More Information
Submitted: 13 October 2020 | Approved: 03 November 2020 | Published: 04 November 2020
How to cite this article: De Miguel Manso S, García García E, Gobernado Tejedor JA, Badillo Bercebal CE, Viruega Cuaresma D, et al. 4-year recurrence risk factors after tension-free vaginal tape-obturator as a treatment of stress urinary incontinence. Clin J Obstet Gynecol. 2020; 3: 145-150.
DOI: 10.29328/journal.cjog.1001069
ORCiD: orcid.org/0000-0003-0753-9802
Copyright License: © 2020 De Miguel Manso S, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Recurrence; Risk factors; Stress urinary incontinence
Abbreviations: BMI: Body Mass Index; MUI: Mixed Urinary Incontinence; OR: Odds Ratio; POP: Pelvic Organ Prolapse; ROC: Receiver Operating Characteristic; SUI: Stress Urinary Incontinence; TO: Transobturator Bands; TVT: Retropubic Bands; UDS: Urodynamic Study
4-year recurrence risk factors after tension-free vaginal tape-obturator as a treatment of stress urinary incontinence
De Miguel Manso S1,2*, García García E1, Gobernado Tejedor JA1, Badillo Bercebal CE1, Viruega Cuaresma D1 and González Martín JI1
1Department of Obstetrics and Gynecology, Valladolid University Clinical Hospital, Spain
2Faculty of Medicine, University of Valladolid, Spain
*Address for Correspondence: S De Miguel Manso, Department of Obstetrics and Gynecology ,Faculty of Medicine, Valladolid University Clinical Hospital, Spain, Tel: +34617061826; Email: [email protected]
Objectives: Tension-free vaginal tapes are the gold standard of the surgical treatment of stress urinary incontinence (SUI); however, long-term recurrence of SUI after this surgery has been a matter of problem. Here, we attempted to determine the incidence of its recurrence and to identify the risk factors of 4-year-recurrence of SUI after this surgery.
Methods: Of all patients undergoing this surgery (n = 341, 2015-2019), 71 patients were met the study inclusion criteria. Of 71, SUI recurred in 8 patients, with the recurrence rate being 11.3%. The following three were identified to be independent risk factors: older age, history of delivery of macrosomic baby (>4 kg), and the presence of mixed urinary incontinence. The frequency of recurrence in cases with mixed incontinence amounted for 19.5%. Recurrence was 22 and 50% for women with macrosomic delivery once and more than twice, respectively.
Conclusion: Advanced age, macrosomic delivery and mixed urinary incontinence have shown to be independent risk factors of recurrence of SUI after tension-free vaginal tape-obturator at 4 years.
Key message: Stress urinary incontinence can recur so investigate possible risk factors is a priority. Our paper relates recurrence with: advanced age, fetal macrosomia and mixed incontinence.
Stress urinary incontinence (SUI) is defined, according to the ICS (International Continence Society) terminology standardization, as involuntary loss of urine after physical exertion (sport, activity) or after coughing or sneezing [1]. It is estimated that its prevalence in the female population ranges between 10% and 40% [2].
Treatment of SUI depends on the degree of severity. Therapy generally begins by changing lifestyle and the rehabilitation of the pelvic floor musculature for at least 3 months. In moderate and severe cases, when these measures have failed, surgical treatment will be indicated, which will depend on the degree and conditions of the patient (suburethral band or bulking agents if there are comorbidities that make surgery impossible) [2].
Rehabilitation of the pelvic floor muscles is effective for the treatment of mild-moderate SUI in the short-medium term and is more effective than the absence of treatment. Therefore, a significant number of women will seek other treatment alternatives with a faster cure [3].
Synthetic suburethral polypropylene tapes are the “gold standard” for the surgical treatment of SUI according to the guidelines of the European Society of Urology (ESU, 2016) [4] and the position of the European Urogynecological Association (USA, 2017) [5].
Current tension-free vaginal tapes include the retropubic and transobturator pathways.
