More Information
Submitted: 18 August, 2020 | Approved: 29 August 2020 | Published: 31 August 2020
How to cite this article: Yang S, Bhatnagar R, Byrne J, Jelks A. Universal testing for severe acute respiratory syndrome coronavirus 2 upon admission to three labor and delivery units in Santa Clara County, CA. Clin J Obstet Gynecol. 2020; 3: 109-113.
DOI: 10.29328/journal.cjog.1001060
Copyright License: © 2020 Yang S, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Labor and delivery; Coronavirus disease 2019; Severe acute respiratory syndrome coronavirus 2; Pregnancy
Universal testing for severe acute respiratory syndrome coronavirus 2 upon admission to three labor and delivery units in Santa Clara County, CA
Sophia Yang1, Rishi Bhatnagar1, James Byrne1-3 and Andrea Jelks1*
1Department of Obstetrics and Gynecology, Santa Clara Valley Medical Center, San Jose, CA,USA
2Department of Obstetrics and Gynecology, O’Connor Hospital, San Jose, CA, USA
3Department of Obstetrics and Gynecology, St Louise Regional Hospital, San Jose, CA, USA
*Address for Correspondence: Andrea Jelks, MD, Maternal Fetal Medicine, Department of Obstetrics and Gynecology, Santa Clara Valley Medical Center, San Jose, CA, Department of OBGYN 751 S. Bascom Ave San Jose, CA 95128, USA, Tel: 408-236-0598; Email: [email protected]
Objective: To determine the prevalence of patients with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in labor and delivery units in one of the epicentres of the West Coast.
Study Design: This was a retrospective chart review of patients admitted to labor and delivery from April 15, 2020-May 15, 2020 after implementation of a universal testing policy on Labor and Delivery.
Results: The prevalence of patients with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in the admitted labor and delivery population was 2.5%, of whom 87.5% were asymptomatic.
Conclusion: We present additional data on the prevalence of asymptomatic SARS-CoV-2 in pregnant patients on the West Coast, which is much lower compared to other locales, possibly as a result of aggressive ‘shelter in place’ policy. Universal screening is insufficient to detect asymptomatic SARS-CoV-2 and thus rapid, universal testing should be prioritized for labor and delivery units for the protection of patients and staff, and to better allocate appropriate resources.
Key points:
1. 2.5% of 320 patients tested positive for SARS-CoV-2.
2. 87.5% of positive patients were asymptomatic.
3. Universal testing on labor and delivery is necessary.
4. ‘Shelter-in-place’ policies reduced SARS-CoV-2.
Since the novel coronavirus disease 2019 (COVID-19) was first identified in China in late 2019, the disease has spread over all continents and affected all areas of life. Within the context of the pandemic, pregnant women are a unique population in society and within the healthcare system, as their care is highly time sensitive and inherently involves contact with healthcare providers. As of this submission, recommendations from the CDC and ACOG states, ‘consider universal testing as the potential for asymptomatic patients presenting to labor and deliveries in high prevalence areas, and continue to prioritize testing for symptomatic individuals requiring hospital admission, symptomatic first responders and/or residents in congregate living settings [1,2]. Recent reports of universal severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) testing in labor and delivery units in the New York and London areas have shown a high proportion of asymptomatic patients among women testing positive for SARS-CoV-2 [3-5]. Given the much higher disease prevalence in those areas, it is unclear how generalizable that information is to other geographic areas with lower rates of SARS-CoV-2 prevalence.
Santa Clara County, California, emerged as an early focus of COVID-19 disease activity and was the home of the nation’s first shelter-in-place order on March 16, 2020 [6]. It remains one of the most affected counties in the San Francisco Bay Area, albeit with a per-capita COVID-19 rate substantially lower than New York [6]. Hospitals in the Santa Clara County Health and Hospital system were some of the first institutions on the West Coast to implement universal testing of all patients admitted to labor and delivery to both guide care and determine the incidence of SARS-CoV-2 infections in both symptomatic and asymptomatic pregnant patients.
We performed a retrospective cohort study of all maternal admissions in the Santa Clara County health and hospital system between April 15 and May 15, 2020, during which all women admitted to Labor and Delivery units were tested for SARS-CoV-2, regardless of symptoms. Santa Clara County health system is a safety-net three-hospital system in the heart of Silicon Valley performing a total of approximately 4100 deliveries per year. IRB approval was granted for this study.
