More Information
Submitted: 13 June 2020 | Approved: 22 June 2020 | Published: 24 June 2020
How to cite this article: Darido J, El Haddad C, Diari J, Grevoul Fesquet J, Bouzid N, et al. COVID-19 in pregnancy: Our experience at a tertiary maternity unit in France. Clin J Obstet Gynecol. 2020; 3: 054-064.
DOI: 10.29328/journal.cjog.1001051
Copyright License: © 2020 Darido J, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: COVID-19; SARS-COV-2; Coronavirus; Infection; Pregnancy; Masks; Maternal complications; Obstetric complications; Review; Fetus; Intrauterine transmission; Route of delivery; Comorbidities
COVID-19 in pregnancy: Our experience at a tertiary maternity unit in France
Darido Jessie1,2*, El Haddad Cynthia1, Diari Jed1, Grevoul Fesquet Julie1, Bouzid Nassima1, Bobric Andrea1, Lakhdara Nefissa1, Bazzi Zeinab2, Lebis Cindy1 Khadam Louay1 and Rigonnot Luc1
1Department of Obstetrics and Gynecology, Centre Hospitalier Sud Francilien (CHSF), Ile de France, France
2Department of Obstetrics and Gynecology, The Lebanese University, Beirut, Lebanon
*Address for Correspondence: Darido Jessie, Department of Obstetrics and Gynecology, Centre Hospitalier Sud Francilien, Ile de France, France & Department of obstetrics and gynecology, Faculty of medical sciences, The Lebanese University, Beirut, Lebanon, Tel: 0033754441180; Email: [email protected]
Objectives: Our main objectives are to reveal the pregnancy and neonatal impacts of COVID-19 infection and to compare it to the results that are reported in the literature.
Methods and materials: The characteristics of the admitted pregnant patients COVID-19 positive with their initial presentation, course at the hospital, and short term follow-up are exposed. Correlation of the age and gestational age with the severity of the disease was calculated.
Results: Thirty five COVID-19 positive pregnant patients presented between the beginning of March and the end of April 2020. From 5 weeks till 41 weeks of gestation, all trimesters were included. The mean of age is 32 and the BMI equal 28.2. Associated comorbidities included not only diabetes and hypertension but also PCOS. The symptomatology was considered mild in most of the cases. The distribution of the symptoms included cough in 86%. 10 out of 35 delivered and cesarean was performed in 50% of the cases. The mean length of stay is 6 days. Neither maternal nor neonatal deaths occurred. There is a significant correlation between the age of the patient and the severity of the disease but this is not the case with gestational age.
Conclusion: Our results were comparable to the literature in terms of initial presentation, associated comorbidities and the length of stay. Despite the fact that the cesarean rate was high, it was far below that of the literature. More data is still needed about COVID-19 in pregnancy.
The new Beta coronavirus, the SARS-COV2, Known as COVID-19, this new version of coronaviruses was highly infectious, particularly during the asymptomatic period of incubation, with a low rate of consequent mortality. Therefore, it kept spreading, became pandemic and resulted in a worldwide health crisis of rapid evolution with consequent socioeconomic effect due to international strict measurements of lockdowns and border closures [1-3].
Officially, the first confirmed case in France was reported on the 24th of January 2020 and the first death on the 14th of February. However, the retroactive testing of samples revealed that one of the reported COVID-19 positive patients seemed to be infected with the virus since December 2019 [5]. The obligatory lockdown was officially declared by the French President Emmanuel Macron on the 16th of March 2020. Up until the latter date, the total number of infected cases was 6,633 and the additional infected patients within 24-hours were 1097 at the level of the whole territory. France was classified the seventh between 163 affected countries attacked by COVID-19. At the end of April, after 45 days of home confinement, the COVID-19 statistics in France turned back with a total of 129,581 infected patients (Source: Statista database).
The pregnant women are affected by this virus. The impacts of COVID-19 on this category of patients and their fetuses at the different stages of pregnancy are subjected to multiple discussions. Questions are also raised concerning the long term effects on the patients and the vertical transmission to newborns. Its impact on pregnancy cannot be negligible especially if the maternal and fetal complications due to other types of coronaviruses in previous epidemics are taken into consideration [6]. It is evident that the sociodemographic characteristics and presumed predisposing risk factors are of high importance.
The subject of COVID-19 in pregnancy is a matter of two major points:
- At first, the pregnancy itself. It is a state of vulnerability due to the correlated physiological and mechanical changes not only at the level of the cardiopulmonary and immune system but also the hypercoagulable state.
- Secondly, the obstetricians and health agencies that receive the case because their level of competence counts for the management outcomes.
All the active members of the medical, obstetrical and public health fields are constantly engaged in the periodic monitoring of the risks on pregnant women, the organization of training resources in addition to the elaboration of new recommendations and reports in order to get day after day a better performance facing COVID-19. Lots of studies and researches were done worldwide in order to understand this virus, and to help the public health systems of all affected countries in the instauration of the accurate prevention and treatment protocols for the patients that are hospitalized depending on the severity of this disease. Despite the large number of articles that were recently published, the data concerning the impact of COVID-19 on pregnancy, particularly in its first and second trimester, is still limited.
We hereby report the experience of the department of obstetrics and gynecology at a tertiary maternity unit in a public hospital in France, the Centre Hospitalier Sud Francilien (CHSF), where a COVID unit was opened for the hospitalized pregnant women who presented at the hospital with a suspicion of COVID-19 infection. We expose the characteristics of the hospitalized pregnant patients PCR positive, their initial presentation, their course at the hospital, their short term follow-up. The Chest CT scanner results were reported if done. In addition, we will be revealing the COVID protocol that was developed at our department and its outcomes at the level of the hospitalized studied patients.
Our main objectives are to reveal the pregnancy and neonatal impacts of COVID-19 infection and to compare it to the results that are reported in the literature. The secondary objectives consist to point at the clinical presentation of COVID-19 in our pregnant patients and the degree of its severity, to evaluate the associated comorbidities and to provide the department protocol that leaded to an overall very acceptable outcome of management.
The tertiary maternity unit of the CHSF has about 5300 delivery per year. It is one of the most dynamic maternities of Ile de France, France. During this crisis, measurements were taken in order to manage the cases of pregnant women infected with COVID-19 independently from those who are not infected.
Pregnant patients that presented to the Emergency Room (ER) of obstetrics and genecology were divided into three major groups:
- Possible cases: clinical respiratory signs and/or fever: Pneumonia, Acute Respiratory Distress Syndrome and/or sudden anosmia without any nasal obstruction
- Probable cases: clinical signs in the last fourteen days following a close contact with a confirmed case
- Confirmed cases: sampling is positive either the patient is symptomatic or not
Note that “close contact” is considered to be the situation of one of two:
A person who, 24 hours before apparition of the symptoms of a confirmed case, have shared the same place (for example: family in the same room) or have had a direct contact with him: face to face about less than 1 meter and/or during more than 15 minutes discussion, flirt, close friends in the class or in a workplace or in a common transport of long duration, etc.