The largest long-term randomized controlled study (9 years, n = 341) performed with TO (both modalities: in-out and out-in) reveals a stable success rate with transobturator tape after 3 years. The subjective cure at 1, 3 and 9 years was 80%, 73.1% and 71.6% respectively. The reduction in the cure rate was significant between the first and ninth year, but not between the first and third year [6].
The surgical treatment of SUI with a tension-free vaginal tape is currently performed using the TO pathway, which has shown high cure rates, especially in the short and medium-term, since the long-term studies report highly variable rates, between 43% and 92% [7] (Cochrane, 2017).
The decrease in cure rate in the medium and long term means that SUI recurs, and many are the variables that have been studied and that may influence.
The objective of this study is to identify factors associated with the risk of recurrence of SUI after 4 years.
A prospective four-year follow-up observational study (2015-2019) was performed in women suffering from stress urinary incontinence who underwent treatment using the tension-free vaginal tape-obturator.
All the patients underwent treatment in the University Clinic Hospital of Valladolid (Spain) and were evaluated at the Pelvic Floor Unit. The main output variable studied was recurrence of stress urinary incontinence (positive cough test with a frequency of at least several times per week) and the follow-up was carried-out after 6 months, 1, 2, 3 and 4 years: over the first 2 years it was performed in person at the consultation and for the 3rd and the 4th year patients were evaluated by telephone interview. As secondary results, we value possible variables associated with the risk of recurrence and differences in complications between patients with and without recurrence.
Objective cure was evaluated using the cough test in consultation (with a bladder filled with 250-300 ml and checked by ultrasound) and by telephone through an exhaustive anamnesis of SUI symptoms. Subjective cure was evaluated with the PGI (Patient Global Impression of Improvement) scale.
The only exclusion criteria for the insertion of a TO band were being under 18 years old and suffering from SUI due to intrinsic sphincter deficiency evaluated by urodynamic study (UDS).
No patient had to be excluded because of these reasons. Therefore, women without taking into account the following criteria were included: body mass index (BMI), previous anti-incontinence surgery, associated pelvic organ prolapse surgery (POP) and symptoms of overactive bladder with or without incontinence.
Anthropometric variables (age, height, weight and BMI), obstetric history (parity, vaginal delivery of fetus >4 kg, delivery with forceps), comorbidity (AH, respiratory, neurological or psychiatric pathology), concomitant medication (antihypertensive, respiratory, neurological or psychiatric), previous anti-incontinence surgery, type of urinary incontinence (effort, mixed), severity of SUI (Grade I, II, III), type of TO tape (in-out, out-in ), correction of associated POP and type of surgery were studied.
The UDS was only performed in recurrent SUI, when SUI was suspected to be due to intrinsic sphincter deficiency and in complex urine incontinence (UI).
Post-surgical complications were recorded and classified by time periods: immediate (<7 days), intermediate (7-30 days), and late (>1 month).
Patients with mixed urinary incontinence (MUI) and/or treatment with anticholinergics, with previous surgeries of SUI and who underwent concomitant POP surgery were also included.
The surgery was performed by 4 gynecologists and the insertion modality, in-out or out-in, depended on the surgeon’s preference.
The types of in-out TO tape used were: I-Stop Braun® (B. Braun SA, Barcelona) and TOA® (Presurgy SL adjustable sling, Madrid), and with the out-in needle path Monarc® bands were placed until 2015 (AMS, Inc., Minnetonka, USA).
Estatistical analyses
The Kolmogorov-Smirnov test was applied for quantitative variables to determine the type of distribution. The T-Student test was used to study quantitative variables with a normal distribution, and the U-Mann-Witney test was used otherwise. The Chi-square test with Yates correction was used to study qualitative variables. In all cases, less than 0.05 was the value taken as statistically significant. For quantitative variables with a statistically significant relationship, a ROC curve was constructed and the area under the curve was calculated, and for qualitative variables the OR was calculated with a 95% confidence interval. SSPS v. 23 was the stadistic software used.
Ethical approval
The patients were verbally informed individually, both in consultation and by telephone, that their data will be included in studies on the results of the anti-incontinence bands, if they were satisfied with it. For this purpose, this study was authorized by the ethics and research committee of the eastern health area of Valladolid. With start date of the study 02-13-2015 and approval date 03-18-2016 (Code: FO-P07-12) (Appendice-1).
