More Information
Submitted: 29 August 2020 | Approved: 07 September 2020 | Published: 08 September 2020
How to cite this article: Dionysopoulou A, Skala C, Weiss C, Hasenburg A, Albrich S. Establishment of a new reference line for 2D transperineal ultrasound in urogynecology. Clin J Obstet Gynecol. 2020; 3: 114-119.
DOI: 10.29328/journal.cjog.1001061
ORCiD: orcid.org/0000-0003-4601-6887
Copyright License: © 2020 Dionysopoulou A, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Transperineal ultrasound; Bladder neck descent; Urogynecology
Establishment of a new reference line for 2D transperineal ultrasound in urogynecology
Anna Dionysopoulou1*, Christine Skala1, Christel Weiss2, Annette Hasenburg1 and Stefan Albrich3
1Department of Obstetrics and Gynecology, University Medical Center Mainz, Johannes Gutenberg University, Langenbeckstr. 1, 55131 Mainz, Germany
2Department of Statistics and Biomathematics, Mannheim University Medical Centre, University of Heidelberg, Theodor Kutzer Ufer 1-3, 68167 Mannheim, Germany
3Frauenärzte 5 Höfe, Salvatorstr. 3, 80333 Munich, Germany
*Address for Correspondence: Anna Dionysopoulou, Department of Obstetrics and Gynecology, University Medical Center Mainz, Johannes Gutenberg University, Langenbeckstrasse 1. 55131 Mainz, Germany, Tel: +49 6131177311; Email: [email protected]
Background: The purpose of this study was to establish a new, reliable and reproducible reference line for assessing bladder neck descent using 2-dimensional transperineal ultrasound. Therefore, we created a novel line, named Symphysis-Levator Line (SLL) and defined it as the connecting line between the hyperechogenic, dorsocaudal edge of the symphysis pubis and the hyperechogenic anterior margin of the puborectalis muscle, posterior to the anorectal junction.
Methods: A retrospective study was performed including 111 patients, who underwent a transperineal ultrasound as part of an urogynecological examination in the department of Urogynecology at the University Medical Center of the Johannes Gutenberg University Mainz. We calculated the bladder neck decent using the SLL and compared our results with the measurements assessed using a horizontal line through the infero-posterior margin of the symphysis pubis, as previously described by Dietz (Horizontal Symphysis Line, HSL). In addition, we calculated the intra- and interobserver reliability of the two methods and examined the influence of various patient characteristics on the obtained values.
Results: Both methods demonstrated a high intra- and interobserver reliability. Even though the HSL produced slightly higher numerical values for the bladder neck descent, the novel SLL was more precise. Our data support that the 2-point fixation of the SLL on two anatomical structures ensures the stability of the reference plane during the functional changes of the pelvic floor.
Conclusion: The Symphysis-Levator Line could be a useful tool for urogynecologists in the future.
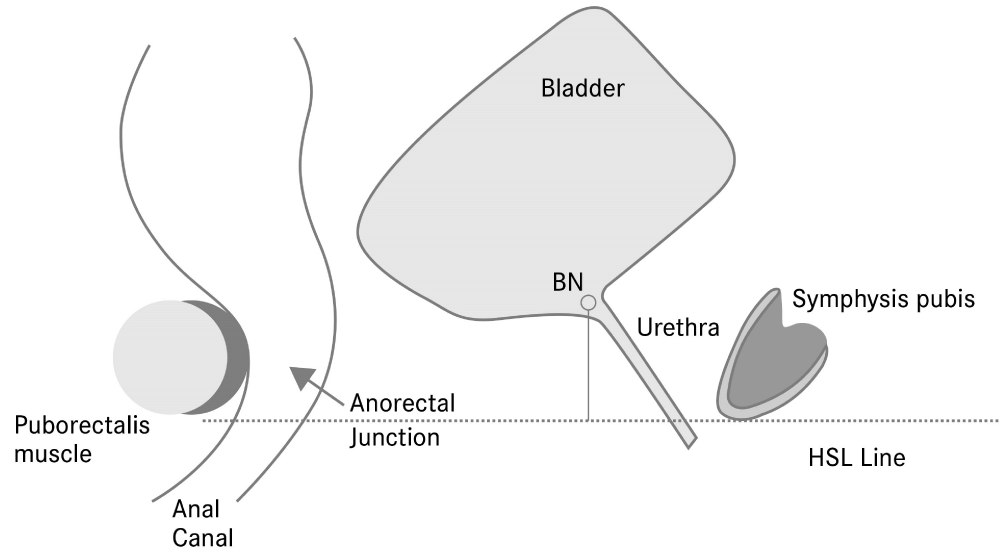