A worker who is taking care of a confirmed case or manipulating the correspondent biologic sampling in the absence of adequate protection.
The management of suspected or confirmed pregnant patients is controlled by the precaution measurements of droplets and contact isolation. Note that the limited availability of the materials of protection (e.g. masks) imposed restrictive measurements on their usage. The surgical masks were systematically available for the healthcare workers, symptomatic, probable and confirmed cases. In fact, they should be wearing it during the whole period of care. Concerning the exposing care (e.g. vaginal delivery, cesarean, head and neck sampling), measurements are as follow:
- A respiratory protection device (FFP2 mask) for every health care worker. A face fit test has to be performed before the entry into the patient’s room
- A disposable single-use isolation gowns with long sleeves doubled by a plastic apron. Whereas the reinforced sterile gowns are reserved for deliveries (normal or cesareans)
- Non sterile gloves
- Full face and neck shield mask for sampling or delivery
- Covering cap for complete protection of the hair
- Rigorous hand hygiene with hydroalcoholic gel
As for the non-exposing care (e.g. blood sampling, fetal heart rate monitoring), measurements are as follow:
- Hand hygiene with hydroalcoholic gel
- Surgical masks
- Non sterile gloves
Upon presentation to the obstetrical ER, suspected or possible cases have to wear the surgical mask. Then they enter one of the boxes that have been reserved and prepared for such COVID obstetrical emergencies. As for the healthcare workers who are taking in charge this patient, they wear in accordance with the CHSF vigorous procedures of droplets and contact isolation as mentioned above.
- After ruling out all the etiologies of fever during pregnancy, we proceeded with the following:
- Anamnesis: Past history, infectious contact, beginning of symptoms (fever, cough, anosmia, digestive problems)
- Vitals: Blood Pressure, pulse, oximetry, respiratory frequency, urinary dipstick
- Physical exam: pulmonary auscultation is included
- Obstetrical exam depending on the gestational age: fundal height, cervical exam +/- speculum and amnicator tests
- Fetal heart rate depending on the gestational age: cardiotocography machine with a distance of more than one meter from the patient who should not touch it
- Systematic Obstetrical ultrasound before admission : biometry, Doppler, amniotic fluid index
- Routine Biological tests performed in case of fever: CBCD, CRP, vaginal culture, Urine dculture
- If the patient needs to be admitted, we extend the laboratory tests to: hemostasis, electrolytes, urea, creatinine, liver function tests (LFTs), irregular agglutinin, blood group, haptoglobin, D-dimers, Creatine Phosphokinase, N-terminal proB-type Natriuretic Peptide, troponins, Procalcitonin, blood culture if fever ≥ 38.5 degrees (rule out listeriosis), rapid urinary antigen test (legionella, pneumococcus), Serologies (rubella, toxoplasma, HIV, syphilis and HbS antigen), hemoglobin electrophoresis depending on the patient’s origin
- Nasopharyngeal and oropharyngeal swabs for COVID-19 sampling. PCR tubes tightly closed, put in a plastic bag then in a 95 kPa bag sent to the labs
- The thoracic imaging is not done systematically
If the patient is discharged home, there are no indications for a prophylactic dose of Low Molecular Weight Heparin (LMWH), except if there is an additional risk factor.
As for the management of possible cases with a maternal or fetal life-threatening condition, the patient should be considered as infected until the sampling results prove otherwise. In this case, if the ultrasound is necessary for evaluation, the probe should be protected before usage and after that and the machine should be disinfected according to the institutional procedures. If the reanimation trolley is needed, it should also be disinfected. Patient’s personal belongings are put in a bag tightly closed and labeled with her name. In an obstetrical emergency, the patient is directly transferred to the delivery suite.
In case of a suspected or confirmed patient with no life-threatening emergency, we have three major situations:
- If needed oxygen is ≤ 3l/min: hospitalization in the COVID unit
- If needed oxygen is > 3l/min: multidisciplinary decision (obstetricians, anesthesia, pneumologists, pediatrician) for the case management and hospitalization (ICU or COVID unit)
- If there are no criteria for hospitalization, we proceed into an ambulatory surveillance. The directives are given. Next morning, the patients are called by a midwife who is officially responsible of transmitting their PCR results and verifying their inscription for follow up on ECOVID application.
- Pregnant patients who are hospitalized at the COVID unit, either confirmed or suspected cases, are considered as high risk pregnancies and the measurements that were taken towards them are as follow:
- General measurements
o Droplets and contact precautions
o Limitation of the number of contacts: one Midwife and one senior visit
o The hygiene measurements
o Surgical mask for the patient and the healthcare workers. FFP2 masks are used for a nursing care at less than one meter distance from the patient.
- Criteria of oxygen needs
o If saturation ≥ 95%, no need for oxygen
o Patient with increased respiratory rate and saturation ≥ 95%: vigilance because of the secondary desaturation risk. In this case it is possible to supplement the patient with an oxygenation of comfort.
o Sat < 95% is an indication for oxygen therapy
- Mode of administration: nasal oxygen with a surgical mask over it. We start with 2 liters/min. and the rate of oxygen is adapted progressively in order to obtain a saturation ≥ 95%. Oxygen can be increased up to 5 liters/min so the surgical mask can be maintained for the patient. After oxygen administration, a reevaluation of the patient’s state is performed after one hour and a transition to 3 liters/min is done if there was no improvement.
- Vital signs are taken every 4 hours (pulse, blood pressure, oxygen saturation, respiratory rate)
- In case of maternal aggravation and increased oxygen needs, seniors of obstetrics, anesthesia and pneumology are called and the labs are renewed: CBCD, PCT, D-dimers, electrolytes, renal panel and liver function tests
- The fetal heart rate is monitored once daily, to be renewed if fever > 39 degrees or saturation < 95%
- Antibiotherapy based on Amoxicillin 1G 3 times per day if there is associated fever waiting for the results to be out. It will be maintained depending on the case. If the patient is allergic to amoxicillin, Clindamycin is prescribed. In case of acute respiratory syndrome with superimposed pulmonary infection (purulent sputum) or PCT > 0.25 ng/ml, amoxicillin is stopped. Then, the combination of Cefotaxime (1 g 3 times per day intravenously) during 7 days and Spiramycin (3 MU 3 times per day per os or 1.5 3 times per day IV) is given.
- A cure of steroids for fetal maturation is reserved for high risks of premature deliveries. In case of induced prematurity linked to a respiratory distress syndrome, the balance between advantages and risks of corticotherapy should be evaluated in a multidisciplinary meeting.