Informed written consent was obtained from the patients to undergo the surgical intervention, and regarding the degree of satisfaction during the follow-up, the consent was verbal informing them that the data would be treated respectfully and confidentially with the intention of studying the long-term results of the bands.
The sample was composed of 71 women operated on with tension-free vaginal tape-obturator and followed during 4 years: 8 women of this sample showed symptomatic relapse of SUI, representing 11.27% of recurrence. There were no significant differences regarding the type of TO tape placed, either the insertion of the needle from inside to outside or from outside to inside (Table 1).
| Table 1: Type of transobturator tape. | |||
| Type of to tape | Recurrence | p | |
| No (63) | Yes (8) | ||
| Out-in: Monarc® | 8 | 2 | 0.117a |
| In-out: I-stop® Toa® |
47 8 |
6 0 |
|
| achi-square | |||
From all variables analyzed those that showed a significant association with the recurrence of SUI in the univariate analysis were age, a history of fetal macrosomia and suffering from MUI. The most relevant factors studied are shown in table 2.
| Table 2: Univariate association between anthropometric, obstetric, medical variables, type and grade of urinary incontinence, previous surgery for SUI, simultaneous surgery for POP, previous urodinamic study and complications, and the development of relapse of SUI. | |||
| Variable | Recurrence | p | |
| No | Yes | ||
| AGE (70) Median (Range Q1-Q3) |
(62) 67.00 (41-80) |
(8) 75.00 (64-85) |
< 0.008a |
| Weight (kg) (68) Mean ± Standard Deviation |
(61) 69.79 ± 11.722 |
(7) 65.57 ± 11.731 |
0.370b |
| Daily physical activity (14) | 14 | 0 | 0.137c |
| Parity (≥ 1) (66) | 58 | 8 | 0.099a |
| Forceps (≥ 1) (4) | 4 | 0 | 0.635c |
| Fetal macrosomy (13) 1 delivery >4 kg ≥2 deliveries >4 kg |
7 2 |
2 2 |
0.01c |
| AH (35) | 30 | 5 | 0.428c |
| Respiratory pathology (4) | 3 | 1 | 0.371c |
| Psychiatric pathology (15) | 13 | 2 | 0.776c |
| Tobacco ≥ 5 per day (5) | 5 | 0 | p = 0.409c |
| Previous mui (41) | 33 | 8 | p = 0.010c |
| SUI grade: I (2) II (58) III (11) |
2 51 10 |
0 7 1 |
0.842c |
| Previous SUI surgery (10) | 10 | 0 | > 0.05c |
| Associated pop surgery (49) | 42 | 7 | p = 0.230c |
| Uds prior to surgery (11) | 10 | 1 | p = 0.804c |
| Immediate complications (10) | 8 | 2 | p < 0.05c |
| Intermediate complications (3) | 3 | 0 | p < 0.05c |
| Late complications (11) | 4 | 7 | p < 0.05c |
| Aumw; bt-Student; cchi-square | |||
From the entire sample, 10 patients had a history of anti-incontinence surgery: 6 of them had already another transobturator tape put down and 4 of them had another mini-sling tape put down. These 10 patients were also evaluated with UDS to rule out intrinsic sphincter deficit before vaginal tape-obturator tension-free. Another patient required a UDS for complex urinary symptoms, ruling out sphincter deficiency.
49 women of the sample also underwent a POP surgery in the same procedure. Neither of these 2 variables were related to the risk of recurrence (Table 2).
There were also no differences in the degree of SUI and the frequency of complications between patients with and without recurrence of SUI (Table 2).
In this sample of patients, the immediate complications were (n = 10): fever, pain, bladder retention and urgent surgery for bleeding; as intermediate complications appeared (n = 3): urinary tract infection (UTI) and bladder retention, and after more than 1 month the complications were (n = 11): de novo urgency, bladder retention, pain and urethrolysis (Table 2).
The variables that showed a significant association with SUI recurrence in the bivariate analysis were: age, mixed urinary incontinence and fetal macrosomia.