All patients presenting to Labor and Delivery were queried about symptoms possibly suggestive of COVID-19, including cough, shortness of breath, fevers, myalgias, and/or close contact with a known COVID-19 case (Box 1). Nasopharygeal swabbing was performed by a trained nurse or physician in a negative pressure room or other specially designated room, using the Cepheid GeneXpert® Xpress SARS-CoV-2 Assay (Cepheid, Sunnyvale, CA). This is a cartridge-based, rapid test that detects the viral Envelope (E) and Nucleocapsid (N) gene targets (2). The E target shares sequence homology with the SARS-CoV-1 and with other bat-associated coronaviruses whereas the N target sequence is unique to the SARS-CoV-2. The Xpress assay has a claimed limit of detection of 250 copies/ml. Separate in house laboratory comparisons showed 100% agreement between the Cephepid GeneExpert assay and the more labor-intensive CDC 2019-nCoV Real-Time RT-PCR Diagnostic Panel. Expected turnaround time was approximately 1.5-2 hours from receipt in the lab.
| Box 1: Universal COVID-19 Screening Questions |
| High Risk Factors: |
| Have you been tested for COVID (coronavirus)? |
| If yes, what were the results, when tested, where tested, and why tested? |
| Have you been exposed to an individual with confirmed COVID 19 w/in last 14 days? |
| Have you had any of the following symptoms currently or w/in last 7 days? |
| fever (subjective or objective > 100.0) AND |
| cough and/or |
| shortness of breath |
| Are you homeless, incarcerated, or live in a group home/shelter or a skilled nursing facility? |
| Low/Moderate Risk Factors: |
| Have you had any of the following symptoms currently or w/in last 14 days? |
| fever (subjective or objective > 100.0) |
| cough and/or |
| shortness of breath |
| Have you had any of the following symptoms currently or within last 14 days? |
| sore throat |
| muscles soreness (myalgias) |
| excessive tiredness (fatigue) |
| nausea/ emesis |
| diarrhea |
| headaches (new for you) |
| loss of sense of smell or taste |
Patients with negative SARS-CoV-2 tests received their care in normal patient rooms. Of note, universal hospital policy throughout this time frame included measuring temperature of all staff, patients and visitors upon hospital entry, required use of surgical facemasks for everyone in the facility, intensified cleaning protocols, and revised layout to help patients and staff maintain social distancing. Visitors were limited to one asymptomatic support person during labor.
Women with positive SARS-CoV-2 test results labored and delivered in a negative pressure room, if available. They were allowed one asymptomatic support person during the active phase of labor. Support persons were not tested for SARS-CoV-2. Providers were minimized to only those essential for care and wore N-95 masks, face shields, gowns and gloves for all encounters. Assessments not requiring a physical exam could be performed via secure video chat using institution-supplied tablet computers equipped with Face Time. Delayed cord clamping was performed with the infant on a clean blanket on mother’s chest at delivery; after cord clamping the infant was kept under the radiant warmer until after the mother changed into a clean gown and performed hand hygiene. Mothers who were SARS-CoV-2 positive were housed in single rooms postpartum. Infant rooming location was determined by shared decision-making between pediatricians and the patient. Mothers who chose to room-in kept their infant in an isolate 6 feet away, and were coached to wear a mask and utilize appropriate hand hygiene prior to breastfeeding or holding their infant.
All new-borns born to mothers who were SARS-COV-2-positive were tested for SARS-CoV-2 at 24 or more hours of life, prior to hospital discharge. After discharge infants were followed by pediatricians via telephone for 14 days. Mothers testing positive for SARS-COV-2 were followed by obstetricians via telephone weekly for two weeks. Both mothers and infants were assessed for development of symptoms or complications of COVID-19 after hospital discharge.
Patient charts are stored on one electronic medical record, EPIC, which is shared between all three hospital sites. EPIC reporting was used to identify the delivered patients and various maternal data points. The authors reviewed the charts of all women admitted during the study period for infectious symptoms while admitted.