Pelvic floor disorders affect a large proportion of the female population and cause significant discomfort and impairment of both social function and quality of life. A thorough and accurate diagnostic work-up is essential not only in planning the therapeutic algorithm, but also postoperatively, when dealing with complications. In order to quantify the mobility of the internal urethral orifice, various examination techniques and coordinate systems, such as endorectal, endovaginal and transperineal ultrasound, the Q-tip test and lateral chain urethrocystography, have been proposed [1]. Among them, transperineal ultrasound imaging has proven to be most useful [2]. In order to determine the position of the bladder neck, the most commonly used method is relative to a horizontal line through the infero-posterior margin of the symphysis pubis, as previously described by Dietz (Horizontal Symphysis Line - HSL) (Figure 1) [3]. Another standardised and reproducible method is the central line of the symphysis, proposed by Schaer. The author used a rectangular coordination system conducted by drawing a line between the inferior and posterior border of the symphysis pubis [4]. A limitation of the methods used so far, is that only one anatomical structure, the symphysis pubis, is needed to draw the reference lines. As a consequence, the stability of the reference plane during the functional changes of the pelvic floor and movement of the patient is not guaranteed. In addition, lack of standardisation concerning the design of the studies and the examination technique, makes comparison of the findings difficult.
Figure 1: Illustration of the horizontal line through the infero-posterior border of the symphysis pubis, HSL:Horizontal-Symphysis Line BN: bladder neck.
The primary purpose of this study was to establish a new, reliable and reproducible reference line for assessing bladder neck descent using 2-dimensional transperineal ultrasound. We compared our measurements with the ones assessed using the HSL and determined the intraobserver and interobserver reliability of the two methods. In addition, we investigated the influence of various factors and patient characteristics, including patients´ age, body mass index, mode of delivery, parity, type of pelvic floor dysfunction (symptoms of stress urinary incontinence, overactive bladder syndrome, and pelvic organ prolapse) and the presence of a levator ani avulsion injury on the measurements obtained with each method respectively.
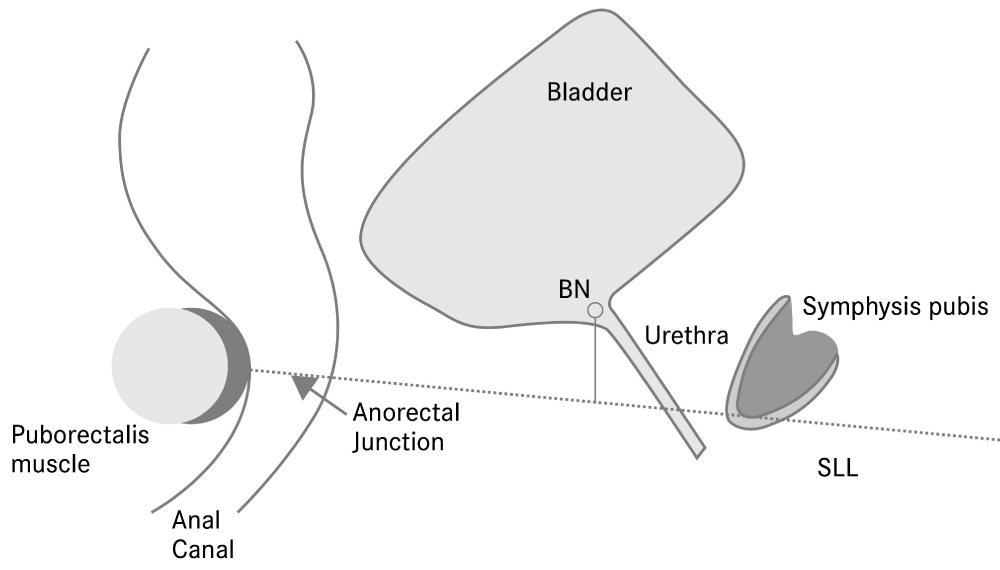
The new line: Symphysis-Levator Line (SLL)
In order to develop a reliable new coordinate system, we defined a reference line through not only one, but two separate anatomical reference points. We named the new line Symphysis-Levator Line, and defined it as the connecting line between the hyperechogenic, dorsocaudal edge of the symphysis pubis and the hyperechogenic anterior margin of the puborectalis muscle, posterior to the anorectal junction (Figure 2). The 2-point fixation of the SLL ensures the stability of the reference plane during Valsalva manoeuvre and contraction of the pelvic floor.