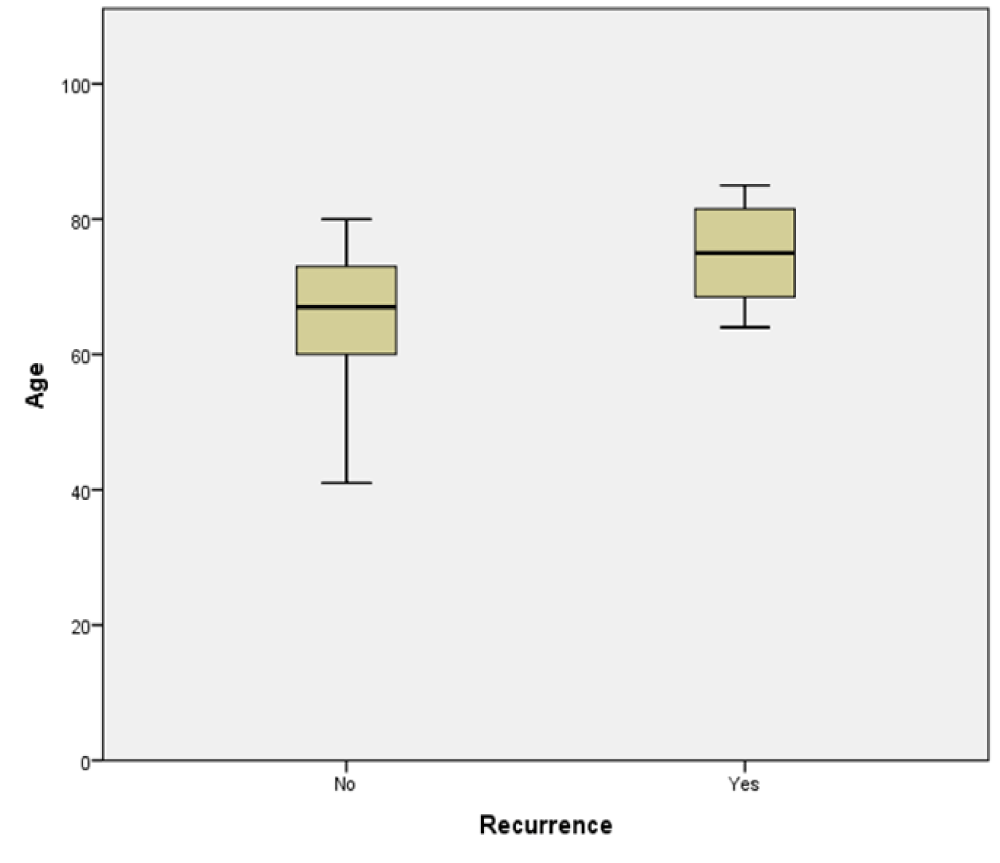
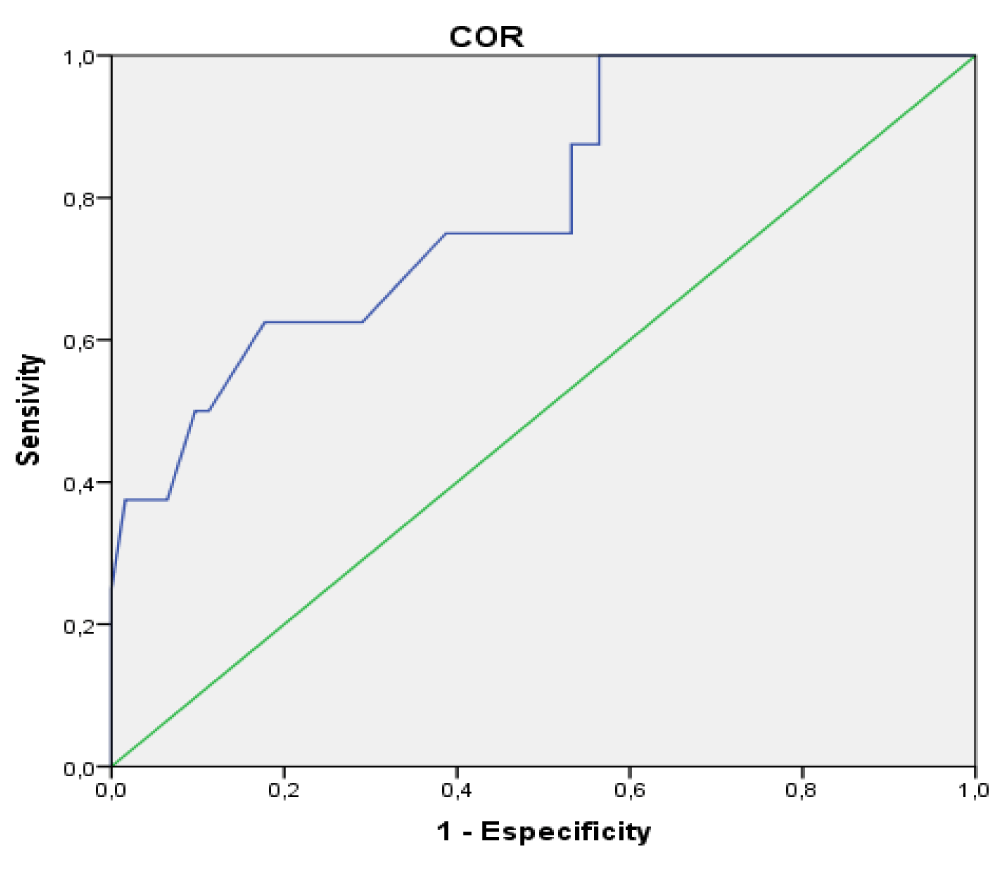
As can be seen in the figure 1, patients who presented SUI recurrence were older at the time of surgery (median of 75 years) than those not presenting it (median of 67 years). In addition, age as a predictor of recurrence has an area under the curve ROC of 0.79 (Figure 2).
Figure 1: Age distribution in both groups.