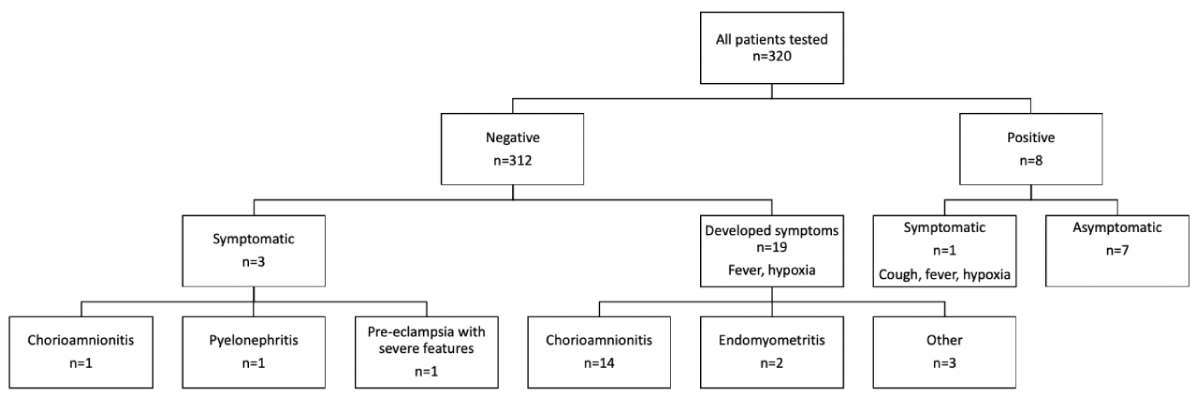
320 women were tested for SARS-CoV-2 on admission to Labor and Delivery between April 15th and May 15th. Our patient population was primarily Hispanic (64.4%), English speaking (60%), and with an average maternal age of 29.4 years (Table 1). 82.2% receive coverage through Medi-Cal, California’s version of Medicaid. 24.4% delivered by cesarean section. Of all tested patients (n = 320), 8 were positive (2.5%) for SARS-CoV-2 (Figure 1). Of those who tested positive for SARS-CoV-2 on admission, one was symptomatic with a cough, fever, and hypoxia (12.5%) at 23 weeks gestation. She did not require ICU admission or intubation, and was discharged undelivered in good condition 6 days later. Of the 7 women with asymptomatic COVID on admission, all underwent uncomplicated term deliveries, and all remained asymptomatic throughout delivery and hospitalization.
| Table 1: Demographics of all maternal admissions tested for SARS-CoV-2. | |
| Demographics | All maternal admissions (n = 320) |
| Age (y) | 29.4 ± 6.5 |
| Race | |
| Hispanic | 206(64.4) |
| White | 33(10.3) |
| Asian | 50(15.6) |
| Black | 12(3.8) |
| Multiple | 11(3.4) |
| Declined | 6(1.9) |
| Other | 2(0.6) |
| Primary Language | |
| English | 193(60) |
| Spanish | 101 (32) |
| Vietnamese | 8(2.5) |
| Other | 18 (5.6) |
| Insurance | |
| Medi-cal | 263(82.2) |
| Commerical | 51(15.9) |
| No insurance | 6(1.9) |
| Mode of delivery | |
| Vaginal | 237(74.1) |
| Cesarean | 78(24.4) |
| Undelivered | 5(1.6) |
| Data are mean ± standard deviation or n (%) Percentages may not add up to 100% due to rounding error |
|
Figure 1:
Of the 312 women who tested negative for SARS-CoV-2 on admission, 3 were symptomatic on admission—two with fever and one with cough and hypoxia. The final diagnoses in these cases were chorioamnionitis, pyelonephritis, and pre-eclampsia with severe features and heart failure. During hospitalization, 19 patients further developed symptoms—all had fever and one additionally had hypoxia. Additionally, two of these patients met sepsis criteria. The most common final diagnoses in these cases were chorioamnionitis (14/19, 73.7%) and endomyometritis (2/19, 10.5%). Repeat SARS-CoV-2 testing was performed in one case 2 days after admission due to symptoms of shortness of breath and hypoxia; repeat testing was negative and the patient was managed for pulmonary edema related to preeclampsia.
The sensitivity, specificity, positive and negative predictive values of symptoms for positive SARS-COV-2 testing on admission to Labor and delivery were 1/8(12.5%), 309/312(99.0%), 1/4(25.0%) and 309/316(97.8%), respectively. Use of intensified PPE was lower when guided by results of universal COVID testing: based on symptoms, 23/320 (7.2%) patients would have required intensified PPE use; based on test results, only 8/320 (2.5%) patients actually required intensified PPE use, an absolute difference of 15/320 (4.7%).
All seven delivered newborns of SARS-COV-2-positive mothers were themselves tested for SARS-COV-2, and all were negative (0/7, 0%). None developed any symptoms concerning for COVID-19 in the 14 days after delivery. Of the 7 mothers’ positive for SARS-COV-2 who remained asymptomatic during hospitalization, six remained asymptomatic within 1 and 2 weeks after discharge, and one was lost to follow-up. The one patient with symptomatic COVID-19 during hospitalization reported recovery at 2 weeks.