Figure 2: Illustration of the Symphysis-Levator Line (SLL), BN: bladder neck.
Patient population and procedure
This is a retrospective analysis of data collected from the files of 111 women, who were referred to the Department of Urogynecology at the University Medical Center of the Johannes Gutenberg University Mainz between January 2013 and July 2013. A thorough medical history using a standardized, self-made questionnaire was obtained. In addition to the demographic characteristics, special attention was paid to the obstetric history of the patients and in particular to the number of pregnancies and the mode of delivery. Lower urinary tract symptoms, such as urgency and stress incontinence, as well as symptoms associated with pelvic organ prolapse, such as the feeling of a lump, were recorded.
Each patient underwent a clinical and gynecological examination, including the assessment of avulsion injury of the puborectalis muscle by vaginal palpation and 3-dimensional ultrasound [5,6]. The examination was performed in the dorsal lithotomy position after voiding. An empty bladder was preferred because, from our own experience, a full bladder may displace the neighbouring structures of the anterior compartment and merely impede the prolapse of another compartment. Furthermore, women with a full bladder often perform suboptimal Valsalva manoeuvres because of fear of urinary leakage [7]. The dorsal lithotomy position was preferred, since it is technically simpler and more pleasant for both the patient and the examiner, compared to the standing position. Although in the standing position the structures of the anterior compartment lie lower than in the lithotomy position, the differences are small and not of clinical significance [8]. The relative bladder neck mobility itself is shown not to be affected by the examination position [9,10].
A transperineal ultrasound scan was performed using a Voluson e, GE Healthcare system with a 4-8 MHz volume transducer. To obtain an image in the midsagittal plane, the probe was placed in the patient`s axis between the external urethral orifice and the perineum. Low contact pressure was used to create an image with good resolution without preventing full development of a prolapse [11,12]. All cranial structures were displayed in the upper part of the image in accordance with the recommendations of the German, Austrian and Swiss urogynecological association. The symphysis pubis, the urethra and the bladder were displayed on the right side (ventral). The anal canal, the rectum and the levator ani muscle, presented as a hyperechogenic structure posterior to the anorectal junction, were shown on the left side (dorsal) of the image [13].
For recording a complete examination, the patients were asked to perform a Valsalva manoeuvre by forcefully attempting to exhale against a closed glottis without levator co-activation for at least 5 seconds. This causes a dorsocaudal displacement of the bladder neck and the pelvic organs and can reveal pelvic organ prolapse of various degrees. Real time observations and feedback to the patient was used to ensure an optimal Valsalva manoeuvre.
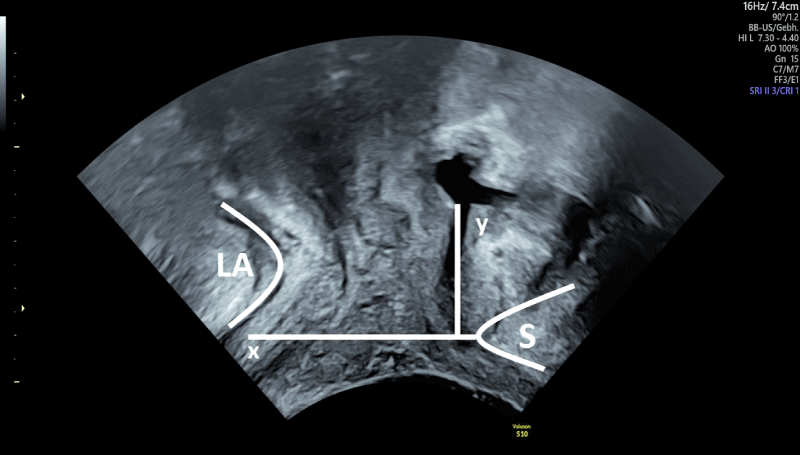
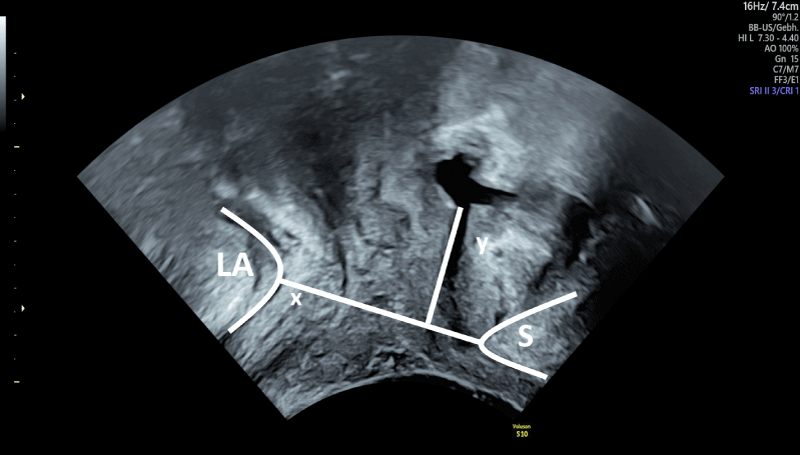
All data were saved for later analysis using the software “4D View” by GE Healthcare. At first, the distance between the bladder neck and the horizontal line, drawn through the lower border of the symphysis pubis, was measured at rest (BNrest_HSL) (Figure 3). Then, the distance of the bladder neck was determined according to the SLL at rest (BNrest SLL) (Figure 4).