- If the patient is on lopinavir/ritonavir, prescribed by pneumologists, it should be continued 400 mg x 2/ day per os for a total duration of 7 days.
- Deep venous thrombosis prevention with TED stockings and LMWH at prophylactic doses 4000 IU:
o One subcutaneous injection per day (to be adapted to the weight of the patient) for 14 days.
o One subcutaneous injection twice per day if D-dimers > 4 000
Over this protocol, modifications were done at the level of antibiotics and anticoagulants as follow:
- If fever, amoxicillin 1g x 3/day the time the results are out and if allergy erythromycin IV 1g x 3/day
- If COVID-19 positive and the oxygen needs are less than 3 liters per minute, no antibiotics are given except if
o Purulent sputum
o PCT > 0.25 ng/ml
o Radiologic imaging (bacterial pneumonia)
o Immunodepression (HIV, drepanocytosis)
o In case of the above exceptions, amoxicillin is stopped:
o If the patient is in her first trimester, amoxicillin/clavulanic acid 1G x 3/day IV and if allergy cefotaxime 1G x 3/day (7 days)
o If the patient is in her second to third trimester, cefotaxime 1G x 3/day (7 days)
- As for the anticoagulation, fibrinogen and D-dimers are tittered:
o DVT prophylaxis is reinforced with LMWH 4000 x 2/day and 6000 x 2/day if the weight > 120 kg. If clearance < 30 ml/min, Calciparin is given 200 IU/kg/24 h. Platelets are controlled two times the first week, then once every week
o However, if fibrinogen > 8 and D-dimers > 3000, the risk of thrombosis is very high. Heparinotherapy at curative dose is given: LMWH 100 IU/kg/12 h. If Clearance < 30 ml/min, Non Fractionated Heparin 500 IU/kg/24 h. Platelets control, PTT, AntiXa four hours after the second injection are taken with a goal of 0.5 and 0.7.
The criteria of discharge are the following:
- Absence of fever
- Improvement of pulmonary signs
- 48 hours of oxygen abstinence
- No aggravation of the underlying comorbidities
Even if discharged, a total of 14 days lockdown at home after the symptoms have started should be respected. Concerning the treatment of discharge, one subcutaneous injection of LMWH 4000 IU per day (to be adapted to the patient’s weight) to be continued for 14 days in total. As for the outpatient surveillance, discharged patients were called at day 3, day 7 and day14 (from the beginning of the symptoms). More surveillance is provided if necessary. The patient is given the hospitalization summary. The obstetrical follow-up is maintained by a scheduled consultation at 3 weeks after the discharge and a growth ultrasound at 3 to 4 weeks then to be renewed depending on the second and third trimester ultrasound. Diagnostic ultrasound and MRI is recommended for the patient who required mechanical ventilation due to severe hypoxia that could have caused fetal hypoxia.
All pregnant women that were admitted to the Obstetrics and gynecology ER of the CHSF, Iles de France, France, hospitalized or not, starting from March 2020 and up till the end of April 2020, with suspected COVID and positive PCR test were registered. The maternal age, gestational age, initial symptoms, PCR results, lab results, hospitalization date, discharge date, route of delivery, follow-up were retrospectively reviewed. For the patients who delivered, neonatal throat swabs were taken and placenta was sent for pathology exam. Note that COVID positive mothers were allowed to breastfeed their newborns. Their precaution measurements included a surgical mask on the face along with hand hygiene. The policy of hospital at this COVID period restricted the presence of partners to the imminent delivery phase only. In other terms, the partners were not allowed to stay during the whole labor period.
The total number of suspected cases that were admitted to the ER of the maternity was 70 pregnant patients. 35 patients (50%) were COVID-19 positive after PCR tests. The overall cases are documented in table 1 where the patients are detailed case by case.
| Table 1: Characteristics of the pregnant COVID positive patients of our serie. | ||||||||||||
| P | Age | G A | PMH/ PSH Comorbidities |
BMI | Gr | Symptoms | O2 Liters/min | Labs | CT scan | LoS (days) |
Delivery | Follow up |
| 1 | 20 | 37+3 | None | 34 | O+ | Cough, asthenia | 2 | ↑ CRP | GGO | 11 | NVD at 37+6 | Good GS |
| 2 | 43 | 28+4 IVF | Hypothyroidism | 22 | A- | Fever, Cough | 2 | Thrombocytosis | NP | 8 | Ongoing Pregnancy | PersistentDyspnea |
| 3 | 35 | 31 | Gestational Diabetes | 44 | A+ | Fever, cough Dyspnea, anosmia Dysgeusia |
3 | Ddimers>4000 | NP | 5 AMA |
NVD at term | Mild cough |
| 4 | 40 | 17 | Chronic hepatitis B | 32 | M | Fever, cough Dyspnea,asthenia | 2 | ↑ CRP | NP | 6 | Ongoing Pregnancy | Good GS |
| 5 | 29 | 20 | Gestational Diabetes | 26 | A+ | Cough, dyspnea asthenia, anosmia Dysgeusia | NN | Normal | NP | NH | Ongoing Pregnancy | Day 3 & 7 Same symptoms Day 14 only fatigue |
| 6 | 34 | 5 | Chronic hepatitis B | 21 | AB+ | Anosmia | NN | NP | NP | NH | Spont. abortion at 8 weeks | Good GS |
| 7 | 34 | 14 | HTN, Migraine Ovarian cysts |
35 | O+ | Fever, cough Asthenia, Myalgias Anosmia, Dysgeusia |
NN | ↑ LFTs ↑CRP HypoK |
NP | 3 | Ongoing Pregnancy | Good GS |
| 8 | 21 | 32 | Benign pinealocytoma PCOS |
21 | O+ | Cough,Asthenia Anosmia | NN | NP | NP | 3 | Ongoing Pregnancy | Good GS |