Figure 2: ROC curve for the age-relapse of SUI relationship.
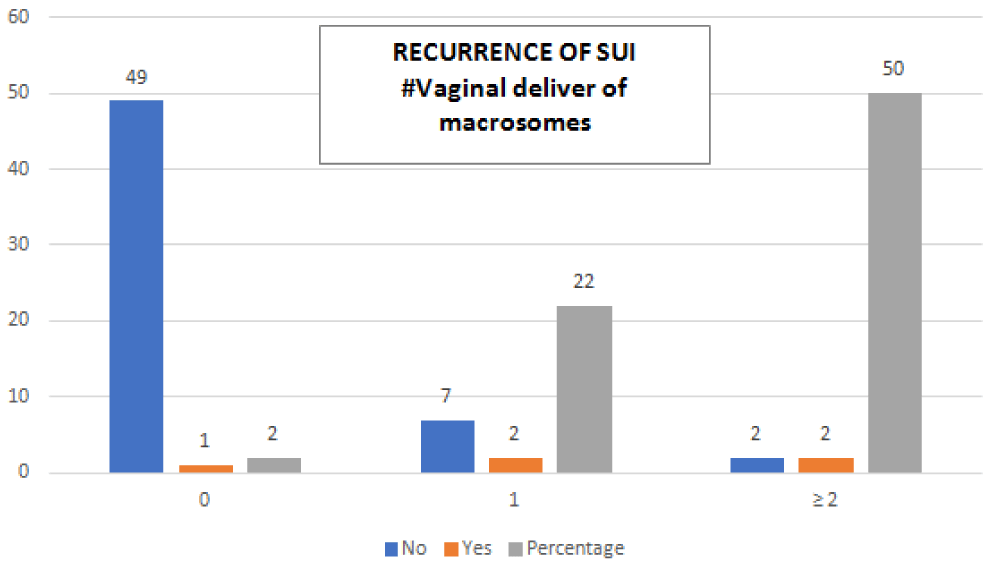
22% of the patients with a history of fetal macrosomia who underwent surgery with a tension-free vaginal tape-obturator, presented recurrence of SUI after 4 years and this percentage increased to 50% when they had 2 or more deliveries with fetus > 4 kg (Figure 3).