Figure 3: Illustation of the horizontal line through the infero-posterior border of the symphysis pubis (HSL), x: HSL Reference line, y: Distance between the referece line and the position of the bladder neck, LA: levator ani muscle, S: symphysis pubis.
Figure 4: Illustation of the Symphysis-Levator Line (SLL), x: SLL Reference line, y: Distance between the referece line and the position of the bladder neck, LA: levator ani muscle, S: symphysis pubis.
Finally, the patients were asked to perform a Valsalva manoeuvre. The position of the bladder neck was once again determined in relation to the HSL (BNval_HSL), and using the SLL (BNval_SLL). The bladder neck mobility (BNm) was defined as the difference between the position of the bladder neck at rest and at maximum Valsalva manoeuvre.
The main question in our study was to determine and compare the extent of agreement between the two methods for estimating the bladder neck mobility. The same procedure was performed again three months later by the same investigator (A.D.) in a sample of 44 patients to ensure reliability. The reproducibility of each method was determined after separate analysis of a sample of 15 patients by a second investigator (S.A.), who was blinded to the measurements of the first one.
Further, given that the study population was heterogeneous, we investigated the influence of various factors and patient characteristics on the measurements obtained using the two methods.
Compliance with ethical standards
No funding was provided for this study.
All authors declare that they have no conflict of interest.
All procedures performed in this study were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments. Due to the retrospective nature of the study and the fact that all data presented were collected during standard clinical care, the local ethics committee (Medical Board of the State of Rheinland-Pfalz) waived the requirement for a formal ethic approval. Informed written consents was obtained from all participants included in this study for the use of their data.
Statistical analysis
For statistical analysis we used the Student´s t - test to compare normally distributed data. When two related samples were to be compared the t-test for two correlated samples was used. The test procedure of Maloney/Rastogi was applied for the comparison of precisions in paired data. Pearson´s correlation coefficient, r, was derived to evaluate the strength and direction of correlation. Spearmans rank correlation coefficient, rs, was used to assess the effect of parity and univariate analysis the effect of the delivery mode on bladder neck mobility. Intraclass correlation coefficient (ICC) was used in test-retest, intrarater, and interrater reliability analysis. A p - value of < 0.05 was considered statistically significant for each test and each correlation coefficient.
A total of 111 patients were included in this retrospective study. Mean age at the time of the examination was 61.66 years (range 30-89 years) and the mean BMI 26.70 kg/m2. Among all patients, there were 40 women presenting with stress urinary incontinence (36%), 46 with symptoms indicating an overactive bladder (41.4%) and 25 (22.5%) with symptoms of both stress and urgency. Symptoms of prolapse were stated by 20 patients (18%). Information about the obstetric history was available for 85 patients. An intact levator ani was documented on 59 patients, whereas 21 patients had a unilateral levator ani avulsion injury. A bilateral levator ani avulsion was not observed in our study population.
The mean, minimum, maximum and standard deviation of the measurements assessed using the HSL method and the SLL at rest and during Valsalva manoeuvre respectively, as well as the calculated values for the bladder neck mobility are listed on tables 1-3. Centimetres were used as metric unit of the measurements. Analog to the POPQ-method, negative values imply that the bladder neck was positioned above the reference line.