| 9 | 31 | 30 | None | M | O+ | Cough , dyspnea Anosmia, diarrhea | NN | NP | NP | NH | Ongoing Pregnancy | Cough |
| 10 | 36 | 32 | Current preg. Preeclampsia Twins bi bi |
29 | O+ | Fever. Cough Myalgias, Headache | NN | ↑CRP D dimmers>3000 PCT>0.25 |
NP | 6 | Induction labor NVD Twin 1Ceph AS 10/10/10 pH 7.31 L 2.8 Twin 2 breech AS 5/7/9/10 pH 7.28 L2.8 NRFHR |
Good GS |
| 11 | 44 | 37 | Ovarian cyst One cesarean Gestational diabetes |
25 | A+ | Fever, Cough Anosmia,Dysgeusia | 2 | ↑ CRP | NP | 8 | Cesarean in labor, NRFHR at 40+6 pH 7.08 L 8.8 AS 7/7/9/9 |
Persistent cough anosmia, Dysgeusia |
| 12 | 25 | 31 | None | M | A+ | Fever, cough, dyspnea, asthenia headache | NN | ↑ CRP HypoK |
NP | 6 | Ongoing Pregnancy | Transitory Fetal tachycardia |
| 13 | 37 | Del. | None | 23.5 | O+ | Fever cough Day 3 PP |
NN | NP | NP | 3 | SROM OVD (vacuum) NRFHR Neonatal hyperthermia | Good GS |
| 14 | 27 | 25 | None | 25 | M | Cough, Anosmia | NN | NP | NP | NH | Ongoing Pregnancy | Anosmia Dysgeusia |
| 15 | 37 | 30 | 3 cesareans Current Preg IUD, ICP |
25 | B+ | Fever, cough, Asthenia, anosmia diarrhea | 2 | ↑ LFTs Bile acids 16 |
NP | 6 | Ongoing Pregnancy | Same as admission |
| 16 | 36 | 20 | Umbilical hernia | 29 | B+ | Fever, cough Dysgeusia, dyspnea | NN | ↑CRP | NP | 4 | Ongoing Pregnancy | M |
| 17 | 36 | 29 | Type 2 diabetes One cesarean |
36 | AB+ | Cough dyspnea | 3 | Normal | NP | 12 | Ongoing Pregnancy | Same as admission |
| 18 | 19 | 34 | None | -- | M | Asthenia headache cough dyspnea | NN | Normal | NP | NH | Ongoing Pregnancy | Fatigue anosmia Dysgeusia |
| 19 | 26 | 34 | Operated Aortic coarctation | 23 | AB+ | Asthenia myalgias fever cough dyspnea | 2 | Lymphopenia | NP | NH | Ongoing Pregnancy | Good GS |
| 20 | 29 | 32 | One cesarean Gestational diabetes, HTN |
39 | A+ | fever cough Myalgias headache |
NN | NP | NP | NH | Ongoing Pregnancy | Cough anosmia Dysgeusia |
| 21 | 39 | 27 | 4 cesareans MS |
-- | O+ | cough dyspnea Myalgias, headache | NN | Thrombopenia | NP | NH | Ongoing Pregnancy | AstheniaMyalgias headache |
| 22 | 27 | 26 | Gestational HTN | 34 | O+ | Headache rhinitis | NN | NP | NP | NH | Ongoing Pregnancy | Good GS |
| 23 | 27 | 12 | Hyperemesis gravidarum | -- | M | Decreased weight of 13kg | NN | HypoK, HypoNa ↑LFTs |
NP | NH | Ongoing Pregnancy | M |
| 24 | 30 | 41 | Breast cysts | 25 | A+ | Fever cough | NN | NP | NP | 5 | IOL NVD Shoulder dystocia(4.4kg) pH 7.19 L 5.4 |
Cough |
| 25 | 27 | 24 | Lupus, Basedow Two cesareans Pancreatitis Cholecysytectomy |
28 | B+ | Cough asthenia thoracic pain | NN | Normal | NP | NH | Ongoing Pregnancy | Cough |
| 26 | 30 | 34 | Two cesareans | 28 | B+ | Headache Cough Tinnitus |
NN | HypoNa ↑CRP |
NP | 2 | Scheduled cesarean | Cough |
| 27 | 29 | 30 | Gestational Diabetes | 21 | O+ | Cough asthenia dyspnea | NN | ↑CRP | NP | 12 | Scheduled cesarean | Good GS |
| 28 | 42 | 27 | One cesarean Rhinitis |
31 | AB - | Asthenia cough dyspnea | 3 then 12 | ↑LFTs | GGO | ICU 45 |
Cesarean at 27 + 3, GAn, GS alteration AS 6/10/10 pH 7.27 L 2.7 intubated in NICU but stable |
Good GS |
| 29 | 35 | 24 | Chronic HTN Two cesareans Cholecystectomy |
24 | B+ | Asthenia Myalgias headache cough dyspnea fever | 2 | Hypok ↑CRP |
GGO | 11 | Ongoing Pregnancy | Fever cough thoracic pain |
| 30 | 32 | 30 | Appendectomy | 35 | O+ | Anosmia fever cough dyspnea | 2 | ↑CRP ↑LFTs |
NP | 15 | Ongoing Pregnancy | Cough |
| 31 | 23 | 32 | None | 23 | O+ | Asthenia cough | NN | ↑CRP | NP | 9 | Ongoing Pregnancy | Good GS |
| 32 | 39 | 18 | Asthma, Diabetes | 34 | O- | Myalgia fever cough | NN | Normal | NP | 8 | Ongoing Pregnancy | M |
| 33 | 21 | 30 | childhood Asthma | 25 | A+ | Dyspnea | NN | Lymphopenia ↑CRP |
NP | NH | Ongoing Pregnancy | M |
| 34 | 34 | 24 | Migraine Breast fibromas Gastritis |
23 | O+ | Cough dyspnea asthenia headache | 3 | ↑WBC | NP | 10 | Ongoing Pregnancy | Cough |
| 35 | 36 | 39 | Current preg Toxoplasmosis infection |
24 | B+ | Asthenia fever | 2 | PCT > 0.25 Thrombopenia ↑CRP |
NP | 10 | cesarean NRFHR |
Fever |
| P: Patient; GA: Gestational Age; GR = Blood Group; CRP: C Reactive Protein; GGO: Ground Glass Opacities; GS: General State; IVF: In Vitro Fertilization; NP: Not Performed; AMA: Against Medical Advice; NVD: Normal Vaginal Delivery; UK: Unknown; NN: Not Needed; HTN: Hypertension; LFT: Liver Function Test; Hypok: Hypokalemia; Hypona: Hyponatremia; NP: Not Performed; Spont: Spontaneous; M: Missed; Bi: Bichorionic Biamniotic; PCT: Procalcitonin; AS: Apgar Score; NRFHR: Non Reassuring Fetal Heart Rate; L: Lactate Gan; General Anesthesia; Preg: Pregnancy; NICU: Neonatal Intensive Care Unit; ICU: Intensive Care Unit; PP: Postpartum | ||||||||||||
In this serie, we are covering the three trimesters of pregnancy from 5 weeks of gestation till 41 weeks and the repartition is as follow: first trimester (n = 2), second trimester (n = 10) and third trimester (n = 22) in addition to only one case where the infection was diagnosed at day 3 postpartum. In other terms, 24 out of 34 pregnant patients are at a viable stage of pregnancy and 10 out of 34 are in their early stage. The mean of age, gestational age and BMI with the minimum and maximum values are exposed in table 2. A mean of BMI about 28 indicates an overall weight status of overweight reaching morbid obesity with a maximum of 44.
