Bioactive/immunoreactive ratio hCG < 0.5 | |
| Progesterone <45 nmol/l in 1st trimester | |
| Inhibin A <0.553 multiples of median | |
| CA125 level ≥43.1 U/mL in 1st trimester | |
History and physical examination
Vaginal bleeding in early pregnancy requires prompt attention. A review of the menstrual history and prior ultrasonography can help establish gestational dating and determine whether the pregnancy location is known. A speculum examination can help identify non obstetric causes of bleeding, such as vaginitis, cervicitis, or a cervical polyp. If products of conception are visible on speculum examination, the diagnosis of incomplete abortion can be made and treatment offered [22].
Pelvic examination
Pelvic exam is a mandatory to determine the type of abortion. During the pelvic exam, suction may be needed to remove blood and products of conception to allow for better visualization of the cervix [29].
Sonographic evaluation
Sonography can usually differentiate between an intrauterine pregnancy (viable or non-viable), a molar pregnancy, or an inevitable abortion [18].
Maternal serum markers
Women with threatened miscarriage generally show lower serum hCG values as compared with women continuing the pregnancy [18].
Management of threatened miscarriage
Bed rest
Bed rest is conventionally the most commonly used management technique for threatened miscarriage. Despite this, there is little evidence of its value. Physical activity is rarely associated with an increased risk of miscarriage, and indeed a lack of activity can lead to a number of other complications such as thromboembolic events, back pain, muscle atrophy and bone loss [30].
Pharmacological evolution of supplemental progestins
Progesterone
Progesterone is the main product of the corpus luteum, and giving progestogen is expected to support a potentially deficient corpus luteum gravidarum and induce relaxation of a cramping uterus. Progesterone is prescribed in 13% - 40% of women with threatened miscarriage, according to published series [18]. A Meta-analysis reviewed various clinical trial and showed the impact of progesterone supplementation on miscarriage rate [31].
Dydrogesterone: Dydrogesterone is highly selective for the progesterone receptor and differs from most other synthetic progestogens in its lack of oestrogenic, androgenic, anabolic and corticoid properties. It is considered particularly suitable for the management of women with threatened miscarriage and other pregnancy-related disorders as it does not suppress the pituitary–gonadal-axis at normal therapeutic doses. This means that it does not affect the normal secretory transformation of the endometrium, does not inhibit formation of progesterone in the placenta during early pregnancy and does not cause masculinisation of the female fetus [30].
Recent studies have focused on the use of dydrogesterone, an orally-active progestogen with no androgenic effects. There have been no reports of foetal abnormalities other. A small recent RCT on its use in the context of a threatened miscarriage showed that there was an improvement in outcome with more continuing pregnancies in the treatment group. The use of dydrogesterone in recurrent miscarriages has also been studied in another recent RCT, which showed a decrease in the number of miscarriages as compared to both the control group [13].
Uterine relaxing agents
Increased uterine activity is associated with threatened miscarriage and morphine was introduced in the 19th century in the belief that it would reduce contractions and prolong pregnancy. Morphine has now been replaced with antispasmodic drugs and myometrial relaxants (tocolytic agents) [13].
All patients with recurrent or threatened miscarriages should receive supportive care and close supervision. Appropriate investigations should be carried out to elicit any treatable cause for recurrent miscarriages. When a specific aetiological factor can be identified, directed treatment is warranted. There is early evidence that dydrogesterone reduces miscarriage rates. Consideration should be made for the screening of BV in all women between 10–22 weeks and treatment with oral or vaginal clindamycin, if the swab is positive.
We acknowledge the Abbott team for their assistance, guidance, and expertise in convening the expert forum. The information contained herein solely represents the views and opinions of the authors. This expert opinion document does not seek to represent the opinions and policies of or the procedures used by Abbott.
Funding
This expert opinion initiative was funded by Abbott. The article processing charges and the open access fee received by the journal for the publication of this article were sponsored by Abbott.
Medical writing and/or editorial assistance
Editorial support was provided by Spirant Communications Private Limited, which was funded by Abbott.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work, and gave final approval for the version to be published.
- RCOG Green Top Guideline. The investigation and treatment of couples with recurrent first-trimester and second-trimester miscarriage, RCOG Green Top Guideline. 2011; 17: 1-17.
- Radford EJ, Hughes M. Women's experiences of early miscarriage: implications for nursing care. J Clin Nurs. 2015; 24: 1457-1465. PubMed: https://pubmed.ncbi.nlm.nih.gov/25662397/
- Horne AW, Alexander CI. Recurrent miscarriage. J Fam Plann Reprod Health Care. 2005; 31: 103-107. PubMed: https://pubmed.ncbi.nlm.nih.gov/15921544/
- El Hachem H, Crepaux V, May-Panloup P, Descamps P, Legendre G, Bouet PE. Recurrent pregnancy loss: current perspectives. Int J Womens Health. 2017; 9: 331-345. PubMed: https://pubmed.ncbi.nlm.nih.gov/28553146/
- Homer HA. Modern management of recurrent miscarriage. Aust N Z J Obstet Gynaecol. 2019; 59: 36-44. PubMed: https://pubmed.ncbi.nlm.nih.gov/30393965/
- Patki A, Chauhan N. An epidemiology study to determine the prevalence and risk factors associated with recurrent spontaneous miscarriage in India. J Obstet Gynaecol India. 2016; 66: 310-315. PubMed: https://pubmed.ncbi.nlm.nih.gov/27486274/
- Garrido-Gimenez C, Alijotas-Reig J. Recurrent miscarriage: causes, evaluation and management. Postgrad Med J. 2015; 91: 151-162. PubMed: https://pubmed.ncbi.nlm.nih.gov/25681385/
- Lia J, Gaob JS, Wangc CC, Ngd EH, Wub XK. Evidence-based interventions of threatened miscarriage. World. 2017; 3: 50-59.