Compared to the SLL, using the HSL reference line, we documented significantly higher numerical values for the position of the bladder neck, both at rest as well as during Valsalva (Tables 1,2). The closer distance of the SLL to the bladder neck explains this difference. In order to examine the extent of agreement between the two methods, the Pearson correlation coefficient was calculated. We found a value of r = 0.98499, which indicates a strong linear positive relationship between the two data series. Furthermore, we found that the horizontal line produced larger numerical values for the bladder neck descent than the SLL (median 0.164 cm, p < 0.0001 [CI 0.1223-0.2056]). The test procedure of Maloney/Rastogi was applied for the comparison of precisions in the two data series. The statistical analysis showed that the novel method measured more precise (p < 0,0001). The fact that the values for the bladder neck mobility using the SLL showed a smaller scatter of the data (recognizable by the standard deviations, Table 3) also supports this conclusion. In some cases, however, high deviations were detected. The differences between the two methods were more significant when high bladder neck mobility values were measured (p < 0.0001) and in patients with a high BMI (p = 0.2387).
| Table 1: Position of the bladder neck at rest. | ||||
| Mean | Minimum | Maximum | Std. dev. | |
| BNrest_SLL | -1.902 | -4.560 | -0.640 | 0.547 |
| BNrest_HSL | -2.382 | -5.140 | -0.720 | 0.532 |
| BNrest_diff | -0.408 | -0.880 | -0.080 | 0.143 |
| BNrest_SLL: position of the bladder neck relative to the SLL at rest, BNrest_HSL: position of the bladder neck relative to the HSL at rest, BNrest_diff: difference BNrest_HSL-BNrest_SLL, Std. dev: standard deviation | ||||
| Table 2: Position of the bladder neck during Valsalva manoeuvre. | ||||
| Mean | Minimum | Maximum | Std. dev. | |
| BNval_SLL | -0.195 | -2.130 | 2.300 | 1.073 |
| BNval_HSL | -0.475 | -2.540 | 2.250 | 1.182 |
| BNval_diff | -0.280 | -0.810 | 3.260 | 0.410 |
| BNval_SLL: position of the bladder neck relative to the SLL during Valsalva manoeuvre, BNval_HSL: position of the bladder neck relative to the HSL during Valsalva manoeuvre, BNval_diff: difference BNval_HSL-BNval_SLL, Std. dev.: standard deviation | ||||
| Table 3: Bladder neck mobility. | ||||
| Mean | Minimum | Maximum | Std. dev. | |
| BNm_SLL | 1.707 | 0.030 | 5.080 | 1.032 |
| BNm_HSL | 1.871 | 0.020 | 5.880 | 1.148 |
| BNm_diff | 0.164 | -0.270 | 0.800 | 0.221 |
| BNm_SLL: mobility of the bladder neck calculated using the SLL, BNm_HSL: mobility of the bladder neck calculated using HSL, BNm_diff: difference BNm_HSL-BNm_SLL, Std. dev.: standard deviation | ||||
The first investigator (A.D.) analysed the data of 44 patients once again three months later to ensure reliability (Intrarater reliability). The position of the bladder neck at rest and during Valsalva manoeuvre was once more determined, and bladder neck mobility was recalculated. No significant differences between the initial values and the values assessed three months later by the same investigator were detected.
A second investigator (S.A.), who was blinded to the results of the first one, analysed the images of 15 patients to examine reproducibility (Interrater reliability). The comparison of the measurements indicated a strong positive correlation for both methods.
Given that the study population was heterogeneous, we decided to examine the influence of various factors and patient characteristics on the bladder neck mobility measurements, that were obtained using both methods. We chose to investigate the influence of patients´ age, body mass index, mode of delivery, parity, type of pelvic floor dysfunction (symptoms of stress urinary incontinence, overactive bladder syndrome and pelvic organ prolapse) and the presence of a levator ani avulsion injury. Table 4 summarises the tests that were used for statistical analysis, as well as the obtained p-values. We could not demonstrate a significant influence of any of the above-mentioned factors on the bladder neck mobility, irrespective of the method used.