| Table 2: Mean of age, gestational age and BMI with the minimum and maximum value of each. | |
| Mean ± SD [min; max] |
|
| Age | 31.7 ± 6.7 [19 - 44] |
| Gestational age (weeks) |
28 ± 1 [5 - 41] |
| BMI (Kg/m2) |
28.2 ± 5.9 [21 - 44] |
| SD: Standard Deviation; BMI: Body Mass Index | |
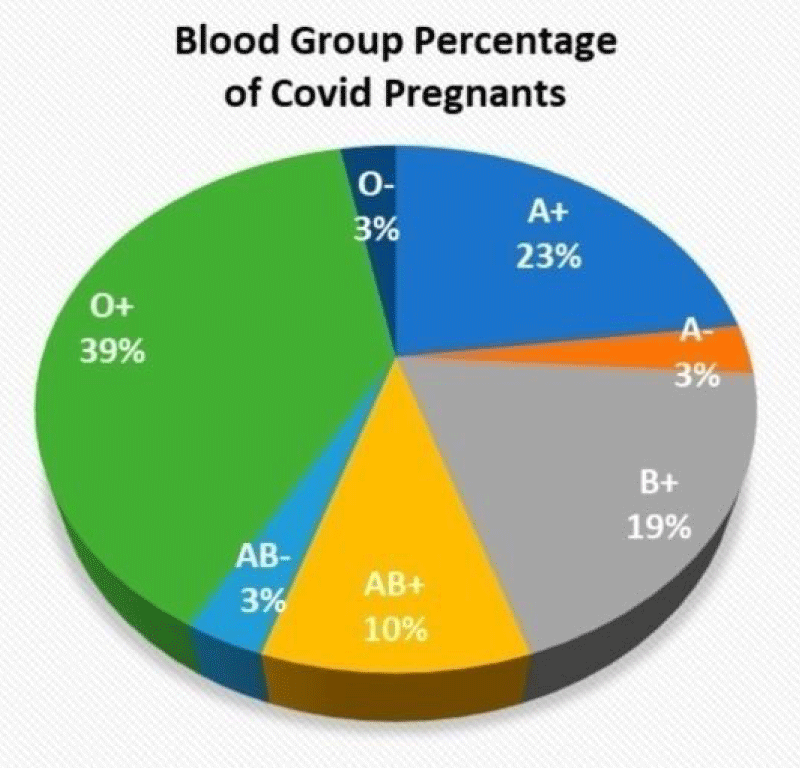
Near one third of the patients is O positive. The distribution of other blood groups is exposed in table 3 and figure 1. It seems that its correlations with the supplemental Oxygen and length of stay are significant (OR = 0.39870 p = 0.0263 and OR = 0.33106 p = 0.0689 respectively)
| Table 3: Repartition of patients by their blood group. | ||||||||
| BG | O | A | B | AB | ||||
| Rh | + | - | + | - | + | - | + | - |
| N | 12 | 1 | 7 | 1 | 6 | 0 | 3 | 1 |
Figure 1: Distribution of the blood groups by percentages over our patients.
As for the associated medical comorbidities, over our pregnant COVID positive patients, diabetes in its gestational or type 2 form was the most prevalent with 7 patients out of 35 with consists 20% of the studied cases. Secondly, we have the hypertension (chronic/gestational ± preeclampsia) with 4 cases out of 35 (11.4%). The other comorbidities are listed in table 4. If we do not take into consideration the previous surgical history of appendectomy, umbilical hernia repair, and cesareans we note that 10 patients are strictly healthy without any associated medical health issues either prior to conception or during pregnancy, about 28.5% of the patients. In other terms, most of our cases (71.5%) have an associated medical condition.
| Table 4: Associated underlying medical and pertinent surgical conditions. | |
| n | |
| Diabetes type 2/gestational | 7 |
| HTN /preeclampasia | 5 |
| Migraine | 2 |
| URT condition | |
| Asthma | 2 |
| Rhinitis | 1 |
| Infections | |
| Chronic Hepatatis B | 2 |
| Toxoplasmosis recent infection | 1 |
| Pancreatitis | 1 |
| Thyroid problems | |
| Hypothyroidism | 1 |
| Hyperthyroidism (BAsedow) | 1 |
| Autoimmune diseases | |
| Multiple sclerosis | 1 |
| Lupus | 1 |
| Gynecologic conditions | |
| PCOS/ ovarian cysts | 3 |
| Breast benign path (cysts/ fibromas) | 2 |
| Preg related pathology | |
| ICP | 1 |
| HG | 1 |
| Previous Sx | |
| benign pinealocytoma | 1 |
| Aortic coractation | 1 |
| ICP: Intrahepatic Cholestatsis; HG: Hyperemesis Gravidarum; Sx: Surgeries; URT: Upper Respiratory Tract | |
The spectrum of the symptoms of the patients is divided into three major groups:
- Mild with no pneumonia signs and no alteration of the labs
- Severe with dyspnea, need of supplemental oxygen, infiltrates on CT scan or respiratory rate of more than 30
- Critical with intensive care unit admission
If we consider the Oxygen need as a major criteria to characterize the severity of the disease, the COVID 19 infection in our patients was in the majority of the cases mild with no need of oxygen in 62.8% of the cases (n = 22/35). However, 12 patients required 2 to 3 liters of oxygen per minute. And one patient have had a major alteration of her respiratory condition requiring emergent delivery and transfer to the intensive care unit with 12 liters supplementation of Oxygen.