Figure 3: SUI recurrence if antecedent of delivery >4 kg (1 delivery / ≥2 deliveries).
The history of fetal macrosomia obtained an OR of 21.78 (95% CI: 2.18-218.03) for recurrence of SUI. 19.5% of the women with MUI who underwent anti-incontinence surgery suffered a recurrence of SUI at the 4th year (Image 4), while patients with pure stress incontinence did not present it.
The probability of recurrence before surgery if having a MUI was 11.3%, with S=100%, E=47.6% and FP ratio=52.4%.
Bottom line: The frequency of recurrence of SUI at 4 years was 11.27%, but some factors increased this frequency, such as a history of fetal macrosomia (1 delivery >4 kg: 22% and ≥2 deliveries >4 kg: 50%) and suffering MUI (19.5%).
Multiple variables have been evaluated and proposed as possible risk factors for the development of recurrence of SUI after tension-free vaginal tape: advanced age, comorbidities, associated POP or concomitant POP surgery, a high BMI, presence of urgency or urge incontinence, previous urinary incontinence surgery, anticholinergic treatment or severity of incontinence.
Nevertheless, the advance in the knowledge of SUI recurrence after transobturator suburethral tape is complex for several reasons. The first is the heterogeneity of the available studies, from a methodological point of view and by the type of population included and the duration of follow-up. Most of the studies are retrospective and prospective, observational and cohort. Randomized controlled trials [8-10] are rare. Furthermore, the follow-up years range from 1 year [8,11,12], 4-5 years [9,10,13-16], to 7-10 years [17-20].
Our study is prospective observational, with a 4-year follow-up, and includes women with a prior MUI, a history of an anti-incontinence tape and POP surgery concomitant to the insertion of the tension-free vaginal tape. Therefore, it resembles the usual population, where all possible characteristics are given. Other studies have also included in their samples POP surgery [8,18], presenting an overactive bladder [13,15,19] and having previously SUI surgery [11].
There are authors who have carried out their studies with some exclusion criteria, which we have included such as associated POP surgery [13,20], overactive bladder [8,20] and prior anti-incontinence tape [8].
The frequency of recurrence of SUI at the 4th year in our study was 11.27%. This is similar to that found by other authors. Ashok, after a systematic review, describes it as 10% - 20% [21], Yonsson Funk estimates it at 13% at 9 years [17] and Serati at 9.2% at 5 years [14]. Nevertheless, higher percentages have been reported: 16.5% at 1 year [8], 18% at 5 years [13] and up to 30.12% at 4 years [16].
In our population, the risk of recurrence of SUI at 4 years was related to age, presenting MUI and a history of macrosomal delivery.
Thus, the frequency of recurrence if the type of incontinence was mixed amounted to 19.5%, if the patient had 1 delivery >4 kg to 22% and if the antecedent was ≥2 macrosomal deliveries it increased up to 50%.
In our sample, women who had recurrence were older than those who did not relapse (median of 75 vs. 67 years). Other authors also agree with this association [8,17]. However, other studies do not find this relationship [10,16].
As women get older, they lose the striated musculature of the bladder neck and dorsal wall of the urethra [22], which could modify the location of the suburethral sling and decrease its long-term efficacy.
A randomized two-arm trial (transobturator tape, in-out vs out-in) with 1-year follow-up, showed that for every 10 years that age increased, the risk of objective failure increased almost 50% compared to subjective [12]. Objective measures are more related to the mechanism of action of the suburethral band, and this mechanism can be affected by varying the characteristics of adjacent tissues with advancing age. In contrast, subjective failures may be influenced by symptoms of urgency.
In the case of patients with MUI, we found a probability of recurrence before surgery of 11.3%. No patient with pure SUI recurred during these 4 years. Women with symptoms of urge incontinence may reflect more complex neuromuscular dysfunction, so perhaps in these patients, more intense treatment with lifestyle changes and/or medical therapies should be considered before surgery [12].
A randomized study assigning 4-year retropubic or transobturator tape also related recurrence with MUI, with an OR of 2.4 [10]. A similar association with the MUI (OR = 2.87) was found by Paick in a prospective cohort study (retropubic vs. transobturator) but in the short term (mean follow-up of 10 months) [23].
