More Information
Submitted: 26 June 2020 | Approved: 06 July 2020 | Published: 07 July 2020
How to cite this article: Darido J, Grevoul Fesquet J, Diari J, El Haddad C, Bouzid N, et al. Hemorrhagic shock due to irreducible uterine torsion in a third trimester twin pregnancy: A case report. Clin J Obstet Gynecol. 2020; 3: 085-089.
DOI: 10.29328/journal.cjog.1001055
Copyright License: © 2020 Darido J, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Uterine; Torsion; Twin; Pregnancy; Maternal; Mortality; Hemorrhagic; Shock
Hemorrhagic shock due to irreducible uterine torsion in a third trimester twin pregnancy: A case report
Darido J1,2*, Grevoul Fesquet J1, Diari J1, El Haddad C1, Bouzid N1, Abou El Hassan N1, Khadam L1 and Rigonnot L1
1Department of Obstetrics and Gynecology, Centre Hospitalier du Sud Francilien, Iles de France, France
2Department of Obstetrics and Gynecology, Faculty of Medical Sciences, Lebanese University, Beirut, Lebanon
*Address for Correspondence: Darido Jessie, Department of Obstetrics and Gynecology, Centre Hospitalier du Sud Francilien, Iles de France, France Tel: 0033 7 54 44 11 80; Email: [email protected]; [email protected]
Uterine torsion is a rare life-threatening event that happens at any age or any gestational age. By definition, it consists of a rotation of more than 45 degrees around the long axis of the uterus. The reported cases have variable presentations. The uterine torsion can happen without any sequelae either for the fetus or the mother. However, fetal and maternal mortalities were also reported in such a case.
We hereby, report the case of a 29-year-old female patient, with previous four Normal Vaginal Deliveries, pregnant with twins, presenting at 36 weeks gestation with an irreducible uterine torsion at the third trimester of her pregnancy complicated by maternal and fetal deaths.
We concluded that the prognosis is improved as long as the management is done rapidly. More data is needed to know about the genetic predilection and the characteristics of imaging workup for a rapid preoperative diagnosis of this condition.
Uterine torsion is a rare life-threatening event that happens at any age of the reproductive period in a patient of any parity number and also if pregnant, at any gestational age. Its incidence is not very well known. By definition, it consists of a rotation of more than 45 degrees around the long axis of the uterus at the level of the cervico isthmic junction [1]. However, the cases that were reported in the literature describe a wider spectrum of a uterine torsion that ranges between 45 degrees and 720 degrees. It occurs most of the time to the right side in the presence of a uterine malformation, fibroids, abnormal presentation or anomalies of the fetus [2,3].
On the other hand, there is a wide range of nonspecific symptoms in the cases of uterine torsion. In fact, the reported cases have either presented with abdominal pain, vaginal bleeding, urinary and intestinal symptoms or have been completely asymptomatic. Also note that sometimes uterine torsion has been revealed via birth obstruction. Uterine torsion is generally managed via an immediate laparotomy where the diagnosis is made intraoperatively most of the time especially if the patient was asymptomatic upon admission.
Note that uterine torsion can happen without any sequelae either for the fetus or the mother. However, fetal and maternal mortalitieswerealso reported in such a case [4,5].
We hereby, report the case of a 29-year-old female patient, pregnant with twins, presenting with an irreducible uterine torsion at the third trimester of her pregnancy complicated by maternal and fetal deaths.
It is a 29-year-old female patient, with previous four Normal Vaginal Deliveries and two abortions, and that is well followed during her current twin dichorionic diamniotic pregnancy. Shehad a normal course with no complications, and no abnormalities on morphoscan. Supplemented by iron due to anemia (hemoglobin 8) associated with asthenia. Pruritus was evaluated by a complete liver enzymes workup that turned back to be normal. At one of her second trimester consults, we have found a blood pressure of 140/80 mmHg spontaneously normalized to 132/84 associated with 0.3 g/l of proteins at the urine dipstick test with no abnormal associated symptoms, no metrorrhagia, no repeat contractions, and a normal preeclampsia workup. No gestational diabetes upon screening.
Prior to her presentation at 36 weeks gestation to a private peripheral clinic, the patient had a severe abdominal pain, associated with nausea and vomiting. No vaginal bleeding, no rupture of membranes. Upon her admission, she was in a deep alteration of her general state, pale and unresponsive to mild to moderate stimuli. Her blood pressure was 80/40 mmHg, pulse 98 bpm. However, her hemodynamic state was deteriorating: the systolic blood pressure decreased to 70 mmHg and the pulse increased to 110 bpm. Hemoglobin was at 5.5 and her clinical symptoms were marked by the aggravation of the abdominal pain with no cervical dilation on physical exam. Hemoglobin decreased to 4.8. In addition, she was severely deteriorating at the neurologic level: Glasgow at 3 with intermediate reactive pupils. Patient was intubated, sedated and transfused with three PRBCs and two FFPs. then, a decision to transfer the patient to our hospital was done.