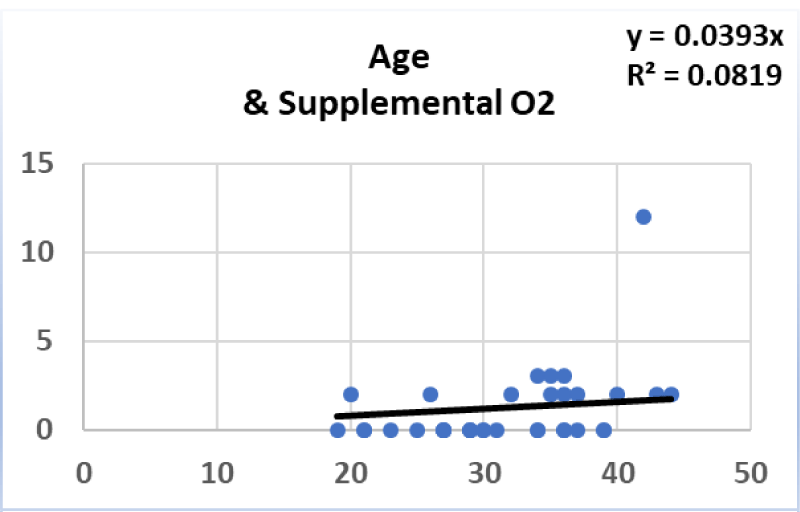
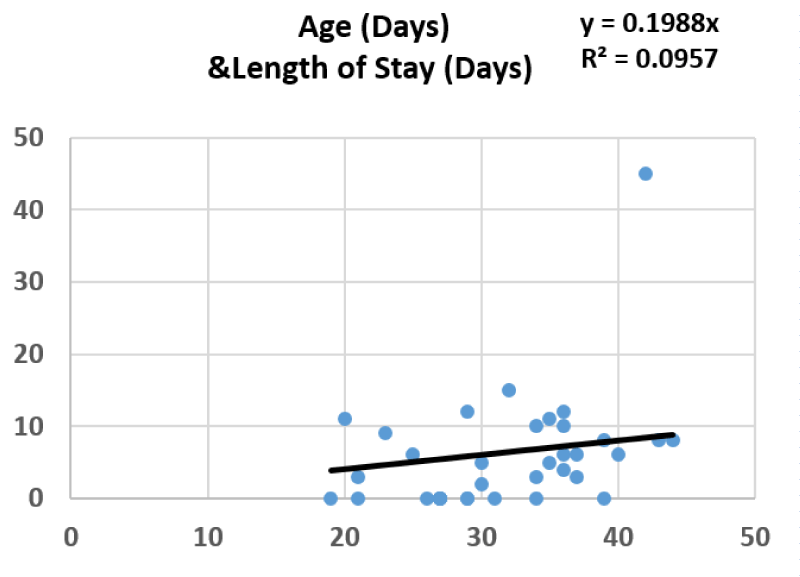
More than half of the patients were hospitalized whereas 12 out of 35 were not. The length of stay was a mean of 6 days (5.9 ± 8.1), with a maximum of 45 days for the ICU case. The statistical measurement of correlations between the age (OR = 0.41676 p = 0.0128 and OR = 0.38068 p = 0.0241, respectively). However, the correlations between the gestational age of the patient and the supplemental oxygen as well as the length of stay were not (OR = 0.09554 p = 0.5909 and OR 0.13561 p = 0.4444, respectively) (Figures 2,3).
Figure 2: Despite the considered correlation, age cannot be predicting the required quantity of oxygen.
Figure 3: Despite the considered correlation, age cannot be predicting the required length of stay.
Upon presentation, the majority of the patients have a symptomatology including cough. Near half of them presented with fever followed by asthenia and dyspnea at equal repartition. On the other hand, the neurologic symptoms cannot be underestimated. In fact, Anosmia reached 30% of the symptoms and we had 26% and 14% for the headache and the Dysgeusia, respectively. All presentation symptoms are listed in table 5.
| Table 5: Repartition of the initial symptoms at presentation of COVID-19 positive pregnant patients | |
| Symptoms | N (%) |
| Fever | 17 (49%) |
| Cough | 30 (86%) |
| Asthenia | 16 (46%) |
| Dyspnea | 16 (46%) |
| Diarrhea | 2 (6%) |
| Myalgias | 7 (20%) |
| Anosmia | 10 (29%) |
| Dysgeusia | 5 (14%) |
| Headache | 9 (26%) |
| ↓weight | 1 (3%) |
| Tinnitus | 1 (3%) |
| Rhinorrhea | 1 (3%) |
| Thoracic pain | 1 (3%) |
8 patients have not had lab tests and the laboratory findings were strictly normal in 5 cases only. Only one case had an elevated WBC. The other ones were with normal WBC. (hypothesis: physiologic tendency in pregnancy to increase white blood counts while the virus tends to decrease it?). All lab results are in table 6. The CT scan was performed in three cases and in all of them, the results returned with bilateral ground glass opacities bilaterally.
| Table 6: laboratory findings list. | |
| LABS | n (%) |
| Lymphopenia | 2 |
| Elevated CRP | 14 |
| Elevated LFTS | 5 |
| Thrombocytopenia | 2 |
| Thrombocytosis | 1 |
| Elevated d dimmers | 2 |
| PCT | 2 |
| Hypokalemia | 4 |
| Hyponatremia | 2 |
Ten of the pregnant patients delivered: 5 vaginal deliveries including a twin pregnancy and five cesareans (4 with obstetrical indications distributed with equal percentages for previous cesarean history and Non Reassuring Fetal Heart Rate (NRFHR) and one due to maternal respiratory deterioration) (Table 7).
| Table 7: Pregnancy outcomes in COVID positive pregnant patients. | |
| Pregnancy outcome | n (%) |
| Ongoing pregnancy | 24 |
| C sections | 5 (50%) |
| Vaginal deliveries | 5 (50%) |
| Spontaneous abortion | 1 |
| Maternal Mortality | Zero |
In our serie, there was no maternal mortality.
As for the neonatal status upon delivery, in the majority of the case there was no respiratory distress and APGAR score was 10 at one minute post delivery in 70% of the cases. Three cases of one minute APGAR ranging between 5 and 7 then reestablished between 9 and 10 at 5 minutes. There were only one case NICU admission and one case of neonatal hyperthermia. Note that all neonates returned negative for COVID. Two deliveries were preterm (less than 37 weeks).
The protocol of COVID-19 positive pregnant women management allowed us to have no healthcare workers positive for COVID in the department.
On the Medline database searching website pubmed, up until the twenty second of May 2020 there are about 15,496 results on the subject of COVID-19. By adding the keyword
The pathogenesis of SARS-CoV-2 during pregnancy is still not completely understood [8]. Pregnancy is considered in itself a vulnerable state to viral and respiratory infections mainly caused by the associated immune changes. Severe COVID-19 symptoms are the result of a severe inflammatory state characterized by a storm of cytokines and increased interleukins 2. This will be consequently having maternal and fetal outcomes [9]. The dominance of the T-helper 2 (Th2) over the T-helper 1 in pregnancy protects the fetus relatively against this viral infection but leaves the mother vulnerable [4].
It is well known of the general population through different reports that older age or underlying medical conditions are associated with the severity of the disease [10]. We have had the same among our studied pregnant patient, since the percentage of infected pregnant with at least one risk factor was higher among those who required hospitalization in comparison with those who were not hospitalized. The most common associated comorbidities in our patients were diabetes and hypertension. At another level comes PCOS followed by the multiple cited associated hyper/hypothyroidism, asthma and chronic hepatitis B. In fact, it is well known that generally diabetes in pregnancy increases the susceptibility to infections as it weakens the immune self defense. However, the PCOS is commonly known for early abortion in pregnancies. The presence in our case serie can be explained by the insulin resistance that causes in itself high glucose levels and consequent diabetes. Rare are the reported COVID-19 positive pregnant women series that provide reports on the associated comorbidities. Zaigham, et al. in their metaanalysis performed over 108 pregnancies mentioned the preeclampsia, gestational diabetes and hypothyroidism as associated underlying comorbidities that are present in pregnant COVID-19 positive patients [11].