The third significant association of our work was the history of macrosomal delivery, which obtained an OR of 21.78 (95% CI:2.18-218.03) for recurrence of SUI. This relationship has not been described in the literature and could suggest that women with births of more than 4 kg suffer greater involvement of the pelvic support structures, which in the long term would modify the positioning or function of the sling.
Several factors associated with recurrence described by other authors, such as prior anti-incontinence surgery [10,11,17], associated POP surgery [8,24] or BMI [10], have not been related to the risk of recurrence in our sample.
Advanced age, a history of macrosomic delivery and presenting MUI have shown a significant association with the risk of relapse of SUI after tension-free vaginal tape-obturator at 4 years.
This does not mean that these patients cannot benefit from the surgical treatment of the loss of urine with the effort, but that in the preoperative interview it would be necessary to inform them of a greater risk of failure in the medium term.
- Haylen BT, de Ridder D, Freeman RM, et al. International Urogynecological Association; International Continence Society. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol Urodyn. 2010; 29: 5-26. PubMed: https://pubmed.ncbi.nlm.nih.gov/19937315/
- Capobianco G, Madonia M, Morelli S, Dessole F, De Vita D, et al. Management of female stress urinary incontinence: A care pathway and update. Maturitas. 2018; 109: 32-38. PubMed: https://pubmed.ncbi.nlm.nih.gov/29452779/
- Labrie J, Berghmans BL, Fischer K, Milani AL, van der Wijk I, et al. Surgery versus physiotherapy for stress urinary incontinence. Engl J Med. 2013; 369: 1124-1133. PubMed: https://pubmed.ncbi.nlm.nih.gov/24047061/
- European Association of Urology. EAU guidelines on urinary incontinence in adults. 2016 In: https://uroweb.org/wp-content/uploads/EAU-Guidelines-Urinary-Incontinence-2016.pdf
- Chapple CR, Cruz F, Deffieux X, Milani AL, Arlandis S, et al. Consensus Statement of the European Urology Association and the European Urogynaecological Association on the Use of Implanted Materials for Treating Pelvic Organ Prolapse and Stress Urinary Incontinence. Eur Urol. 2017; 72: 424-431. PubMed: https://pubmed.ncbi.nlm.nih.gov/28413126/
- Karmakar D, Mostafa A, Abdel-Fattah M. Long-term Outcomes of Transobturator Tapes in Women With Stress Urinary Incontinence: E-TOT Randomised Controlled Trial. BJOG. 2017; 124: 973-981. PubMed: https://pubmed.ncbi.nlm.nih.gov/28094468/
- Ford AA, Rogerson L, Cody JD, Aluko P, Ogah JA. Mid-urethral sling operations for stress urinary incontinence in women. Cochrane Database Syst Rev. 2017; 7: CD006375. PubMed: https://pubmed.ncbi.nlm.nih.gov/26130017/
- Barber MD, Kleeman S, Karram MM, et al. Risk factors associated with failure 1 year after retropubic or transobturator midurethral slings. Am J Obstet Gynecol. 2008; 199: 666.e1-7. PubMed: https://pubmed.ncbi.nlm.nih.gov/19084098/
- Angioli R, Plotti F, Muzii L, Montera R, Panici PB, et al. Tension-free Vaginal Tape Versus Transobturator Suburethral Tape: Five-Year Follow-Up Results of a Prospective, Randomised Trial. Eur Urol. 2010; 58: 671-677. PubMed: https://pubmed.ncbi.nlm.nih.gov/20709444/
- Stav K, Dwyer PL, Rosamilia A, Schierlitz L, Lim YN, et al. Risk Factors of Treatment Failure of Midurethral Sling Procedures for Women With Urinary Stress Incontinence. Int Urogynecol J. 2010; 21: 149-155. PubMed: https://pubmed.ncbi.nlm.nih.gov/19855914/