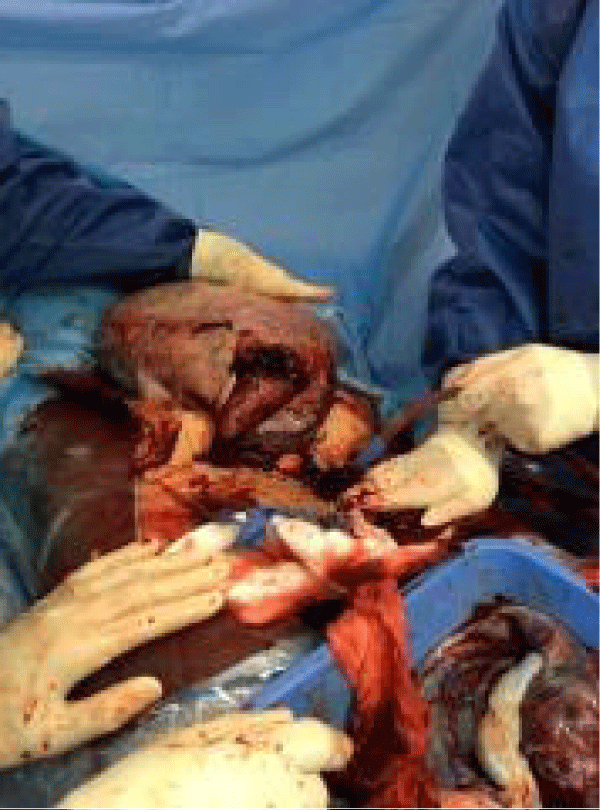
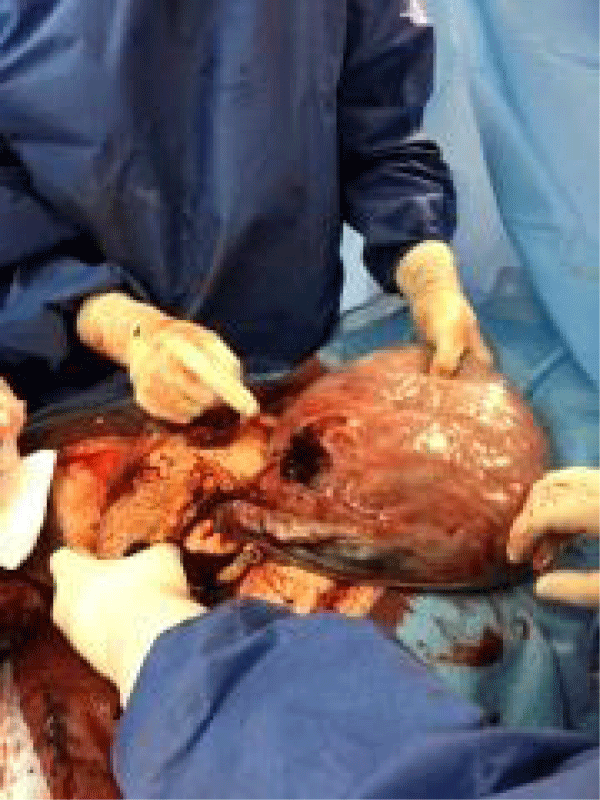
Considering the urgent medical aid service call, where they did not reveal a typical presentation of a retroplacental hemorrhage, the patient was taken in charge by the two seniors that were on duty, one of the two was ready for the incision. The patient was immediately admitted at the operating room. On the operating room table, a rapid ultrasound was performed confirming the absence of cardiac activity for both fetuses driven back at the uterine fundus of the uterus by a very abundant intrauterine collection with no hemoperitoneum ruling out the three main differential diagnoses of hemorrhagic shock during the third trimester: rupture of the splenic arterial aneurysm, uterine rupture and rupture of a peptic ulcer. After scrubbing and draping, incision is done layer by layer until reaching the intraabdominal cavity. A major 180 degrees uterine torsion to the left side was inspected (Figure 1). The detorsion was impossible to be done due to the extremely enlarged uterus (intrauterine blood collection+ two eutrophic fetuses+ the amniotic fluid and placenta). A transverse incision was performed on the posterior wall of the uterus (Figure 2). Three liters of blood were evacuated. Then, amniotomy is done with clear abundant amniotic fluid. Delivery of two dead babies: the first one has a breech presentation, extracted with Lovset and Bracht maneuvers and the second one has a transverse presentation extracted with an internal manual version followed by Bracht and Lovset maneuvers. Then a Manual extraction of complete placentas and membranes is done.