Since one of the anatomical landmarks that define the SLL is the anterior margin of the puborectalis muscle, special attention was paid on the influence of a levator ani avulsion injury on the obtained measurements for the bladder neck descent. The t - test was applied to compare patients with intact levator ani and patients with a levator ani injury. The obtained p - values showed that there was no statistically significant difference between the two groups, irrespective of the method used (p = 0,7777 for the HSL, p = 0,7092 for SSL) (Table 4).
| Table 4: Influence of patient characteristics on the bladder neck mobility assessed using the HSL and SLL method. | |||
| Patient characteristics | Statistical analysis | HSL method | SLL method |
| Age | Pearson´s correlation coefficient | r = -0,11661 p = 0,2229 |
r = -0,10281 p =0,2830 |
| BMI | r = 0,11609 p = 0,2360 |
r = 0,07801 p = 0,4267 |
|
| Mode of delivery | Univariate analysis | p = 0,8762 | p = 0,8952 |
| Parity | Spearman´s rank correlation coefficient | rs = 0,03799 p = 0,7300 |
rs = 0,04398 p = 0,6894 |
| Stress urinary incontinence | t - Test | p = 0,3843 | p = 0,2836 |
| Overactive bladder syndrome | p = 0,5322 | p = 0,3788 | |
| Pevic organ prolapse | p = 0,3182 | p = 0,4357 | |
| Levator ani avulsion injury | p = 0,7777 | p = 0,7092 | |
| HSL: Horizontal Symphysis Line, SLL: Symphysis-Levator Line, BMI: Body Mass Index, r: Pearson´s correlation coefficient, rs: Spearman´s rank correlation coefficient, p: p - value | |||
The primary aim of this study was to introduce a new, reliable and reproducible reference line for 2-dimentional transperineal ultrasound imaging in urogynecology. In order to define a stable reference line, it was essential to use two separate anatomical structures. We compared our method with the widely used horizontal line through the infero-posterior margin of the symphysis pubis, which has been previously described by Dietz (HSL). The main difference between the two lines, is that the novel method uses two anatomical landmarks to define the reference plane according to which the measurements are obtained, whereas for the HSL only the symphysis pubis is needed to define the horizontal plane. As a result, the plane is horizontal only in relationship to the manner in which the image acquisition is chosen. Rocking or tilting of the transducer changes the position of the HSL.
By definition only the dorsocaudal edge of the symphysis pubis needs to be identified to place the SLL: Since the symphysis pubis does not have to be visualised completely, with the novel reference line it is possible to simultaneously display all three compartments, even in women with a wide genital hiatus [14]. We included the puborectalis muscle in the definition of the novel SLL. As part of the levator ani muscle complex, the puborectalis muscle plays a major role in the function of pelvic support and urinary continence mechanism [15]. This 2-point fixation of the SLL on two anatomical landmarks (analogue to the plane of the minimal hiatal dimensions) differentiates the new method from the coordinate systems used so far. It also ensures the stability of the reference plane during Valsalva manoeuvre and contraction of the pelvic floor and explains the difference in precision in favour of the SLL. In addition, the need to capture both bordering structures, the pubic symphysis ventrally and the puborectalis muscle dorsally, in order to draw the SSL, ensures that all three compartments are displayed at the same time and leads to images of good quality.
Using the newly introduced SLL to quantify bladder neck descent, we observed that the measured values were lower than the ones measured using the HSL (mean 0.164 cm). Although the differences were generally small and probably not of clinical significance, higher deviations were detected in some cases. The differences were more pronounced in patients with high bladder neck mobility (p < 0.0001) and high BMI (p = 0.23871). Possible explanations for this, could be the impeded identification of the anatomical structures in women with severe pelvic floor pathology and the poor image quality in obese patients.
In order to evaluate the reliability and reproducibility of the two methods, analysis of intraobserver and interobserver variability was performed. The intraclass correlation coefficient was calculated for each method respectively and indicated strong agreement. Our data suggests that both methods show high intra- and interobserver agreement in assessing bladder neck mobility.
Furthermore, we examined the influence of various patient characteristics (age, body mass index, mode of delivery, parity, type of pelvic floor dysfunction) on bladder neck mobility using both methods and, as stated on Table 4, we could not a demonstrate a significant influence of any of these on the obtained values.
Finally, since one of the two landmarks that define the novel SSL is the anterior margin of the levator ani muscle, we investigated if the presence of a levator ani injury affects the bladder neck mobility. Even though a levator ani avulsion injury has been associated with a wider genital hiatus and an increased risk for development of pelvic organ prolapse later in life, controversy exists in the literature with regard to its association with urinary stress incontinence [16-19]. In terms of pelvic floor imaging, scarce data exist regarding the influence of this injury on the mobility of the urethra and bladder neck. Dietz and Lanzarone could demonstrate that levator injury is associated with increased bladder neck mobility in the postpartum period in a prospective study which included 61 women [20]. We examined the influence of the levator status on the bladder neck mobility and could demonstrate no significant difference in the obtained values between patients with intact levator ani and patients with a levator ani injury, irrespective of the method used (HSL or SSL).