The clinical symptoms that characterized the presentation of COVID positive pregnant patients are not different from those who are not pregnant [3,12,13]. A summary of 72314 cases from the china center for disease control and prevention reported 147 pregnant patients from which 64 diagnosed cases, 82 suspected cases and one asymptomatic case. Most pregnant women have mild flu like symptomatology [14]. In a reported case serie of 15 pregnant women who tested positive for COVID-19 infection, A CT scan was done before and after the delivery. There were no signs of aggravation at the postpartum period. Authors consequently concluded that pregnancy and delivery do not aggravate COVID-19 infection [15]. There is no clear evidence of severe complications caused by COVID-19 in healthy pregnant patients. A multicentre study in New York State concluded that the pregnant COVID-19 infected women are not at increased risk for admission to the intensive care unit in comparison to the non-pregnant ones [16]. However, it seems that we are dealing with contradictory data. Few other authors considered that the anatomical changes at the level of the lungs during pregnancy make the droplets of COVID-19 more difficult to be removed and easier to be inhaled. By this hypothesis, they have explained the fact that the prognosis after infection is worse in pregnant compared to non-pregnant [17]. It is true the percentage of pregnant COVID-19 positive patients of our serie with mild symptoms is greater than those with severe symptoms but it did not reached the 96% of the metaanalysis that were reported in literature. Also note that the majority of our patients that did not even require oxygen supplementation. On the other hand, the length of stay that is logically correlated with the oxygen supplementation and the severity of the disease was acceptable and equal to the mean of length of hospital stay of 6 days that was reported in the literature [18,19]. In our case serie only one ICU admission is reported.
Reviews are done by Yang, et al., Zaigham, et al. Yan, et al., Kasraeian, et al. and Juan, et al., who reported 114, 108,116, 87 and 324 COVID-19 infected pregnant women respectively from the literature the clinical characteristics and neonatal outcomes are also reported in table 9. Our addition at the level of the initial presentation was the reported anosmia and Dysgeusia [11,13,19-21].
The COVID effects on pregnancy are not very known. Panahi, et al. in their narrative review selected 13 articles where it is reported that COVID-19 can cause miscarriages, preterm delivery, and fetal distress [12]. One case of spontaneous abortion out of two first trimester infected pregnancies in our serie is not sufficient to say that a true correlation exists but most of our patients that did not delivered are having an ongoing pregnancy with a good general state upon follow-up. A retrospective case control study compared 16 pregnant patients COVID-19 positive to 45 pregnant women without COVID-19. The differences between the two groups concerning the fetal distress, preterm birth, intraoperative blood loss, neonatal respiratory distress and birth weight were not significant [22]. One case of a 41 year old pregnant COVID positive lady with previous cesarean deliveries having severe respiratory symptoms upon presentation was reported. She underwent a cesarean delivery. The neonate was immediately isolated after extraction with no delayed cord clamping and no skin to skin maternal neonatal contact. The newborn tested positive for COVID sixteen hours postpartum. It was the earliest of all neonates who tested positive. The authors of this case report raised the possible vertical transmission issue. However, this is not sufficient to confirm the vertical transmission especially that the neonatal SARS- CoV-2 immunoglobulins (Ig) M and G were negative [23]. Other authors deny the vertical transmission risk. In fact, in their studied series amniotic fluid, cord blood and neonatal throat swab tested negative for SARS-CoV-2. [24]. Moreover, reported placental pathological analysis of three COVID-19 positive women who delivered turned back with the absence of morphological changes related to infection: negative nucleic acid of 2019 nCov and no villitis [25].
Till now, there are no clear recommendations concerning the management of COVID-19 infection in pregnant patients. The protocol that is mentioned above and that was applied at our department not only permitted the adequate management of COVID plus pregnant patients but also allowed us to maintain the standards of safety towards the healthcare workers. Furthermore the drugs that were used correspond to the recommendations of drug safety during pregnancy.
There is no clear evidence concerning the delivery route in COVID-19 infected pregnant women. In our department indications where guided by the obstetrical status of the patient and her fetus unless there is a major maternal respiratory distress with alteration of general state of the mother. No reported data concerning the optimal timing of delivery in COVID-19 pregnant women and it is not clear whether the possibly still unproved vertical transmission can be prevented via cesarean section or not [26]. While most of the metaanalysis reached a rate of 69% to 92% of cesarean rate over the delivered infected women [11,20], our serie resulted in 50% of c section rate where a previous cesarean was included in the indications.
One of the largest reviews of literature was done Elshafeey F et al published in April 2020. The drauthors identified a total of 33 articles done in different countries affected by COVID-19. It resulted in 385 pregnant women positive for COVID-19 [27]. In comparison to our study, this study reported 248 singleton and only 4 twins’ pregnancy out of 252 pregnant women. So the pregnant women with twins in our serie is considered to be one of the rare reported COVID-19 twin pregnancies worldwide where the patient have had a normal vaginal delivery of two healthy live babies in a good neonatal status.
Our study is mainly limited by its retrospective nature and the small size of our sample with the fact that some of the reported cases are still having an ongoing pregnancy. Consequently the results concerning the neonatal outcomes cannot be generalized over all our COVID-19 infected pregnant patients. Furthermore, no definitive conclusions can be deduced. However the strength of our study consists mainly of the fact that all the pregnant women turned with positive COVID-19 infection. Consequently all the characteristics and outcomes that were reported are representative of the disease.
All the experts in the medical field, from different countries are meeting and confronting this new virus through a worldwide pandemy. The cost is high; many doctors lost their lives and 6% of them are obstetricians/gynecologists. However more data is still needed especially on large sample size comparing the COVID infected pregnant women to the non-pregnant ones! There is no sufficient data on first and second trimester infection. Questions concerning the newborns and infected mothers temporary separation are still not answered. The answers about the vertical transmission, the congenital anomalies the abortions the morbidity and mortality are clarified step by step in order to build at the end a clear clinical picture about this virus.
Evidences and Information on this recent subject are cumulating and being updated every day. So please note that all information mentioned above are up-to-date until the article is published.
We thank Dr Luc Rigonnot, the head of the department of obstetrics and gynecology at Centre Hospitalier Sud Francilien for his continuous support and valuable supervision.
Informed consent
Informed consent was obtained from all the considered patients in order to publish their cases.
Ethical considerations
This observational retrospective study respected the ethical issues of honesty and integrity of the reported information, of objectivity and carefulness of the data that corresponds to each patient of the serie.
Author contributions
Darido J and El Haddad C wrote the initial draft. Other authors wrote the second draft. All authors agreed on the final version of this article.