Figure 1: a 180 degrees left sided uterine torsion. At this point, both babies were delivered and the uterus was exteriorized from the abdominal cavity.
Figure 2: The transverse uterine incision that was performed over the posterior wall of the uterus; from lateral to medial: round ligament of the uterus, Uteroovarian ligament and, fallopian tube.
A Manual revision is performed and the uterus was exteriorized from the abdominal cavity. However, a major uterine atony was present along with active bleeding and an estimated blood loss of 4.5 liters (Figure 3). Despite the uterine detorsion, the hemorrhage persisted, and despite the vascular filling and norepinephrine, the hemodynamic instability also persisted. Therefore, a decision of a cesarean hysterectomy of hemostasis was taken.
Figure 3: Uterine Atony after the manual extraction of the placentas.
The round ligaments were clamped, sectioned and ligated with vicryl 0. Broad ligaments were opened, the ureters were identified; The utero-ovarian ligaments along with fallopian tubes at their origins were clamped, sectioned and ligated with vicryl 0, bilaterally. The utero vesical fold was easily dissected. Then, clamping, ligation and section of the uterine pedicles is followed by the same procedure over the cervico-vaginal pedicles using vicryl 0. The Subtotal intra facial hysterectomy is done and both ovaries were preserved. The uterus and placentas were sent to pathology. The cervix is closed with interrupted sutures of vicryl 1.
Intraperitoneal lavage is done. Hemostasis was observed and reassured. A sealant matrixis put at the colpectomy site. Pad count was verified twice. An intracavitary hemovac is introduced. The parietal peritoneum was closed with vicryl 2.0. The fascia is closed with vicryl 1. Staplers are used on the skin. The overall blood loss was estimated at 5500 ml. The urine was clear at the end of the intervention. Antibioprophylaxis was given to the patient as by protocol. The patient was transfused with6 PRBCs and 5 FFPs 1 pack of platelets and 3 g of fibrinogen were transfused intraoperatively.
The hemodynamic state of the patient was better at the end of the intervention and she was transferred to the ICU. Postoperatively, she presented a multiorgan damage with a major metabolic acidosis and acute renal failure, a hepatic insufficiency and disseminated intravenous coagulation (DIC). At the Intensive Care Unit, our patient was hemodynamically unstable; an intraperitoneal hemorrhage was diagnosed on abdominal ultrasound with signs of intestinal ischemia. The general surgeons were consulted on the case and they opted for the reopening at OR in order to stop the bleed. A staff meeting decided to respect the bowel loops if there are no signs of ischemia. Through the same Pfannenstiel incision, the abdominal wall was dissected layer by layer till reaching the intraperitoneal cavity. A massive hemoperitoneum was evacuated. The inspection of the hysterectomy site revealed active bleeding at the right pedicle. Consequently, the latter was clamped and the hemostasis was reassured by two vicryl 0 sutures. An additional suture was done at the left pedicle for security, since the venous ligature became looser with to the resolution of the edema at the postpartum period. Again, the patient was massively hydrated and transfused. Note that on the exploration of the abdominal cavity, we have seen ischemic bruised intestines without any peristaltism and a gray pale colon. The consulted general surgeon considered this ischemia as the result of the norepinephrine treatment. Considering the young age of the patient, a conservative management of the ischemia was decided with no digestive resection. In the presence of the DIC, a total body scan was done postoperatively showing intraparenchymal frontoparietal bilateral petechiae with two left subdural hematomas and a hepatic ischemia with no identification of thrombi. A hepatic transplantation was done at a referral center with double intestinal resection and splenectomy. However, a severe neurologic deterioration followed the procedure with cerebral edema. Brain death was diagnosed with a cerebral angioscanner confirming the absence of cerebral circulation. Patient passed away few time after that.
The pathology result of the two separated placentas concluded to the absence of anomalies in the cords and membranes with no arguments for a vascular or inflammatory pathology. Retroplacental hematoma was not identified in both placentas. As for the uterus, the pathology report mentioned the presence of a hemorrhagic content in the endometrial cavity with no residual placental tissues.
Uterine torsion is considered to be a very rare complication of pregnancy, especially in humans [6]. A review of literature done by Don Wilson, et al. revealed a total of 212 cases reported worldwide until 2006 [7].