- Jaslow C, Carney J, Kutteh W. Diagnostic factors identified in 1020 women with two versus three or more recurrent pregnancy losses. Fertil Steril 2010; 93: 1234–1243. PubMed: https://pubmed.ncbi.nlm.nih.gov/19338986/
- French DA. A clinician’s approach to the diagnosis and management of recurrent pregnancy loss. Physician Assistant Clinics. 2018; 3: 457-468.
- Jefferys A, Vanderpump M, Yasmin E. Thyroid dysfunction and reproductive health. Obs Gynaecol. 2015; 17: 39–45.
- Brezina P, Kutteh W. Classic and cutting-edge strategies for the management of early pregnancy loss. Obstet Gynecol Clin North Am. 2014; 41: 1–18. PubMed: https://pubmed.ncbi.nlm.nih.gov/24491981/
- Tien JC, Tan TY. Non-surgical interventions for threatened and recurrent miscarriages. Singapore Med J. 2007; 48: 1074-1090. PubMed: https://pubmed.ncbi.nlm.nih.gov/18043834/
- Li YH, Marren A. Recurrent pregnancy loss. Aust J Gen Pract. 2018; 47: 432. PubMed: https://pubmed.ncbi.nlm.nih.gov/30114870/
- Kutteh WH. Novel strategies for the management of recurrent pregnancy loss. Semin Reprod Med. 2015; 33: 161-168. PubMed: https://pubmed.ncbi.nlm.nih.gov/26036897/
- Ford HB, Schust DJ. Recurrent pregnancy loss: etiology, diagnosis, and therapy. Reviews in obstetrics and gynecology. 2009; 2: 76-83. PubMed: https://pubmed.ncbi.nlm.nih.gov/19609401/
- Griebel CP, Halvorsen J, Golemon TB, Day AA. Management of spontaneous abortion. Am Fam Physician. 2005; 72: 1243-1250. PubMed: https://pubmed.ncbi.nlm.nih.gov/16225027/
- Sotiriadis A, Papatheodorou S, Makrydimas G. Threatened miscarriage: evaluation and management. BMJ. 2004; 329: 152-155. PubMed: https://pubmed.ncbi.nlm.nih.gov/15258071/
- Harrison RF. A comparative study of human chorionic gonadotropin, placebo, and bed rest for women with early threatened abortion. Int J Fertil Menopausal Stud. 1993; 38: 160-165. PubMed: https://pubmed.ncbi.nlm.nih.gov/8348164/
- Arck PC, Rücke M, Rose M, Szekeres-Bartho J, Douglas AJ, Pritsch M, et al. Early risk factors for miscarriage: a prospective cohort study in pregnant women. Reprod Biomed Online. 2008; 17: 101-113. PubMed: https://pubmed.ncbi.nlm.nih.gov/18616898/
- Brenner B, Bar J, Ellis M, Yarom I, Yohai D, Samueloff A et al. Effects of enoxaparin on late pregnancy complications and neonatal outcome in women with recurrent pregnancy loss and thrombophilia: results from the Live-Enox study. Fertil Steril. 2005; 84: 770-773. PubMed: https://pubmed.ncbi.nlm.nih.gov/16169422/
- Hendriks E, MacNaughton H, MacKenzie MC. First Trimester Bleeding: Evaluation and Management. Am Fam Physician. 2019; 99: 166-174. PubMed: https://pubmed.ncbi.nlm.nih.gov/30702252/
- Devaseelan P, Fogarty PP, Regan L. Human chorionic gonadotrophin for threatened miscarriage. Cochrane Database Syst Rev. 2010; 5: CD007422. PubMed: https://pubmed.ncbi.nlm.nih.gov/20464754/
- Coppola PT, Coppola M. Vaginal bleeding in the first 20 weeks of pregnancy. Emerg Med Clin North Am. 2003; 21: 667-677. PubMed: https://pubmed.ncbi.nlm.nih.gov/12962352/
- Nybo Andersen AM, Wohlfahrt J, Christens P, Olsen J, Melbye M. Maternal age and fetal loss: population based register linkage study. BMJ. 2000; 320: 1708-1712. PubMed: https://pubmed.ncbi.nlm.nih.gov/10864550/
- Brezina PR, Kutteh WH. Recurrent early pregnancy loss. In Clinical Reproductive Medicine and Surgery. 2013; 197-208.
- Mezzesimi A, Florio P, Reis FM, D'Aniello G, Sabatini L, et al. The detection of anti-beta2-glycoprotein I antibodies is associated with increased risk of pregnancy loss in women with threatened abortion in the first trimester. Eur J Obstet Gynecol Reprod Biol. 2007; 133: 164-168. PubMed: https://pubmed.ncbi.nlm.nih.gov/17046145/
- van der Spuy ZM, Dyer SJ. The pathogenesis of infertility and early pregnancy loss in polycystic ovary syndrome. Best Pract Res Clin Obstet Gynaecol. 2004; 18: 755–771. PubMed: https://pubmed.ncbi.nlm.nih.gov/15380145/
- Mouri M, Rupp TJ. Threatened Abortion. InStatPearls [Internet] 2019 May 6. StatPearls Publishing.
- Qureshi NS. Treatment options for threatened miscarriage. Maturitas. 2009; 65 Suppl 1: S35-41. PubMed: https://pubmed.ncbi.nlm.nih.gov/19945236/
- Oates-Whitehead RM, Haas DM, Carrier JAK. Progestogen for preventing miscarriage. In: Cochrane Library. Chichester: Wiley, 2003. CD003511. PubMed: https://pubmed.ncbi.nlm.nih.gov/14583982/