Data availability
Centre Hospitalier du Sud Francilien, Iles de France, France
- Li X, Geng M, Peng Y, Meng L, Lu S. Molecular immune pathogenesis and diagnosis of COVID-19. J Pharmaceut Analysis. 2020; 10: 102-108. PubMed: https://pubmed.ncbi.nlm.nih.gov/32282863
- Wang W, Xu Y, Gao R, Lu R, Han K, et al. Detection of SARS-COV-2 in different types of clinical specimens. JAMA. 323: 1843-1844. PubMed: https://pubmed.ncbi.nlm.nih.gov/32159775/
- Rasmusen S, Smulian J, Lednicky J, Wen T, Jamieson D. Coronavirus disease 2019 and pregnancy: what obstetricians need to know. AJOG. 2020; 222: 415-426. PubMed: https://pubmed.ncbi.nlm.nih.gov/32105680/
- Dashraat P, Wong JLJ, Lim MXK, Lim LM, Li S, et al. Coronavirus disease 2019 (COVID 19) pandemic and pregnancy. Am J obstet Gynecol. 2020; 222: 521-531. PubMed: https://pubmed.ncbi.nlm.nih.gov/32217113/
- Deslandes A, Berti V, Tandjaoui-Lambotte Y, Alloui C, Carbonnelle E, et al. SARS-COV2 was already spreading in France in late December 2019. Int J Antimicrob Agents. 2020; 55: 106006. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7196402/
- Masmejan S, Pomar L, Lepigeon K, Favre G, Baud D, et al. COVID-19 et grossesse [COVID-19 and pregnancy]. Rev Med Suisse. 2020; 16: 944-946.
- Di Mascio D, Khalil A, Saccone G, Rizzo G, Buca D, et al. Outcome of coronavirus spectrum infections (SARS, MERS COVID 1-19) during pregnancy a systematic review and meta-analysis. Am J obstet Gynecol MFM. 2020; 100-107. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7104131/
- Monteleone PA, Nakano M, Lazar V, Gomes AP, de H Martin, et al. A review of initial data on pregnancy during the COVID-19 outbreak: implications for assisted reproductive treatments JBRA Assist Reprod. 2020; 24: 219-225. PubMed: https://pubmed.ncbi.nlm.nih.gov/32354663
- Lui H, Wang LL, Zhao SJ, Kwak-Kim J Mor G, Liao AH. why are pregnant woman susceptible to COVID-19? An immunological view point J Reprod Immunol. 2020; 139: 103122. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7156163/
- CDC COVID-19 response team preliminary estimates of the prevalence of selected underlying health conditions among patients with coronavirus disease 2019-united states. 2020. MMWR Morb Mortal Wkly Rep. 2020; 69: 382-386.
- Zaigham M, Andersson O. Maternal and perinatal outcoms with COVID-19: A systematic review of 108 pregnancies Acta obstet Gynecol Sci. 2020.
- Panahi L, Amiri M, Pouy S. Risks of Novel coronavirus in pregnancy; a narrative review. Arch Acad Emerg Med. 2020; 8: e34. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7092922/
- Yan J, Guo J, Fan C, Juan J, Yu XX, et al. Coronavirus disease 2019 (COVID-19) in pregnant women: A report based on 116 cases Am J obstet Gynecol. 2020; 111. e1–111.e14. PubMed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7177142/
- Wu Z, McGoogan JM. Characteristics of and important Lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72314 cases from the Chinese center for disease control and prevention. JAMA. 2020. PubMed: https://pubmed.ncbi.nlm.nih.gov/32091533/
- Liu D, Li L, wu X, et al. Pregnancy and perinatal outcomes of women with coronavirus disease (COVID-19) pneumonia: A preliminary Analysis. AJR Am J Roentgenol. 2020; 1-6.
- Blitz MJ, Grunebaum A, Tekbali A. Intensive care unit admissions for pregnant and non-pregnant women with COVID-19. Am J obstet Gynecol. 2020.
- Zhao X, Jiang Y, Zhao Y. Analysis of the susceptibility to COVID -19 in pregnancy and recommendations on potential drug screening Eur J clin Microbiol infect Dis. 2020; 1-12.
- Pierce-Williams RAM, Burd J, Felder L, houry R, Bernstein PS, et al. Clinical course of severe and critical COVID-19 in hospitalized pregnancies: a US cohort study. Am J obstet Gynecol MFM. 2020; 100134. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/32391519
- Yang Z, Wang M, Zhu Z, Liu Y. Coronavirus disease 2019 (COVIS-19) and pregnancy: a systematic review. J Matern Fetal Neonatal Med. 2020; 1-4. PubMed: https://pubmed.ncbi.nlm.nih.gov/32354293/
- Kasraeian M, Zare M, Vafaei H, et al COVID 19 pneumonia and oregnancy ; a systematic review and meta analysis. J matern Fetal neonatal Med. 2020; 1-8. PubMed:
- Juan J, Gil MM, Rong Z, Zhang Y, Yang H, et al. Effects of coronavirus disease 2019 (Covid-19) on maternal, perinatal and neonatal outcomes: a systematic review. Ultrasound Obstet Gynecol. 2020.
- Zhang L, Jiang Y, Mei M, Cheng BH, Zhou XCN et al. [Analysis of the Pregnancy Outcomes in Pregnant Women With COVID-19 in Hubei Province]. Zhongua Fu Chan Ke Za Zhi. 2020; 55: 166-171. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/32145714
- Alzamora MC, Paredes T, Caceres D, Webb CM, valdez LM, et al. Severe COVID 19 during pregnancy and possible vertical transmission. Am J Perinatal. 2020. PubMed: https://pubmed.ncbi.nlm.nih.gov/32305046/
- Chen H, GuoJ, Wang C, Luo F, Yu X, et al. Clinical characteristics an intrauterine vertical transmission potential of COVID19 infection in nine pregnant women: a retrospective review of medical records. Lancet. 2020; 395: 809-815. PubMed: https://pubmed.ncbi.nlm.nih.gov/32151335/
- Chen S, Huang B, Luo DJ, Li X, Yang F, et al. [Pregnancy With New Coronavirus Infection: Clinical Characteristics and Placental Pathological Analysis of Three Cases]. Zhonghua Bing Li Xue Za Zhi. 2020; 49: 418-423. PubMed: https://pubmed.ncbi.nlm.nih.gov/32114744/
- Chen D, Yamg H, Cao Y, Cheng W, Duan T, et al. Expert consensus for managing pregnant women and neonates born to mothers with suspected or confirmed novel coronavirus (COVID 19) infection. Int J Gynaecol obstet. 2020; 149: 130-136. PubMed: https://pubmed.ncbi.nlm.nih.gov/32196655/
- Elshafgeey F, Magdi R, Hindi N, Elshebiny M, Farrag N, et al. A systematic scoping review of COVID 19 during pregnancy and childbirth. Int J Gynaecol Obstet. 2020; 150: 47-52. PubMed: https://pubmed.ncbi.nlm.nih.gov/32330287/