Even though bladder neck descent has been a major focus of research for urogynecologists and has been used in routine clinical diagnostics for decades, there is still uncertainty concerning its correlation with pelvic floor pathology. Even though a hypermobile urethra is precepted to be associated with stress urinary incontinence, to date, there are neither universally accepted normal values, nor a definition for abnormal bladder neck mobility [21,22]. Several studies showed large differences between young nulligravid women and significant overlap between continent and incontinent patients. Dietz, et al. for instance, suggested a mean value of 17.3 mm as normal in young nulligravid women. In this study the values varied enormously between 1.2 mm to 40.2 mm, and a value greater than 35 mm defined hypermobility of the bladder neck [23]. The same author defined a value higher than 25 mm as abnormal bladder neck mobility in a retrospective study, which included 429 patients presenting with lower urinary tract dysfunction and/or pelvic organ prolapse [22]. These results are similar to those of a second smaller study in nulligravid women (mean 14 mm, SD 9 mm) [24], which used the central line of the symphysis pubis, described by Schaer, et al., as reference line [4]. In contrast, much lower values between 0 and 18.7 mm (median 6.3 mm) were described by Reed, et al. in a population of nulligravid volunteers [25]. The discrepancies above described are most likely due to methodological differences concerning the design of the studies and lack of standardisation (concerning proper Valsalva, patient position and bladder filling for example).
The main limitation of this study is its retrospective character. Even though transperineal ultrasound scans are performed in a standardised way in our department, the examinations were carried out as part of the routine clinical consultation and not for the purposes of the study. This resulted in having to exclude patients because of incomplete medical history or poor sonographic identification of anatomical structures of the pelvic floor. Another possible limitation of the study is that avoiding levator co-activation during Valsalva manoeuvre is difficult to achieve voluntarily, especially in nulliparous women. Even though real time observations and feedback to the patients were used to correct suboptimal attempts, levator co-activation during Valsalva presents a substantial confounder that affects pelvic organ descent [7].
Transperineal ultrasound and measurements of the functional anatomy of the pelvic floor are an integral part of the urogynecological examination. We developed a new, reliable and reproducible reference line to quantify the mobility of the bladder neck using transperineal ultrasound. The 2-point fixation of the SLL on two anatomical structures differentiates the new line from the methods used to date and ensures the stability of the reference plane during the functional changes of the pelvic floor. The SLL could be a useful tool in the hands of urogynecologists in the future.
- Jamard E, Blouet M, Thubert T, Rejano-Campo M, Fauvet R, et al. Utility of 2D-ultrasound in pelvic floor muscle contraction and bladder neck mobility assessment in women with urinary incontinence. J Gynecol Obstet Hum Reprod. 2020; 49: 101629. PubMed: https://pubmed.ncbi.nlm.nih.gov/31499282/
- Dietz HP. Why pelvic floor surgeons should utilize ultrasound imaging. Ultrasound Obstet Gynecol: 2006; 28: 629-634. PubMed: https://pubmed.ncbi.nlm.nih.gov/17001745/
- Dietz HP, Wilson PD. Anatomical assessment of the bladder outlet and proximal urethra using ultrasound and videocystourethrography. Int Urogynecol J Pelvic Floor Dysfunction. 1998; 9: 365-369.
- Schaer GN, Koechli OR, Schuessler B, Haller U. Perineal ultrasound for evaluating the bladder neck in urinary stress incontinence. Obstet Gynecol. 1995; 85: 220-224. PubMed: https://pubmed.ncbi.nlm.nih.gov/7824234/
- Dietz HP, Bernardo MJ, Kirby A, Shek KL. Minimal criteria for the diagnosis of avulsion of the puborectalis muscle by tomographic ultrasound. Int Urogynecol J. 2011; 22: 699-704. PubMed: https://pubmed.ncbi.nlm.nih.gov/21107811/
- Dietz HP, Shek KL. Tomographic ultrasound imaging of the pelvic floor: which levels matter most? Ultrasound Obstet Gynecol : the official journal of the International Society of Ultrasound in Obstet Gynecol. 2009; 33: 698-703. PubMed: https://pubmed.ncbi.nlm.nih.gov/19434620/
- Orno AK, Dietz HP. Levator co-activation is a significant confounder of pelvic organ descent on Valsalva maneuver. Ultrasound Obstet Gynecol : the official journal of the International Society of Ultrasound in Obstet Gynecol. 2007; 30: 346-350. PubMed: https://pubmed.ncbi.nlm.nih.gov/17702054/
- Dietz HP, Clarke B. The influence of posture on perineal ultrasound imaging parameters. Int Urogynecol J and pelvic floor dysfunction. 2001; 12: 104-106. PubMed: https://pubmed.ncbi.nlm.nih.gov/11374506/
- Mouritsen L, Bach P. Ultrasonic evaluation of bladder neck position and mobility: the influence of urethral catheter, bladder volume, and body position. Neurourol Urodyn. 1994;13: 637-646.