Our finding that 2.5% of women were positive for SARS-COV-2 on admission to labor and delivery units in Santa Clara County contrasts sharply with the considerably higher of 15.5% and 19.9% reported from two hospitals in the New York-area during March and April of 2020 [3,4]. Other locales outside the United States have also reported higher incidence of positive SARS-COV-2 tests in women admitted to L&D, with one study reporting 7% in London during March and April of 2020 [5]. In all of these studies, screening questions were used to determine symptoms, though ours was the most comprehensive, reflecting updated knowledge about subtle symptoms of COVID-19. All used PCR testing, though provided by different companies.
One potential explanation for the lower rate in the current study may be a result of early adoption of ‘shelter in place’ and other aggressive containment strategies in Santa Clara County, which has resulted in cumulative incidence of 129.3 per 100,000 population as of the date of this submission, as compared to a cumulative incidence of 1466.7 and 2910.8 cases per 100K population in New York and Nassau counties, respectively as of mid-May 2020 [7,8].
Our study has two findings that are notably similar to previous reports: case rates on L&D were substantially higher than reported background community rates at the time, and most women who tested positive under universal screening were asymptomatic. During the 30 days of our study, Santa Clara County reported 502 new cases of SARS-CoV-2, which corresponds to 0.03% of the county population experiencing a new diagnosis SARS-CoV-2 during this time period [7]. Our finding that 2.5% of women admitted to labor and delivery at our hospitals tested positive is nearly 100-fold higher than would be expected based on the background community rate. Large discrepancies between rates of cases diagnosed on labor and delivery versus COVID case rates in the wider community are noted in New York and Nassau counties, as well [3,4,8]. Despite dramatically different absolute rates of SARS-COV-2 infections between these three counties, however, it is likely that asymptomatic cases are being missed in the general population by testing protocols focused on symptoms, contacts and travel history. Universal testing of women admitted to Labor and delivery indicates what is likely to be a truer reflection of SARS-CoV-2 incidence in the wider community.
It is of importance to note that most of our patients, both affected and unaffected, are Hispanic. This is reflected in the larger data in Santa Clara County, where cumulative cases stratified by race/ethnicity reveal that Hispanic patients are disproportionately affected by COVID-19. They comprise 26% of the population but represent 39% of the cases [7]. This contrasts with the White population, which comprises 32% of the population and 18% of cases. The majority of affected patients in our cohort resided in three of the most affected zip codes in the Santa Clara county region [7]. This can be in part explained by the overrepresentation of Hispanic workers in roles considered to be ‘essential’ and as such often precludes working from home and reducing exposure to SARS-CoV-2 [9]. They are also more likely to live in denser housing, particularly in expensive urban areas, and thus have more risk of exposure through household contacts [10]. When considering policy for relief during the COVID-19 pandemic it is imperative to consider these social determinants of health.
Knowledge of both positive and negative SARS-CoV-2 test results affected patient care on Labor and Delivery in numerous ways. When caring for a woman with known SARS-CoV-2 infection, providers intensified PPE use, using gowns, gloves, face shields, and N-95 masks in all patient encounters. We found that requirements for PPE use overall was reduced under a strategy of universal testing, which contrasts with a prior study showing a 10% increase in PPE use under universal testing [3]. In addition, staff and providers indicated that they felt less anxious caring for patients with known SARS-CoV-2 status as this allowed for appropriate protective measures, which is consistent with other reports [11].
Women who were SARS-COV-2 positive were recommended to have epidurals during labor to limit the likelihood of needing intubation if emergent Caesarean were required to reduce aerosolization. Oxygen therapy was avoided unless indicated for maternal hypoxia to minimize aerosolization of viral particles. Airflow and cleaning of rooms and equipment were enhanced to minimize risk of contamination through ventilation systems or via surfaces. Mothers who were SARS-COV-2-positive were roomed individually in the postpartum ward, whereas mothers who tested negative could be double roomed if census required. Finally, after discharge, mothers who were SARS-COV-2-positive and other household members were kept out of pediatric clinics until 14 days later. It was also reassuring that new-borns of patients with positive tests showed no evidence of transmission of infection either at birth or at follow-up. A recent meta-analysis has suggested that vertical transmission occurs rarely, and does not seem to be associated with severe neonatal disease, though much remains unknown [12].
Pregnant women are a unique population in society and within the healthcare system. Unlike other patients pondering appropriate timing of “elective” surgeries or postponing other care, pregnant women admitted for delivery or antepartum complications generally do not have the option of delaying their care significantly to await a reduction in COVID-19 incidence. Care of laboring and delivering women inherently requires patient contact, and aerosol generation is plausible during heavy maternal breathing in the second stage of labor. Risk of healthcare worker infection has been associated with time spent and proximity to an infected patient, as well as with dyspnoeic breathing and oxygen facemask therapy [13]. Universal precautions, such as masking, may not prevent transmission related to environmental contamination. In addition, some patients may not tolerate wearing a mask at all times, especially during the second stage of labor.