Uterine torsion has multiple risk factors:
- Any situation that provokes an asymmetry in the transverse diameter of the uterus (transverse presentation, lateral fibroids, bicornuate uterus, multiple pregnancy).
- Pelvic extrauterine tumors
- Pelvic adhesions
- Morphologic anomalies
However, 16% of the uterine torsion cases have no clear etiology.
As for our patient the major risk factor was multiparity [8].
The first cases of uterine torsion were described in non-pregnant patients who had fibroids. But up till now, uterine torsions due to fibroids are still reported. In fact, Chuan, et al. reported last year a case of uterine torsion with necrosis of bilateral adnexa in a postmenopausal woman where a uterine fibroid was present [9].
The uterine torsion has a very wide range of clinical symptoms and it can be asymptomatic in 14% of the cases. Our case represents the extreme case of hemorrhagic shock. Farhadifar, et al. reported the case of an asymptomatic pregnant woman that was operated of a laparotomy with 180 degrees uterine torsion [10].
Generally, the occurrence of a uterine torsion can be at any gestational age, mostly at the third trimester. Its management is directed by the severity of the symptoms, the gestational age, as well as the presence or not of intraoperative ischemic signs.
Sachan, et al. reported the case of a 45 degrees uterine torsion on a fundal leiomyoma occurring at 15 weeks of pregnancy where the patient presented in a hemorrhagic shock due to severe abruption [3].
Kopko, et al. reported the case of 19 weeks pregnant patient operated of a laparotomy due to acute abdominal pain, intraoperatively the diagnosis of appendicitis with a 100 degrees uterine torsion was done. The uterus was detorsed and the pregnancy continued under close monitoring till 36 weeks where a cesarean was performed [10].
One maternal death and 18 fetal mortalities were reported in the literature from the sixties after 1976 up to 2014 [5,6,11,12]. For example, Cook, et al. reported the case of a pathologic uterine torsion of 270 degrees associated with necrotic uterus and adnexa with placental abruption and consequent maternal shock and intrauterine fetal demise [13].
Rare are the uterine torsions that were reported in twin gestation pregnancies:
- Thubert, et al. reported one of them in 2011 [12].
- Demaria, et al. reported a preterm uterine torsion that happened in a didelphys uterus during a twin pregnancy. The diagnosis of a hemi uterine torsion was done intraoperatively associated with placental abruption [14].
- The third case was reported in 2008 by Joseph, et al. A labor dystocia occurred secondary to uterine torsion [15].
- Asghar, et al. reported a case of 37 weeks twin pregnancy where the c section was scheduled due to twin pregnancy and a difficult obstetrical history. They found 180 degrees rotation of the uterus [16].
Most of the reported cases concern singleton pregnancies. Klicci, et al. reported a case of uterine torsion of 720 degrees in a third trimester 37 weeks pregnancy accompanied by a bladder torsion. Detorsion could not be performed and hysterotomy was performed via a transverse uterine incision. The operation was complicated by uterine atony and B lynch compression sutures were done. The patient was discharged home with her baby at day three postop [17]. Another case of 180 degrees uterine torsion happened in a preterm 30 weeks pregnancy. The patient was asymptomatic and presented in labor. The myoma was obstructing the birth canal. A laparotomy was performed with a good prognosis for the mother and the fetus [18].
Our case is one of the rare reported cases where uterine torsion happened in twin pregnancy. The delay for the management affected the prognosis of this pregnancy and increased the risk of fetal mortality. In fact, the immediate surgical management is the major factor that reduces the fetal and maternal mortality [5].
Because of the high life-threatening risk and emergent condition of our patient , neither the ultrasound nor the MRI could be used as complementary tests for diagnosis and the ultrasound was simply and rapidly used only to detect if intrauterine fetal death occurred or not.
Intraoperatively, the uterine detorsion could not be performed but this condition happened in most of the reported cases [19-21].
Uterine torsion is a very rare entity. The risk of maternal and fetal mortality is high. However, the prognosis is improved as long as the management is done rapidly. More data is needed in order to know about the genetic predilection and the characteristics of imaging workup for a rapid preoperative diagnosis of this condition.
We thank Dr. Luc Rigonnot, the head of the department of obstetrics and gynecology at Centre Hospitalier du Sud Francilien for his continuous support and valuable supervision.
Informed consent
Due to the fact that this case is a life-threatening emergency with inadequate time to obtain consent from the patient itself, written consent was obtained from the patient’s family in order to publish this case report.