- Wen L, Zhao B, Chen W, Qing Z, Liu M. Real-time assessment of the behaviour of the bladder neck and proximal urethra during urine leaking in the cough stress test (CST) in supine and standing positions using transperineal ultrasound. Int Urogynecol J. 2020. PubMed: https://pubmed.ncbi.nlm.nih.gov/32291473/
- Dietz HP. Pelvic floor ultrasound: a review. American journal of Obstet Gynecol. 2010; 202: 321-334. PubMed: https://pubmed.ncbi.nlm.nih.gov/20350640/
- Tunn R, Petri E. Introital and transvaginal ultrasound as the main tool in the assessment of urogenital and pelvic floor dysfunction: an imaging panel and practical approach. Ultrasound Obstet Gynecol : the official journal of the International Society of Ultrasound in Obstet Gynecol. 2003; 22: 205-213.
- Interdisciplinary S2k Guideline: Sonography in Urogynecology: Short Version AWMF Registry Number: 015/055. (Gebfra 2014).
- Albrich SB. Urogenitalsonographie des weiblichen Beckenbodens Ultraschalldiagnostik bei urogynäkologischen Fragestellungen. Gynäkologe. 2018; 51: 208-216.
- Herschorn S. Female pelvic floor anatomy: the pelvic floor, supporting structures, and pelvic organs. Reviews in urology. 2004;6 Suppl 5: S2-s10. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1472875/
- Dietz HP, Shek C, De Leon J, Steensma AB. Ballooning of the levator hiatus. Ultrasound Obstet Gynecol : the official journal of the International Society of Ultrasound in Obstet Gynecol. 2008; 31: 676-680. PubMed: https://pubmed.ncbi.nlm.nih.gov/18470963/
- Dietz HP, Simpson JM. Levator trauma is associated with pelvic organ prolapse. BJOG 008; 115: 979-984. PubMed: https://pubmed.ncbi.nlm.nih.gov/18503571/
- Shek KL, Pirpiris A, Dietz HP. Does levator avulsion increase urethral mobility? European journal of obstetrics, gynecology, and reproductive biology. 2010; 153: 215-219.
- Dietz HP, Kirby A, Shek KL, Bedwell PJ. Does avulsion of the puborectalis muscle affect bladder function? Int Urogynecol J Pelvic Floor Dysfunction. 2009; 20: 967-972.
- Dietz HP, Lanzarone V. Levator trauma after vaginal delivery. Obstet Gynecol. 2005; 106: 707-712. PubMed: https://pubmed.ncbi.nlm.nih.gov/16199625/
- Viereck V, Pauer HU, Hesse O, Bader W, Tunn R, et al. Urethral hypermobility after anti-incontinence surgery - a prognostic indicator? Int Urogynecol J and pelvic floor dysfunction. 2006; 17: 586-592.
- Naranjo-Ortiz C, Shek KL, Martin AJ, Dietz HP. What is normal bladder neck anatomy? Int Urogynecol J. 2016; 27: 945-950. PubMed: https://pubmed.ncbi.nlm.nih.gov/26700104/
- Dietz HP, Eldridge A, Grace M, Clarke B. Pelvic organ descent in young nulligravid women. American journal of Obstet Gynecol. 2004; 191: 95-99. PubMed: https://pubmed.ncbi.nlm.nih.gov/15295348/
- Peschers UM, Fanger G, Schaer GN, Vodusek DB, DeLancey JO, et al. Bladder neck mobility in continent nulliparous women. BJOG. 2001; 108: 320-324. PubMed: https://pubmed.ncbi.nlm.nih.gov/11281475/V
- Reed H, Freeman RM, Waterfield A, Adekanmi O. Prevalence of bladder neck mobility in asymptomatic non-pregnant nulliparous volunteers. BJOG. 2004; 111: 172-175.