The availability of rapid SARS-CoV-2 testing was a vital factor allowing routine SARS-CoV-2 testing to occur with limited disruption in overall patient care. Routine testing protocol required distinct rooms set aside for swabbing and patient isolation while awaiting results. Non-urgent patient care, such as labor induction, was delayed during this time, inevitably extending the total time patients spent on the L&D unit. However, initiation of antibiotics, patient request for epidural, and other necessary care was not delayed. As more hospitals consider testing asymptomatic individuals in advance of admission or elective surgeries, more efficient or offsite testing protocols could be considered. Inevitably some testing will remain necessary on L&D units themselves.
Our study is one of the first in California to estimate the prevalence of SARS-CoV-2 in the obstetric population. As localities begin to slowly reopen their economies and relax social distancing orders, awareness of asymptomatic carriers will become paramount to controlling further outbreaks especially in health care settings.
In conclusion, we found 2.5% of patients admitted to labor and delivery units in Santa Clara County tested positive for SARS-CoV-2, 87.5% of whom were asymptomatic. This knowledge has important implications for care planning in this vulnerable population as they interact with the healthcare system.
- Center for Disease Control. Evaluating and Testing Persons for Coronavirus Disease 2019 (COVID-19). 2020. https://www.cdc.gov/coronavirus/2019-nCoV/hcp/clinical-criteria/html
- The American College of Obstetrics and Gynecology. Novel Coronavirus 2019 Practice Advisory. 2020. https://www.acog.org/clinical/clinical-guidance/practice-advisory/articles/2020/03/novel-coronavirus/2019
- Vintzileos WS, Muscat J, Hoffmann E, John S, Vertichio R, et al. Screening all pregnant women admitted to Labor and Delivery for the virus responsible for COVID-19. Am J Obstet Gynecol. 2020; 223: 284-286. PubMed: https://pubmed.ncbi.nlm.nih.gov/32348743/
- Bianco A, Buckley AB, Overbey J, Smilen S, Wagner B, et al. Testing of Patients and Support Persons for Coronavirus Disease 2019 (COVID-19) Infection Before Scheduled Deliveries. Obstet Gynecol. 2020; 136: 283-287. PubMed: https://pubmed.ncbi.nlm.nih.gov/32433448/
- Khalil A, Hill R, Ladhani S, Pattisson K, O’Brien P. Severe acute respiratory syndrome coronavirus 2 in pregnancy: symptomatic pregnant women are only the tip of the iceberg. Am J Obstet Gynecol. 2020; 223: 296-297. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7204681/
- California Department of Public Health. Covid-19 Updates. 2020. https://www.cdph.ca.gov/Programs/CID/DCDC/Pages/Immunization/ncov2019/aspx
- Santa Clara County Public Health County of Santa Clara Emergency Operations Center, Coronavirus (COVID-19) Data Dashboard. 2020. https://www.sccgov.org/sites/covid19/Pages/dashboard/aspx
- Johns Hopkins University & Medicine, Coronavirus Resource Center. 2020. https://coronavirus.jhu.edu/us/map
- Branson-Potts H, Reyes-Velarde A, Stiles M, Campa AJ. The price of being ‘essential’: Latino service workers bear brunt of coronavirus. Los Angeles Times. 2020. https://www.latimes.com/california/story/2020-05-17/latino-essential-workers-coronavirus
- Palomino J, Sanchez T. Latinos’ coronavirus burden. San Francisco Chronicle. 2020. https://www.sfchronicle.com/bayarea/article/Bay-Area-Latinos-hit-hardest-by-coronavirus-15252632.php
- Bender W, Srinivas S, Coutifaris P, Acker A, Hirshberg A. The psychological experience of obstetric patients and health care workers after implementation of universal SARS-CoV-2 testing. Am J Perinatol. 2020.
- Kotlyar A, Grechukhina O, Chen A, Popkhadze S, Grimshaw A, et al. Vertical transmission of COVID-19: a systematic review and meta-analysis. Am J Obstet Gynecol. 2020. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7392880/
- Wilson NM, Norton A, Young FP, Collins DW. Airborne transmission of severe acute respiratory syndrome coronavirus-2 to healthcare workers: a narrative review. Anaesthesia. 2020; 75: 1086-1095. PubMed: https://pubmed.ncbi.nlm.nih.gov/32311771/