Author contributions
Darido J and Grevoul Fesquet J wrote the initial draft. Diari J, El Haddad C, Bouzid N, Abou El Hassan N, Khadam L, and Rigonnot L wrote the second draft. All authors contributed to the collection of data regarding this case report and agreed on the final version of it.
Data availability
Centre Hospitalier du Sud Francilien, Iles de France, France
- Piot D, Gluck M, Oxorn H. Torsion of the gravid uterus. Can med Assoc J. 1973; 109: 1010-1011. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/4758858
- Jensen JG. Uterine torsion in pregnancy, Acta obstet gynecol Scand. 1992; 71: 260-265. PubMed: https://pubmed.ncbi.nlm.nih.gov/1322618/
- Patel ML, Sachan P, Arora A. Complete axial torsion of pregnant uterus with leiomyoma. BMJ case rep. 2014; 2014: bcr2014205558. PubMed: https://pubmed.ncbi.nlm.nih.gov/25193815
- Cook KE, Jenkins SM. Pathologic uterine torsion associated with placental abruption, maternal shock and intrauterine fetal demise. AmJ Obstet Gynecol. 2005; 192: 2082-2083. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/15970905
- Guie P, Adjobi R, N'guessan E, Anongba S, Kouakou F, et al. Uterine torsion with maternal death: our experience and literature review. Clini Exp Obstet Gynecol. 2005; 32: 245-246. PubMed: https://pubmed.ncbi.nlm.nih.gov/16440824
- Jensen JG. Uterine torsion in pregnancy. Acta Obstet Gynecol Scand. 1992; 71: 260-265. PubMed: https://pubmed.ncbi.nlm.nih.gov/1322618/
- Wilson D, Mahalingham A, Ross S. Third trimester uterine torsion: Case report. J Obstet Gynecol. 2006; 28: 531-535. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/16857121
- Zullino S, Faiola S, Paganelli AM, Ferrazzi E. A case of abruption placentae due to the torsion of gravid uterus. Cas Rep Obstet Gynecol. 2014; 2014: 801616. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/25544919
- Chua KJ, Patel R, Eana A, Varughese J. Uterine torsion with necrosis of bilateral adnexa in a postmenopausal woman. BMJ Case Rep. 2019; 12: e229311. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/31217212
- Kopko J, Stańczak R, Warzecha D, Wielgos M. Uterine torsion in the second trimester of pregnancy. Neuro Endocrinol Let 2018; 39: PubMed: https://www.ncbi.nlm.nih.gov/pubmed/30796791
- Moores KL Wood MG, Foon RP. A rare obstetric emergency: acute uterine torsion in a 32 week pregnancy. BM Case Report. 2014; 2014: BCR2013202974. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/24728893
- Thubert. Journal de gynecology obstetrique et biologie de la reproduction. 2011; 40: 371-374.
- Cook KE, Jenkins SM. Pathologic uterine torsion associated with placental abruption maternal shock and intrauterine fetal demise. Am J Ostet Gynecol. 2005; 192: 2082-2083. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/15970905
- Demaria F, Goffinet F, Jouannic JM, Cabrol D. Preterm torsion of a gravid uterus didelphys horn of a twin pregnancy. Obstet Gynecol. 2005; 106: 1186-1187. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/16260565
- Joseph RF, Irvine LM, Sanusi A. Labour dystocia secondary to uterine torsion in twin pregnancy. J Obstet Gynaecol. 2008; 28: 649-649.
- Asghar. Uterine torsion in twin pregnancy. Professional Med JQ. 2006; 13: 327-329.
- Klicci C, Sanverdi I, Bostanci E, Abide CY, Eser SK. Uterine torsion of 720 degrees in third trimester of pregnancy and accompanying bladder torsion: a case report. Pan Afr Med J. 2018; 29: 175. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/30050639
- Zieger W, Hampl M, Leveringhaus A, Wischnik A. Torsion of the pregnant uterus. Geburtshilfe Frauenheilkd. 1995; 55: 404-406. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/7557208
- Ulu I, Güneş MS, Kiran G, Gülşen MS. A rare cause of placental abruption: uterine torsion. J Clin Diagn Res. 2016; 10: QD06-QD07. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4740659/
- Farhadifar F, Nikkhoo B, Shahgheibi S, Soofizadeh N, Rezaie M. Asymptomatic uterine torsion in a pregnant woman. Indian J Surg. 2014; 76: 321-322. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4175681/
- Fatih FF, Gowri V, Rao K. Uterine torsion in second trimester of pregnancy followed by a successful term pregnancy. BMJ Case Report. 2012; bcr2012006359. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/22914233