- Abdel-Fattah M, Ramsay I, Pringle S, et al. Evaluation of transobturator tension-free vaginal tapes in management of women with recurrent stress urinary incontinence. Urology. 2011; 77: 1070-1075. PubMed: https://pubmed.ncbi.nlm.nih.gov/21414653/
- Richter HE, Litman HJ, Lukacz ES, Sirls LT, Rickey L, et al. Urinary Incontinence Treatment Network. Demographic and clinical predictors of treatment failure one year after midurethral sling surgery. Obstet Gynecol. 2011; 117: 913-921. PubMed: https://pubmed.ncbi.nlm.nih.gov/21422865/
- Groutz A, Rosen G, Gold R, Lessing JB, Gordon D. Long-term outcome of transobturator tension-free vaginal tape: efficacy and risk factors for surgical failure. J Womens Health. 2011; 20: 1525-1528. Https://pubmed.ncbi.nlm.nih.gov/21819253/
- Serati M, Bauer R, Cornu JN, et al. TVT-O for the treatment of pure urodynamic stress incontinence: efficacy, adverse effects, and prognostic factors at 5-year follow-up. Eur Urol. 2013; 63: 872-878. PubMed: https://pubmed.ncbi.nlm.nih.gov/23274106/
- Yonguc T, Gunlusoy B, Degirmenci T, et al. Are the outcomes of transobturator tape procedure for female stress urinary incontinence durable in long-term follow-up? Int Urol Nephrol. 2014; 46: 1295-1300. PubMed: https://pubmed.ncbi.nlm.nih.gov/24384878/
- Betari R, Meynier J, Forzini T, François T, Hakami F, et al. Is Initial Success After Monarc(®) Suburethral Sling Durable at Mid-Term Evaluation? Prog Urol. 2016; 26: 409-414. PubMed: https://pubmed.ncbi.nlm.nih.gov/27032312/
- Jonsson Funk M, Siddiqui NY, Kawasaki A, Wu JM. Long-term Outcomes After Stress Urinary Incontinence Surgery. Obstet Gynecol. 2012; 120: 83-90. Https://pubmed.ncbi.nlm.nih.gov/22914395/
- Athanasiou S, Grigoriadis T, Zacharakis D, Skampardonis N, Lourantou D, et al. Seven Years of Objective and Subjective Outcomes of Transobturator (TVT-O) Vaginal Tape: Why Do Tapes Fail? Int Urogynecol J. 2014; 25: 219-225. PubMed: https://pubmed.ncbi.nlm.nih.gov/23892532/
- Costantini E, Kocjancic E, Lazzeri M, et al. Long-term Efficacy of the Trans-Obturator and Retropubic Mid-Urethral Slings for Stress Urinary Incontinence: Update From a Randomized Clinical Trial. World J Urol. 2016; 34: 585-593 PubMed:. Https://pubmed.ncbi.nlm.nih.gov/26231286/
- Serati M, Braga A, Athanasiou S, et al. Tension-free Vaginal Tape-Obturator for Treatment of Pure Urodynamic Stress Urinary Incontinence: Efficacy and Adverse Effects at 10-year Follow-up. Eur Urol. 2017; 71: 674-679. PubMed: https://pubmed.ncbi.nlm.nih.gov/27597239/
- Ashok K, Wang A. Recurrent Urinary Stress Incontinence: An Overview. J Obstet Gynaecol Res. 2010; 36: 467-473. PubMed: https://pubmed.ncbi.nlm.nih.gov/20598022/
- Perucchini D, delancey JOL, Ashton-Miller JA, Galecki A, Schaer GN. Age effects on urethral striated muscle. II. Anatomic location of muscle loss. Am J Obstet Gynecol. 2002; 186: 356-360. PubMed: https://pubmed.ncbi.nlm.nih.gov/11904591/
- Paick JS, Cho MC, Oh SJ, Kim SW, Ku JH. Factors influencing the outcome of mid urethral sling procedures for female urinary incontinence. J Urol. 2007; 178: 985-989. PubMed: https://pubmed.ncbi.nlm.nih.gov/17632151/
- Black NA, Downs SH. The effectiveness of surgery for stress incontinence in women: a systematic review. Br J Urol. 1996; 78: 497-510. PubMed: https://pubmed.ncbi.nlm.nih.gov/8944504/